The clinical ultrasound report: Guideline for sonographers
Abstract
The reporting roles of sonographers in Australasia vary considerably. A large number of sonographers already routinely produce formal reports, while others are moving into clinical ultrasound roles where reporting is expected. This article summarises the best practice in reporting of ultrasound examinations based on international literature and addresses key topics including report structure, clinical content, style and language. Numerous examples and sample phrases are provided and common pitfalls are discussed.
Introduction
Ongoing advances in ultrasound technology coupled with the wide availability of ultrasound and its excellent safety track record have resulted in increased clinical utility of ultrasound technology across all medical specialties and a dramatic rise in the clinical demand for ultrasound1. In this changing healthcare environment, sonographers have long been recognised as experts in ultrasound imaging and are afforded considerable professional respect, autonomy and responsibility.2 The high level of diagnostic accuracy of experienced sonographers (90–99%) has been shown in a number of studies across all subspecialties.3-11 For this reason, sonographers are now increasingly expected not only to perform ultrasound examinations, but to provide a diagnostic interpretation2, 12 and prepare formal written reports.2, 13, 14 While some countries, such as the United Kingdom, have a long tradition of sonographer practice that includes the provision of a formal report13, 15, in Australia and New Zealand, the practice of sonographer reporting varies considerably between individual sonographers and between different departments.16 Although professional organisations such as the Australasian Society for Ultrasound in Medicine (ASUM) and the Australasian Sonographer's Association (ASA) encourage professional progression of sonographers,2, 17 formal stratification of the ultrasound profession into minimally competent sonographers vs. advanced or specialist sonographers is yet to occur.14, 18 As a result, the Australasian sonographer community is composed of a vastly heterogeneous cohort of practitioners, some of who practice at the minimum required level and are not involved in reporting, while others practice at a very high level and formally report all their ultrasound examinations. A survey conducted by the New Zealand Branch of ASUM in July 2011 revealed that 48% of sonographers already prepared formal reports and 20% of sonographers routinely prepared formal reports that were not going to be sighted by a radiologist prior to the report being available to the referring clinician. Indeed, reporting responsibilities of sonographers have been recognised in New Zealand employment contracts for a number of years under the title of ‘reporting sonographer’, ‘specialist sonographer’ or ‘clinical specialist sonographer’.19-21 As the profession of sonography moves into the future, it will be increasingly important for sonographers to acquire proficient reporting skills. The purpose of this article is to provide a detailed overview of the best practice in formal reporting of ultrasound examinations supported by a comprehensive literature review.
The reporting sonographer
A wide range of health practitioners who perform ultrasound examinations are involved in the provision of a diagnostic report. These include sonographers, radiologists and point-of-care practitioners (emergency doctors, general practitioners, subspecialists, midwifes, nurse practitioners, physiotherapists and other healthcare professionals trained in ultrasound).13, 22, 23 The ability to produce quality reports that are accurate, clinically relevant and composed in a clear style is an acquired skill24 requiring familiarity with current reporting standards, clinical experience, mentorship by senior experienced colleagues, practice, peer review and audit.23, 25 Specific instruction in formal report writing, supervised practice and audit should be a part of the sonographer's training. Academic and professional institutions providing ultrasound training programmes must ensure that formal written reporting is incorporated into academic curricula.26, 27 The Central Queensland University already includes written reporting in the Master's level curriculum (email from Dr Aamer Aziz, CQ University, September 2017)28 while the University of Auckland plans to introduce it in the future (email from Associate Professor Jenny Sim, September 2017). Monash University, University of South Australia and Queensland University of Technology do not intend to address reporting in their curricula in the short term (email from Paul Lombardo, Course Convenor Master of Medical Ultrasound, September 2017, email from Associate Professor Kerry Thoirs, September 2017, and email from Chris Edwards, Course Coordinator Medical Ultrasound).
Report structure
There is good agreement in the literature on the structure of an ultrasound report.13, 22, 23, 25, 29-31 In general, an ultrasound report should contain the following sections:
- (1) Title
- (2) Patient identification, demographics, date, recipients, provider details
- (3) Indications: history and clinical information
- (4) Technique and procedural description (when required)
- (5) Findings
- (a) Itemised findings
- (b) Normal and abnormal observations
- (c) Diagnostic comments
- (6) Impression/Conclusion
- (7) Names of the individuals involved in the examination
- (8) Inclusion of reference standards in the footnotes (when required)
Title
Abdominal ultrasound examination
Targeted ultrasound examination of the right groin
Targeted hepatobiliary ultrasound, portable examination in ICU
The term ‘scan’ should be avoided because the assessment of a patient with ultrasound often goes beyond a simple scanning procedure. Unlike other radiology scans, an ultrasound examination involves important elements of clinical interaction between the sonographer and the patient such as history-taking, observation, palpation, dynamic assessment using various manoeuvres, sonopalpation and assessment in different body positions. It is a comprehensive examination, not a scan.
Patient identification, demographics, date, recipients, provider details
It is important that the report is correctly identified by patient's full name, date of birth and one of the following: address, national health identifier, patient clinic identifier, clinic attendance code or other similar identifier.30 The date and time (if appropriate) of the examination should be clearly noted. The sonographer should ensure that the referrer and recipients are acknowledged and that a procedure exists for the recipients to receive the report, whether in electronic or hard-copy form. For external reports, the facility name and contact details should be clearly stated.
Indications: history and clinical information
The patient's history and clinical information may come from a number of sources including:
- history and clinical information provided by the referrer;
- history and clinical information from other medical records;
- information provided by the patient to the sonographer at the time of examination;
- clinical observations made by the sonographer; and
- clinical tests performed at the time of examination.
The patient's relevant clinical history should be copied from the referral and be included in the report. Many patients present with exhaustive medical history including multiple co-morbidities, serial investigations, complex interventions, detailed management plans and extensive medication regimes. It may not be practical (or desirable) to include all of this information in the body of the report.32 In these cases, the sonographer should exercise sound clinical judgement and select the clinical information that is specifically relevant to the ultrasound examination and the clinical question.
A sonographer working in regional or tertiary-level centres may also be able to obtain valuable medical history from other sources including electronic records (admission and discharge summaries, clinic letters, surgical reports, laboratory tests, past imaging investigations) as well as hard-copy notes. Access to medical records may become more universally available in the near future as more patients will choose cloud-based medical records storage.
Prior to commencing the ultrasound examination, the sonographer should:
Review the referral letter
Elicit relevant history from the patient
Review all relevant medical records including:
Laboratory findings
Previous imaging findings and PACS images (if necessary)
Clinic letters
Discharge summaries
Any other relevant medical records available
The sonographer should elicit further relevant information from the patient. The patient's presenting complaint may have changed, or the patient may reveal hitherto undisclosed clinical information that may be helpful in assessing the patient and interpreting the examination.
The patient experiences pain and movement restriction with arm abduction beyond 45 degrees.
All relevant observations should be noted and included in the report and the source of the information acknowledged.30
Technique and procedural description
The inclusion of procedural description and scanning technique is not necessary for most routine examinations such as abdominal or small-parts ultrasound, but can be helpful for specialised examinations such as transvaginal ultrasound, certain vascular examinations, contrast-enhanced ultrasound, marking for bedside drainage and others.35
- Transabdominal and transvaginal ultrasound examinations were performed with patient's consent.
- Contrast-enhanced ultrasound was performed using Definity® perflutren microspheres (number of IV bolus injections: X, total volume of contrast: Xml).
- High-resolution ultrasound assessment of cranial sutures was performed.
- Resting ankle-brachial pressure index (ABPI) was 1.0 bilaterally. The patient was subjected to a 5-min walking challenge on a treadmill set at 10 degrees incline and 3.5 km/h speed.
Findings
Structure
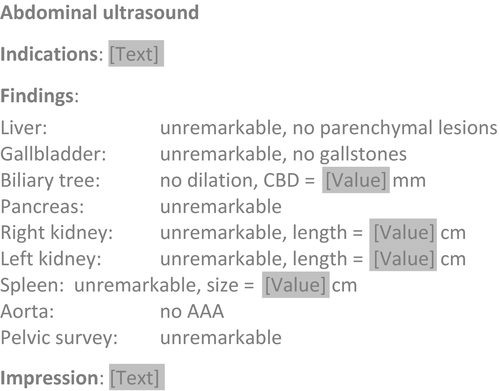
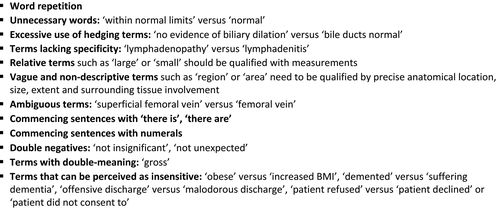
The typical report should present the findings in a logical sequence in the order the examination was performed or in the order of clinical priority. For comprehensive structured examinations, listing specific organs and sites of examination assists in clearly communicating to the referrer what has and what has not been examined (Figure 1).
The right pleural effusion appears simple (not septated) and amenable to percutaneous bedside drainage. A suitable site was marked on patient's skin with a permanent marker. [report end]
Normal and abnormal observations
Segment 8 of the liver contains an irregular thick-walled collection 4.5 × 3.5 × 2.8 cm in size containing particulate contents with fluid-level. The clinical history and imaging findings are consistent with a liver abscess.
Obvious abnormalities with classic and pathognomonic appearance can be referred to directly and do not require a lengthy technical description.36
- The right ovary contains a 4.5 cm simple cyst.
- (Not: ‘The ovary contains a unilocular, round, thin-walled, anechoic, fluid-filled, avascular structure with distal acoustic enhancement, consistent with a simple cyst’.)
- Several gallstones were noted ranging in size from 3 to 6 mm.
- (Not: ‘The gallbladder contains several highly echogenic, rounded, mobile foci with posterior acoustic shadowing characteristic of gallstones, measuring 3–6 mm in size’.)
Incidental findings should be acknowledged37 and worked up. For instance, the incidental discovery of a multilocular solid-cystic mass in a post-menopausal woman presenting for an upper abdominal ultrasound, warrants extending the examination to include a detailed transabdominal and transvaginal scan of the pelvis.
Normal anatomical variants should be reported even if they are of no clinical significance at the time of the examination. Some variants (such as uterine anatomical variants or venous duplications) may become clinically relevant in the future.
- Femoral vein duplication was noted. This is a common normal anatomical variant.
-
Uterus:
size: 7.2 × 4.2 × 5.0, volume: 79 ccs (normal)
orientation: anteverted
morphology: subseptate
Variation from normal protocol
If the examination was extended or reduced in scope, the reasons for this should be acknowledged and justified.13
- Cervix: not examined (term pregnancy)
- The ultrasound features of the liver are consistent with cirrhosis.
- The examination was extended to include Doppler assessment of the mesenteric, portal and hepatic vasculature.
- The findings are in keeping with a right testicular neoplasm. The examination was extended to assess the spermatic cord, regional lymph nodes and kidneys.
- I have informed Mrs Smith about the benefits of performing transvaginal ultrasound to assess the endometrial thickness, however, she declined.
Measurements
Where measurements are provided, it is important to ensure the measurement units are used consistently. For instance, an obstetric report listing a variety of measurements should not mix measurements in centimetres and millimetres.
Fetal biometry:
BPD = 73 mm HC = 271 mm AC = 254 mm FL = 55 mm
EFW = 1383 g ±15%, 45th percentile
Umbilical Artery Pulsatility Index = 0.95 (normal)
Even if a reference chart is embedded in the report, indicating whether a measurement is normal or not can still be helpful in some instances. For example, if the fetal Middle Cerebral Artery Pulsatility Index lies above the 95th percentile on a reference chart, it may appear to be outside the normal limits; however, the measurement is only defined as abnormal if it is below the 5th percentile.39
Comparison with prior studies
Comparison was made with CT dated dd/mm/yyyy. The small indeterminate lesion noted in segment 7 represents a simple cyst measuring 6 mm in diameter.
Direct comparison is particularly important in the cases of surveillance where the sonographer is investigating the patient for the presence of interval change. The presence or absence of change should be clearly stated.40, 41
- The previously noted small echogenic liver lesion is unchanged when compared to previous ultrasounds performed 6 and 18 months ago.
- The previously noted 4.5 cm AAA remains unchanged. Routine surveillance in 12 months’ time has been arranged as per departmental guideline.
Prior ultrasound examinations performed at [clinic, city] on dd/mm/yyyy are not available for direct comparison. Comments regarding interval change cannot be made.
Sonopalpation
Apart from the performance of the ultrasound scan, sonographers also have the ability to clinically examine the patient with the transducer (sonopalpation) and observe important physiological or pathological changes with various clinical manoeuvres or in different patient positions. These observations can provide further clinical information. It can be valuable to include these findings in the body of the report:
- The left ovary and left adnexa are not tender on application of transducer pressure. Gynaecological cause for LIF pain is therefore considered unlikely.
- Impingement of the supraspinatus muscle is seen beyond 45degree abduction
- The area of pain directly corresponds to a cluster of reactive, but morphologically normal inguinal nodes. The findings are consistent with lymphadenitis.
Examination quality
To what degree comments regarding the image quality are helpful to the recipient of a diagnostic report is debatable, however, significant technical shortcomings that may affect the interpretation of the examination need to be acknowledged.22, 25, 29, 30 On the other hand, excessive hedging is generally considered unhelpful because clinicians may not understand the degree to which the results can be relied on.42 For instance, making a comment that ‘examination of the liver is suboptimal due to increased BMI of the patient, however no obvious liver mass was detected’ may leave the referring clinician questioning whether (a) there is no liver mass or (b) a liver mass was not detected because it was not detectable to begin with.
If the quality of the examination significantly impairs the sonographer's diagnostic confidence or the examination is non-diagnostic, these considerations should be disclosed. Whenever possible, suggestions on how to achieve a diagnostic result should be offered.
- Assessment of the liver with ultrasound is non-diagnostic due to technical limitations associated with high BMI. Given the background of Hepatitis B and rising AFP, consideration should be made for other cross-sectional imaging.
- Fetal heart and face anatomy cannot be assessed due to unfavourable fetal position. Repeat ultrasound in 1 weeks’ time is recommended in order to complete fetal morphology assessment.
- Adequate transabdominal and transvaginal ultrasound examinations of the pelvis cannot be achieved because the patient is experiencing severe pain and cannot tolerate the examination. The examination was abandoned. Transvaginal pelvic ultrasound may be achievable under light sedation. Please contact our team on extension ×1234 to discuss.
Dealing with complex findings
Sonographers, like all health care professionals using ultrasound (radiologists, point-of-care practitioners, emergency doctors and others), may not have the full spectrum of expertise in all subspecialties of ultrasound. For this reason, sonographers should resist the temptation to provide specific diagnoses in areas that lie outside their areas of expertise. For instance, a sonographer working in a private centre may be highly proficient at performing fetal morphology scanning, but may not be skilled in the performance and interpretation of fetal echocardiography. In case of an incidental discovery of a complex congenital heart anomaly, it may be more appropriate to (a) withhold specific diagnostic comments, (b) report that ‘the examination of the fetal heart raises the suspicion of congenital heart abnormality’ and (c) refer the patient to a tertiary-level fetal medicine unit for formal echocardiography where the full range of relevant diagnostic comments can be rendered in a format required by the subspecialist paediatric cardiology team.
Fortunately, sonographers most often work as part of a team in a clinic or hospital setting. Such environments offer abundant opportunities for consultation with colleagues in solving complex imaging problems.
Impression/conclusion
Impression:
1 Acute calculous cholecystitis
2 No biliary dilation
3 Fatty liver
4 Simple cyst in the left lobe of the liver
Impression:
The findings are strongly suggestive of ruptured right-sided ectopic pregnancy. Incidental note was made of a simple left ovarian cyst. The patient was immediately transferred to the Emergency Room following the examination.
Formulating a summary
The terms ‘impression’, ‘conclusion’ or ‘summary’ are preferred to ‘diagnosis’.32 As a matter of reading efficiency, many clinicians have a tendency to skip the body of the report and refer immediately to the conclusion.25 For this reason, the conclusion should provide a clear and concise summary of the report. In routine examinations, the summary can be brief.
- Normal abdominal ultrasound. No cause for RUQ pain was identified.
- Interval fetal growth has been normal.
- Unremarkable ultrasound examination of the right shoulder.
In other cases, it may be appropriate to state whether the findings are benign or concerning.
- Occasional premature atrial contractions were noted. These represent a benign fetal arrhythmia which typically resolves spontaneously. Further imaging is not required unless CTG or bedside Doppler examination raises the possibility of supraventricular tachycardia.
- The presence of multiple target lesions in the right lobe of the liver is highly concerning for the presence of metastases.
It is acceptable for brief reports not to have a conclusion.25, 30, 31
Clinical interpretation
The fetal kidneys and bladder are clearly visualized. The fetus is normal in size. Although the mother reports no fluid loss, premature rupture of membranes is the most likely cause for anhydramnios.
The palpable scrotal lump corresponds to a simple epididymal cyst. There is no testicular mass.
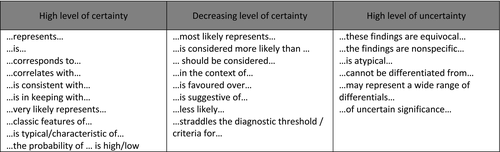
If this is not possible, clinically realistic differentials should be provided and appropriately ranked in terms of probability or clinical priority (Figure 2).13, 22
The cause for biliary dilation is not visualized. Given the acute presentation with pain and jaundice combined with the presence of gallstones in the gallbladder, choledocholithiasis is considered highly likely. The pancreas was well visualized and appears normal. Ampullary-level pathology while less likely cannot be excluded by ultrasound alone.
The palpable axillary lump represents an enlarged and morphologically abnormal lymph node that demonstrates multiple concerning features including: loss of normal hilar pattern, rounded shape, asymmetry in parenchymal thickness, microlobulated margins and zones of hypoperfusion.
Right testis: length = 4.5 cm, volume = 14.5 ccs (normal), colour Doppler perfusion: normal
Testicular torsion has been excluded.
Findings of no or little clinical significance should be acknowledged as such with appropriate qualifying comments.32, 41, 45
- Two small gallbladder polyps were noted measuring 2 and 3 mm in size. These are of no clinical significance and do not require further follow-up.
- In isolation, choroid plexus cysts represent a benign finding and no further assessment is required.
The sonographer should ensure the report directly addresses all clinical questions raised in the referral.13, 25, 29, 30, 34 Furthermore, the sonographer should also anticipate clinical questions that were not explicitly stated on the referral.43 In some cases, stating the absence of specific findings can reassure the clinician by emphasising that sufficient attention has been paid to the region of concern.
- The cause for RIF pain was not identified on transabdominal or transvaginal ultrasound. Specifically, there is no evidence of gynaecological abnormality, appendicitis or urolithiasis.
- No anatomical cause for menorrhagia identified. Specifically, no endometrial thickening, polyp or fibroid was detected.
Although the patient reports acute onset of left testicular pain following a sporting injury, the ultrasound findings are strongly suspicious for testicular malignancy instead. There is no sonographic evidence of trauma.
Finally, in formulating diagnostic comments the sonographer should be aware of his/her level of competence. Sonographers should exercise a judicious threshold for seeking advice or a second opinion from a senior colleague such as an expert sonographer, radiologist or sonologist, particularly in cases requiring a multimodality approach to reach the diagnosis.13
Recommendations (further testing, surveillance, referral, treatment)
The conclusion may also include recommendations for further testing, surveillance, referral, treatment and other considerations that may assist the referrer in managing the patient. Adherence to evidence-based practice principles is especially important. In many instances, the sonographer can refer to established local, national or international guidelines in making recommendations:36, 46-54
- No evidence of intrauterine or ectopic pregnancy was detected. This is a pregnancy of unknown location (PUL). Clinical monitoring and serial bHCG are recommended. Repeat transvaginal ultrasound can be offered when bHCG reaches 1000 iu/l or if the patient's clinical presentation changes.
- The finding of absent end-diastolic flow in the umbilical artery in a 28-week fetus is highly concerning and immediate specialist obstetric opinion is advised.
- Incidentally detected simple asymptomatic ovarian cysts less than 5 centimetres in diameter in premenopausal women generally do not warrant further surveillance.48
AAA surveillance in 6 months is recommended. I have made a booking for a repeat ultrasound in the Vascular Laboratory on dd/mm/yyyy.
As a final step in the preparation of the report, the sonographer should confirm that all clinical questions have been addressed.
Action taken
In special circumstances such as when findings of unexpected or urgent nature arise, the action taken should be recorded in the report.13
- I have informed Mrs Smith that she has a significant deep vein thrombosis and I have arranged for her to be transferred to the emergency room for review.
- In view of the urgent nature of the findings, I have discussed the results with Dr T Smith, urology registrar by telephone.
- Ultrasound confirms clinical suspicion of a large AAA measuring 7.4 cm in maximum AP diameter. I have arranged immediate consultation with Dr J Smith, vascular consultant.
Names of the individuals involved in the examination
Examination performed by: Jane Smith, trainee sonographer
Supervised by: John Doe, clinical specialist sonographer
Discussed with: Kathy White, radiologist
Inclusion of reference standards
*Grading of renal pelvis dilation and management comments are based on New Zealand National Antenatally Detected Asymptomatic Renal Dilation consensus group statement 2017.
Postnatal grade N (Normal) = AP Renal Pelvis Diameter <10 mm, no peripheral dilation
Follow-up recommendation:
Normal scan before 1 month age – repeat in 3 months
Normal scan after 1 month age – no further follow-up
The inclusion of a reference standard may also be useful where multiple standards for the interpretation of the same finding could be used by different ultrasound providers and the application of different standards may influence the final result.53-56
- British Thyroid Association (BTA) classification (2014) was used for ultrasound nodule characterisation.
- The interpretation of carotid artery stenosis was made according to Joint recommendations for reporting carotid ultrasound investigations in the United Kingdom (2009).
Report style and language
Length and detail
The ultrasound report needs to strike a balance between conciseness and sufficient clinical detail.32, 44, 57, 58 The sonographer should have a thorough understanding of what information is relevant to the referring clinician and tailor the report accordingly by prioritising clinically important observations.
Structured reports vs. narrative/prose reports
Clinicians tend to prefer structured, itemised reports rather than prose reports written in a narrative form.24, 25, 44, 57, 59
-
An example of a wordy narrative statement:
The right kidney is normal in size, shape and echotexture, measuring 10.5 cm in craniocaudal length. The renal parenchyma demonstrates normal thickness and echotexture. No masses, stones or hydronephrosis were detected.
-
The same information provided in a concise, structured format:
Right kidney: 10.5 cm length, normal
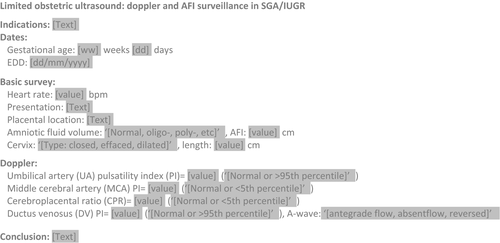
Structured reports also enable easier comparison with prior reports because the information is always presented in the same expected location and the same format. Ultrasound providers should strive to develop structured and consistent reporting styles that address the needs of the referrers.60, 61 Seeking input from the referrers in the development of report templates can ensure that the report meets the referrer's expectations62 (Figure 3). A range of report samples and templates are available online.13, 23, 63
Although itemised reports are preferred, occasionally, a brief narrative report may be more appropriate for examinations of targeted nature.
- Targeted Ultrasound Right Dorsal Wrist
- Indications: 53 year old man, T2DM, cellulitis over dorsum of right wrist, ? Joint effusion, ? Septic arthritis, ? Underlying collection
- Findings: High resolution ultrasound was performed. The area of redness and swelling involving the dorsal wrist demonstrates a unilocular subcutaneous abscess measuring 52 × 47 × 9 mm with an approximate internal volume of 11.5 ccs. The distance from the skin surface to the centre of the abscess is 10 mm.
- Conclusion: Subcutaneous abscess amenable to percutaneous drainage.
The sonographer should be mindful that highly specialised reports that are commonly understood in a subspecialist or inpatient setting may need to be tailored or presented in such a way that they are understandable to recipients working in an outpatient or primary-care setting.13
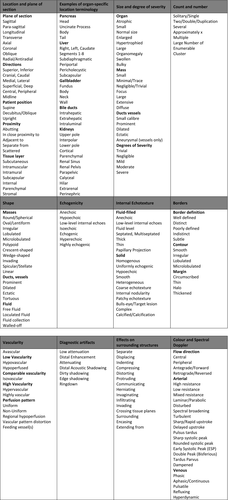
Terminology
The language style should be formal, clear, concise, specific, unambiguous and easily understood by a wide variety of recipients ranging from subspecialists to GPs and other health care professionals involved in the care of the patient.13, 41, 64 Increasingly, reports are also read by patients.41, 65 The sonographer should refer to established guidelines or lexicons and adhere to widely accepted formal terminology.36, 49-52, 66-68 Nonspecific or ambiguous terminology should be avoided. For instance, the term ‘complex’ should never be used to describe findings in the ovaries as the term is ambiguous and may refer to appearance that range from normal (haemorrhagic cyst) to malignant (ovarian cystadenocarcinoma).
The description of normal appearances usually involves the terms ‘normal’, ‘unremarkable’, ‘no sonographic abnormality’ or ‘no abnormality detected’. While some authors prefer the more definitive term ‘normal’,69 it is important to recognise that an absence of abnormality does not necessarily ensure that the organ in question is normal in all respects. For instance, a patient presenting for a hepatobiliary ultrasound with deranged LFTs due to acute hepatitis will most likely demonstrate normal sonographic appearance of the liver. It would be incorrect to state that the ‘liver is normal’. The liver is certainly not normal. It would be accurate to state that ‘the ultrasound appearance is normal’ or ‘no anatomical cause for deranged LFTs was noted’ or that the liver ‘appears sonographically unremarkable’. Figure 4 contains a sample of commonly used descriptive ultrasound terminology.
‘A 4 cm solid, heterogeneous, vascularised renal mass in the interpolar region of the left kidney was detected likely representing a renal cell carcinoma’.
In other instances, the sonographic appearance may represent a wider range of pathologies and broader, more inclusive terminology is appropriate.
- The solid hypoechoic heterogeneous testicular mass is concerning for malignancy (rather than ‘seminoma’)
- The uniformly echogenic lesion in the fetal chest most likely represents a congenital pulmonary airway malformation’ (rather than ‘Type 3 cystic adenomatoid malformation)
The report should be written in a clear and specific style. A sample of common stylistic and wording errors and pitfalls is provided in Figure 5.25, 32
Writing in first person may demonstrate compassion and add a nice personal touch to an otherwise formal and impassive report.
- I have explained to Jenny and her husband that a further scan will be necessary to complete the fetal anatomy assessment and have arranged for them to return in 1 weeks’ time.
- ‘I have discussed the results of the carotid Doppler examination with Mrs Smith and reassured her about the absence of carotid artery disease’.
Abbreviations
The use of abbreviations is discouraged as they can be ambiguous or unfamiliar to the report recipient.70 Consider that the largest online database of pharmaceutical and medical abbreviations (MediLexicon)71 contains over 230 000 abbreviations. For instance, the abbreviation ‘AML’ has 7 potential uses ranging from description of normal anatomy (anterior mitral leaflet), benign renal neoplasm (angiomyolipoma) through to sinister haematological malignancy (acute myeloid leukaemia).
The anterior accessory saphenous vein (AASV) is also incompetent and becomes varicose 20 cm below the groin crease. The AASV is amenable to thermal ablation.
Consistency
For instance, the following three descriptions were provided for the same stable patient with long standing cirrhosis due to autoimmune hepatitis presenting with no interval change over a three-year period:
Year 1: ‘The liver size, shape and echotexture is normal’.
Year 2: ‘The liver appears as expected for known history’.
Year 3: ‘Liver texture unremarkable, no nodularity, minor volume redistribution with increased bulk of the left lobe, no evidence of portal HTN’.
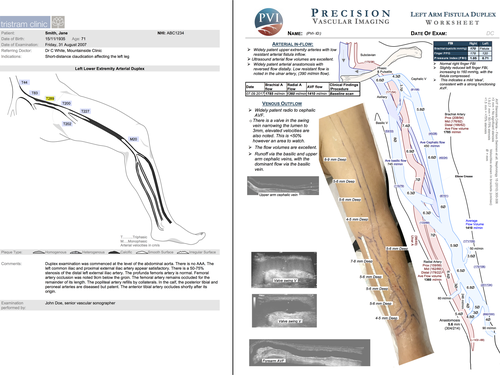
Graphical reports
Graphical reports include supplementary diagrams to better communicate the findings of the ultrasound examination. These types of reports have been commonly used in vascular laboratories because vascular surgeons show a strong preference for diagrams rather than plain text34 (Figure 6). Another type of graphical report that may become more widespread in the future is the image-rich radiology report. Such a report contains a selection of images with annotations.72
Accountability
An ultrasound report is a formal document and represents an important waypoint on the management pathway of the patient. Sonographers therefore have the responsibility to ensure the report is accurate in every respect and is prepared and available as soon as possible, ideally immediately after the examination has been completed.13 There are obvious clinical, professional and medicolegal risks if the report is inaccurate, incomplete or delayed.25, 73-76
Proofreading
The report needs to be carefully proofread to avoid errors in content, spelling and grammar.13, 77 Errors can range from minor embarrassments due to misspelling or word substitution,25 to serious errors concerning the opposite meaning (‘avascular’ vs. ‘a vascular’) or wrong side (‘left’ vs. ‘right’).
Conclusion
Formal reporting is an important professional skill for sonographers, radiologists, sonologists and point-of-care practitioners. Many sonographers already fulfil reporting roles and are recognised for such roles in employment contracts. This article provides a detailed summary of current best practice taking into account existing guidelines and published literature. The reporting strategies and examples provided in this article can serve as vignettes that the sonographer can implement to enhance his or her own reporting style.
Acknowledgement
The author would like to thank the following colleagues for their review of the manuscript, advice and support: Dr Sue Campbell Westerway, Kathryn Busch (Sydney) Debra Paoletti, (Canberra); Peter Coombs, Paul Lombardo, Dr Aamer Aziz, Suean Pascoe (Melbourne); Deb Coghlan, Sue Davies, Christopher Edwards (Queensland); Laura Lukic (Adelaide); Dr Chhaya Mehrotra, Michelle Pedretti (Perth); Dr Kate Thomas, Jill Muirhead, Gerry Hill (Dunedin); Rex de Ryke Christchurch, Josie MacFarlane, Wendy Parker (Christchurch); Angela Browne, (Whangarei); Dr Melissa Haines, Dr Thodur Vasudevan, Dr Cristina Zollo, Nicole Curtis, Bridget Boyle, Fei Yuan, Karen Robertson, Jo McCann, Dr Kara Prout, Sarah Martinez (Hamilton); Carol Bagnall, Scott Allen, Alan Williams, Mike Heath, Sangeeta Kumar, Dr Christina Tieu (Auckland); Dr Barbara Loeliger (Thames); Brendon Cosford, Sally Shaw (Tauranga); Rowena Tyman (Napier); Elaine Hampton (Whanganui); Ruth Tuck (Whangarei); Bridget Sparks (Gisborne); and Jonathan Meredith (Wellington).
Conflict of interest
No disclosures or conflicts of interest to declare.




