A review of endophenotypes in schizophrenia and autism: The next phase for understanding genetic etiologies
Abstract
Many psychiatric disorders are caused by multiple genes and multiple environmental factors, making the identification of specific genetic risk factors for these disorders difficult. Endophenotypes are behaviors or characteristics that are intermediate between the genotype and a phenotype of interest. Because they are more directly related to the gene action than is the endpoint disorder, they may be useful in the identification of specific genes related to psychiatric disorders and the classification of disorders or traits that share an underlying genetic etiology. We discuss genetic and endophenotype research on schizophrenia and autism spectrum disorder (ASD) in this review. Some of the psychophysiological endophenotypes that have been studied for schizophrenia include prepulse inhibition of the startle response, the antisaccadic task assessing frontal lobe function, inhibition of the P50 event-related potential (ERP), and other auditory ERP measures. Potential ASD endophenotypes include theory of mind, language skills (specifically, age at first spoken word and first spoken phrase), social skills, and certain brain functions, such as asynchronization of neural activity and brain responses to emotional faces. Because the link between genes and specific psychiatric disorders is difficult to determine, identification of endophenotypes is useful for beginning the search to identify specific genes that affect these disorders.
1 INTRODUCTION
We have come a long way from the early days of believing in the “schizophrenogenic” mother in our studies of the etiology of schizophrenia and autism. The cold, detached, and unloving behaviors of these mothers were believed to be the cause of their children's eventual autism or schizophrenia diagnoses. We now know, through multitudes of twin, adoption, and molecular genetic studies, that genes as well as environmental experiences are important contributors to these psychiatric disorders. In addition, we have learned that there is no single gene and no single environmental influence responsible for engendering the onset of these disorders. Rather, these complex disorders are multiply determined through exquisitely complicated combinations of both genetic and environmental risk factors (Gottesman, 1991). As we attempt to understand better the genetic underpinnings of these disorders and the ways in which other related spectrum disorders or behaviors might be connected to schizophrenia and autism, it is valuable to consider characteristics that occur intermediate between genes and the behaviors or disorders of interest. These interim characteristics have been termed endophenotypes.
Irving Gottesman and James Shields were the pioneers who first introduced the concept of the endophenotype to the psychiatric and medical literature (Braff & Tamminga, 2017; DiLalla & DiLalla, 2017; Gottesman & Shields, 1967). Although the term originally came from the biological sciences, Gottesman clarified it for psychologists as information about an individual that cannot readily be seen and that is intermediate between the genotype and the psychological phenotype of interest (Gottesman, 1991; Gottesman & Gould, 2003). It is essential to understand that most psychological phenotypes (observable, measurable characteristics) are influenced by multiple genes and multiple environmental factors. Thus, identification of specific genes that influence any psychiatric disorder is incredibly complicated. Although there is no clear path to the development of a psychological disorder, the identification of possible contributing genes may have important implications for medical/psychological prevention and intervention. For this reason, identification of endophenotypes that augment our understanding of how specific genes may impact behaviors, or at least help to identify some of the genes in the equation, is clearly a valuable avenue of study.
Endophenotypes hold enormous promise for the study of psychiatric disorders because they may be used to help identify some of the underlying genetic influences on these disorders. Because endophenotypes are biologically closer to the actual gene expression than are the psychological disorders, they should be advantageous for pinpointing specific genotypes that may be related to the disorders (Liu et al., 2016; McGue, 2010). Endophenotypes must be associated with the disorder (Gottesman & Gould, 2003) and may potentially be one facet of the disorder (El-Fishawy, 2013). As a hypothetical example, the action of a particular dopamine receptor gene might lead to a specific tic. If many people with psychiatric disorder X also evidence that specific tic, then that dopamine receptor gene might be one of the genes affecting the expression of disorder X. It also would be likely that non-affected family members might show the same tic by virtue of sharing that particular dopamine receptor genotype with the affected individual. Similarly, they may express sub-threshold symptomatology that stems from this dopamine receptor gene, but might not meet full diagnostic criteria for disorder X due to their genotype or environment. In this example, the tic would be an endophenotype for disorder X. The tic may not be a symptom of the disorder, but it frequently co-occurs because the genes that affect the disorder also directly affect the tic behavior. Understanding the genetic influence on the tic would provide important information about some of the genetic etiology of the disorder.
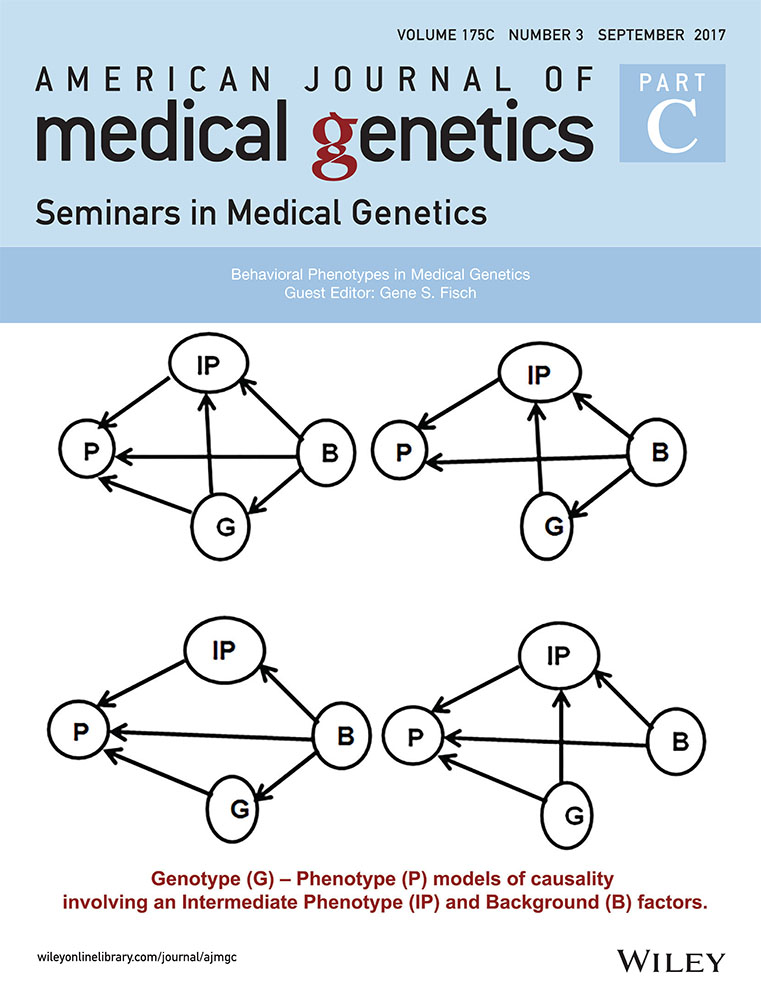
One problem with identifying endophenotypes is the probability that the effect sizes of genetic influence on endophenotypes are quite small, comparable to the effect sizes for the psychiatric disorder itself (Flint & Munafo, 2007), making the genetic influences on the endophenotypes equally difficult to identify. If this is correct, then identifying endophenotypes may not in fact be particularly beneficial for discovering genes related to the actual disorders of interest. One recent study suggested that enormous samples are needed to identify underlying genes causally related to endophenotypes (Liu et al., 2016). Additionally, correlations between genotypes and endophenotypes are not necessarily indicative of causality (Kendler & Neale, 2010), and thus we must be careful to consider direction of effects as well as the role of environmental influences as we search for genetic effects on both endophenotypes and psychiatric disorders.
1.1 Use of endophenotypes
The study of endophenotypes is important in a number of ways. First, it may lead to a better understanding of the genetic mechanisms underlying a particular behavior. Second, identification of particular endophenotypes may provide a means for the identification of family members who are at increased risk for a genetically influenced disorder. Third, by identifying endophenotypes, we may become able to better design medications and interventions that could either alleviate symptoms or prevent a disorder altogether. It may become possible to better tailor interventions (medical as well as behavioral) on the basis of the presence or absence of particular endophenotypes, because that would provide evidence of whether a specific genotype is part of the constellation of factors responsible for a disorder in a given individual (Bakermans-Kranenburg, van IJzendoorn, Pijlman, Mesman, & Juffer, 2008; DiLalla & Bersted, 2015). Thus, theoretically, the study of endophenotypes should be able to move forward the study of both schizophrenia and autism in a major way. However, there is still much work to be done before these benefits are realized.
In addition to helping us better understand genetic causes of a disorder and inform treatment, identification of endophenotypes may also lead to a greater understanding about the spectrum nature of certain disorders. Understanding etiology is not the only reasonable way to categorize disorders; using clinical symptoms to derive disorder definitions also can be useful for clinicians. However, if we find that a number of psychiatric disorders share a common endophenotype, then it is reasonable to consider that they have a shared etiology and may belong together in a diagnostic category. Endophenotypes have been used nosologically in refining diagnoses (Stein, Lund, & Nesse, 2013) for the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013) and International Classification for Disorders 10 (ICD-10; World Health Organization, 2016), although many identified endophenotypes are proving to be quite complicated constructs by themselves. Nonetheless, the study of endophenotypes may provide information that etiologically ties together disorders that previously have been purportedly disparate (El-Fishawy, 2013). This also has important implications for family members of someone with a psychiatric disorder. For instance, if an endophenotype is discovered for schizophrenia, then it is likely that family members of someone diagnosed with schizophrenia will share the endophenotype even if they do not share the diagnosis. This information may be useful for genetic counseling of family members when considering their own risk for the disorder as well as possible risks for their current or potential offspring.
Endophenotypes specifically related to the psychiatric disorders of schizophrenia and autism have been studied by many researchers over the past decade. The nature of these disorders, specifically in terms of the spectrum of related disorders for each, makes them ideal candidates for the examination of endophenotypes. Below we define each disorder, and then we discuss evidence for endophenotypes for each of them.
2 SCHIZOPHRENIA
Schizophrenia is perhaps one of the most well-known disorders in the field of psychology and can be one of the most debilitating mental health disorders. Schizophrenia tends to appear later in life, during late adolescence for men and early adulthood for women (Andreasen, 1995). Despite the different age of onset, it is one of the few disorders that appears to affect both men and women at similar rates (WHO, 2016). The criteria used to diagnose individuals have been derived from clinical symptoms and require more than the presence of purely psychotic symptoms.
The ICD-10 and DSM-5 are the two most prominent classification systems used to diagnose individuals with schizophrenia (APA, 2013; WHO, 2016). Although different, these classification systems incorporate many of the core components commonly associated with schizophrenia, including the presence of both positive and negative symptoms (APA, 2013; WHO, 2016). Positive symptoms include experiences that are not present in typically developing individuals (e.g., psychosis), whereas negative symptoms are defined as the absence of core characteristics that impact the individual's ability to function in everyday life (e.g., blunted affect; Andreasen, 1995). Although “first-rank Schneiderian symptoms” such as delusions and hallucinations are not sufficient for a diagnosis of schizophrenia, they are more severe in individuals with this diagnosis and are commonly associated with poorer outcomes (Rosen, Grossman, Harrow, Bonner-Jackson, & Faull, 2011).
Schizophrenia is a polythetic disorder, meaning that it is often characterized by the presence of numerous disturbances in functioning and cognition as opposed to a single necessary criterion (Andreasen, 1995). Due to the nature of this disorder and plethora of characteristics needed for its diagnosis, the exact cause of schizophrenia historically has been a source of great controversy. Initially, researchers assumed that schizophrenia was not heritable due to its lack of consistency with traditional Mendelian genetic patterns (Gottesman & Shields, 1967). In the early 19th century, the zeitgeist and prominent psychological orientations pointed to an environmental explanation of schizophrenia (Neill, 1990). Before the 1980s, it was commonly believed that schizophrenogenic mothers were to blame for the development of schizophrenia in their children (Harrington, 2012). It was not until the deinstitutionalization of the seriously mentally ill and emergence of the biological approach that psychologists began to consider a potential heritable component to this disorder (Harrington, 2012).
Irving Gottesman initially proposed that schizophrenia most likely had a polygenetic source largely exacerbated by stressful environments (Gottesman & Shields, 1967; McGuffin, Farmer, Gottesman, Murray, & Reveley, 1984). Since that time, numerous studies have identified multiple genetic and environmental risk factors for schizophrenia. Twin studies have found higher concordance rates of schizophrenia in monozygotic (MZ) twins when compared with dizygotic (DZ) twins, indicating that genetic factors likely play a role in its development (Kläning et al., 2016).
More recently, there have been more than 100 genomic loci implicated in the development of schizophrenia using GWAS (genomic wide association studies) methodology (Ripke et al., 2014; Srinivasan et al., 2016), although no specific genes have been pinpointed as necessary or sufficient for its development. Much research from consortiums such as the Consortium on the Genetics of Schizophrenia (COGS) and Psychiatric Genomics Consortium (PGC) appear to converge on glutamate as one critical neurotransmitter impacting schizophrenia symptoms and related endophenotypes, thus implicating genes related to glutamate (e.g., NRG1, ERBB4) as likely candidates for partial contributors to these symptoms (Braff, 2015). One large GWAS study noted significant effects of protein-coding Transcription Factor 4 (TCF4) and Neurogenic Locus Notch Homolog Protein 4 (NOTCH4), which are consistent with other studies, as well as a number of other SNPs related to functions such as immune response and neuronal signaling (Aberg et al., 2013). Additionally, de novo mutations have been demonstrated to be important for certain aspects of schizophrenia (Braff, 2015). Certain rare deletions, which are more difficult to identify, have been noted as related to schizophrenia as well (Greenwood et al., 2013). Despite the identification of many possible risk genes, more research is needed to determine the functionality of these genes and circumstances under which they may lead to the development of schizophrenia (Bray & Hill, 2016).
Although overwhelming evidence suggests that schizophrenia is a disorder of genetic and environmental origins, there is still much work to be done to better understand its etiology and causes. The diathesis-stress model suggests that the presence of a stressful environment may cause schizophrenia in individuals with certain genetic risk factors, and this has largely been supported (Gottesman & Shields, 1967). Factors such as childhood abuse or neglect (Àlvarez et al., 2015), birth complications, prenatal environment, social adversity, and numerous others continue to be identified as possible risk factors for schizophrenia (Harper, James, & MacCabe, 2015). Researchers from one study found that the differences in genomic makeup from Neanderthals to Homo Sapiens may be partly responsible for the etiological underpinnings of schizophrenia, indicating that this disorder may be a byproduct of the development of human language and creativity (Srinivasan et al., 2016). Furthermore, behavioral genetic studies on schizophrenia point to a possible genetic liability that is shared with a variety of psychotic disorders, supporting a threshold model (Kläning et al., 2016). Research such as this allows for the identification of genetic makeup in combination with specific environmental risk factors and is important for the accurate identification of causal factors. It would be valuable to be able to identify both environmental risk factors and individuals’ specific genetic risk because this could lead to more accurate identification and effective treatment. Due to the polythetic nature of this disorder and complexity identifying specific risk factors, this research also provides possible avenues of exploration for related endophenotypes.
3 AUTISM SPECTRUM DISORDER
Autism spectrum disorder (ASD) is classified as a neurodevelopmental disorder in the DSM-5 (APA, 2013). Previous diagnoses of autistic disorder, Asperger's disorder, and childhood disintegrative disorders have been incorporated into the overarching disorder of ASD to reflect a more dimensional or spectrum view of the characteristic symptoms of ASD (Wakefield, 2013). This new spectrum approach is meant to signify differences in the severity and presentation of symptoms among individuals with ASD (Lai, Lombardo, Chakrabarti, & Baron-Cohen, 2013). ASD is considered a lifespan disorder, meaning that symptom onset presents in the early developmental period, and the symptoms persist throughout the lifespan (Klinger, Dawson, Barnes, & Crisler, 2014).
There are two core symptom categories that characterize individuals with ASD: (1) deficits in social communication and interaction abilities across multiple contexts; and (2) restrictive and repetitive behaviors and interests (Lai et al., 2013). Deficits in communication abilities may be nonverbal (e.g., poor eye contact, atypical body language, and gestures) and/or verbal (e.g., pronoun reversal, echolalia) in nature (APA, 2013). Examples of social communication deficits include failing to respond to social interactions, inability to share a focus of attention with others, and inability to engage in imitation and pretend play (Klinger et al., 2014). Individuals with ASD may also have difficulty developing, maintaining, and understanding social relationships. Restricted, repetitive patterns of behavior may be in the form of stereotyped or repetitive motor movements, use of objects, or speech (APA, 2013). Symptoms from this domain also include rigid adherence to routines, extremely circumscribed interests, and over- or under-reactivity to sensory stimuli.
Despite ASD's classification as a neurodevelopmental disorder, there are currently no medical tests or biological markers that can be used to diagnose ASD (Lai et al., 2013). However, much genetic research shows that the likelihood of an individual being diagnosed with ASD increases if a related family member also is affected by the disorder (Bourgeron, 2016). Specifically, twin studies have shown ASD concordance rates ranging from 60% to 96% in MZ twins and from 0% to 23% in DZ twins, suggesting that genes may play a major role in the development of ASD (Klinger et al., 2014).
Some research has suggested that a “broader autism phenotype” exists, in which relatives of individuals with ASD may not be affected by the disorder itself, but instead may exhibit a “lesser variant” that is influenced by shared genes (Baron-Cohen & Hammer, 1997). Traits of ASD, such as communication deficits, social skills deficits, and restrictive interests, may be found in approximately 4–20% of first-degree relatives of individuals with ASD (Klinger et al., 2014). Evidence for a broader autism phenotype supports the role of genes in contributing to the development of ASD and also pinpoints possible areas of study for endophenotypes.
There is no current evidence for a single genetic mutation that leads to the development of ASD. Rather, as with schizophrenia, there may be multiple genetic as well as environmental pathways that contribute to its development (An & Claudianos, 2016). Much of the research on genetic factors related to ASD has focused on common DNA variants and genetic alterations in the DNA nucleotide sequence. Common variants may account for approximately 40% of the genetic risk for ASD (An & Claudianos, 2016). Multiple variants of known risk genes (e.g., SHANK2, SHANK3, and neuroligin 4 [NLGN4]) and chromosomal loci (e.g., 15q11-13 and 16p11.2) can influence the presentation of ASD and its severity (Abrahams & Geschwind, 2008). Additionally, new research has identified some rare inherited genetic variants that are implicated in ASD (Krumm et al., 2015). These rare variants appear to be inherited most often from mothers to sons. Three rare inherited candidate genes identified by Krumm et al. (2015) include Regulating Synaptic Membrane Exocytosis 1 (RIMS1) and Centromere Protein J (CENPJ), both of which have been shown to be related to cognitive function, and Leucine Zipper Like Transcription Regulator 1 (LZTR1). We have yet to better understand why these particular genes affect ASD symptoms. Current research suggests that most of these may predispose a child toward ASD, but they certainly are not sufficient to cause the disorder.
Studies have also shown that some ASD cases may be explained by observable genetic mutations or de novo copy number variants (CNVs; Bourgeron, 2016). However, duplications and deletions of specific chromosomal regions account for a small percentage of ASD cases with a known genetic cause (Klinger et al., 2014). De novo CNVs may also be common risk factors in sporadic, rather than familial, cases of ASD (Bourgeron, 2016). Research suggests that CNVs may directly lead to ASD development or may increase genetic susceptibility when combined with common variants (Abrahams & Geschwind, 2008). It should also be noted that identified risk genes and mutations are not specific to ASD. Rather, they are implicated in a range of ASD symptoms, such as language difficulties, as well as other similar disorders (Klinger et al., 2014).
Development of ASD may also be influenced by the interaction of genetic factors with environmental factors. Gene-dosage models suggest that the cumulative risk of both genetic and nongenetic factors interact to produce ASD (Abrahams & Geschwind, 2008). Research has shown that prenatal environmental conditions may affect the development of ASD, in that maternal infection during pregnancy has been linked to social communication difficulties in children with ASD-associated CNVs (Vijayakumar & Judy, 2016). Other environmental factors that have been proposed to interact with risk genes include preterm birth, folate deficiency, and exposure to certain toxins (Vijayakumar & Judy, 2016). Epigenetic factors may also increase risk of ASD. One model suggests that older paternal age is associated with accumulated exposure to environmental toxins, which may result in alteration of the paternal germ cells (Hultman, Sandlin, Levine, Lichtenstein, & Reichenberg, 2011). Hultman et al. also propose an alternate explanation in which advanced paternal age may contribute to an increased number of de novo genetic mutations that lead to ASD.
Given the strong evidence for genetic influences on both schizophrenia and ASD, it is clear that identification of endophenotypes for each of these disorders could be beneficial for aiding in the discovery of specific genes that affect each of these disorders. This also could lead to earlier identification of individuals with an increased risk for these disorders, thus leading to earlier intervention that may improve outcomes. A large number of studies have begun investigating endophenotypes, with some promising results. Below we review some of the more recent evidence for endophenotypes and discuss the implications for each disorder.
4 ENDOPHENOTYPES FOR SCHIZOPHRENIA AND ASD
4.1 Schizophrenia
A number of possible endophenotypes have been identified for schizophrenia as well as for disorders on the schizophrenia spectrum, such as schizotypal personality disorder. In fact, the number of researchers identifying and studying endophenotypes for schizophrenia in particular and for psychiatric illnesses in general has increased dramatically in the past decade (Braff & Tamminga, 2017). Certain endophenotypes, such as psychophysiological inhibitory responses to both internal and external stimuli, which are symptomatic of individuals diagnosed with schizophrenia and schizophrenia-like disorders, have been chosen because they are closer to the gene action and are less influenced by environmental factors (Cadenhead, Light, Geyer, McDowell, & Braff, 2002). Specific inhibitory endophenotypes that have been studied include prepulse inhibition of the startle response, the antisaccadic task assessing frontal lobe function, and inhibition of the P50 event-related potential using electroencephalography (EEG) measures. Each of these is related to inhibition abilities, but they are regulated by different neural substrates (Cadenhead et al., 2002). Preliminary data by Cadenhead et al. (2002) suggested that the P50 inhibition and antisaccadic tasks were similar in one subgroup of individuals with schizotypal personality disorders, whereas performance on the prepulse inhibition of the startle response identified a separate group of diagnosed individuals. They suggest that these neurobiological measures may better identify subgroups of patients in terms of genetic etiology than do symptoms of the disorder itself. This is evidence of the utility of endophenotypes because they are able to distinguish subtypes of a disorder or subgroups of patients who differ genetically. Such identification could result in more accurate classification of disorder subtypes and therefore in more accurate medical prescriptions. Therefore, the genes responsible for these endophenotypes need to be identified.
Further investigation of neurophysiological mechanisms has yielded other endophenotypes for schizophrenia worthy of future study. Comparisons between unaffected controls and relatives of individuals with schizophrenia on such mechanisms is important for identifying endophenotypes that can then be studied further to identify genetic underpinnings. For example, Earls, Curran, and Mittal (2016) demonstrated that event-related potentials (ERPs) significantly discriminated relatives of patients with schizophrenia from controls. Across a number of studies, family members performed worse than controls on several auditory ERP measures, including P50 suppression (assesses sensory gating), P300 amplitude and latency (assess attention and classification speed), and mismatch negativity (assesses ability to make perceptual discriminations). This information could be valuable for identifying family members at increased risk for the disorder, and it also is valuable as a research tool to help understand the genetic factors underlying the disorder. A relatively new examination of sleep spindles (an oscillation in the thalamocortical brain region that occurs during non-rapid eye movement in sleep), which may be related to sleep deficits in people with schizophrenia, has yielded evidence of the importance of the CACNA1L gene (involved in calcium channels) in mouse knockout studies (Manoach, Pan, Purcell, & Stickgold, 2015). Interestingly, this gene has previously been implicated in schizophrenia research (Ripke et al., 2014). This suggests another exciting avenue of study for a putative schizophrenia endophenotype.
More recently, the Consortium on the Genetics of Schizophrenia (COGS) was developed to further identify endophenotypes and specific genes related to schizophrenia (Swerdlow, Gur, & Braff, 2015). One unique aspect of the COGS is that it examined schizophrenia and related symptoms among family members (part of the COGS-1) as well as across non-related individuals (part of the COGS-2), which differentiated between genotypes that might be shared by family members (COGS-1) versus those that may be sporadic (COGS-2). Several endophenotypes were identified by COGS-1 by examining neurocognitive and neurophysiological deficits shared by patients with schizophrenia and several of their otherwise-unaffected family members. These included measures such as letter and number span memory, P50 suppression, and antisaccade performance (Swerdlow et al., 2015). Each of these endophenotypes demonstrated shared deficits within families, significant heritability, and various quantitative trait locus (QTL) associations. In a special issue examining a number of endophenotypes across both COGS-1 and COGS-2 samples, findings were essentially replicated across samples (Swerdlow et al., 2015). Interestingly, there are a large number of genes associated with these endophenotypes. A gene network comprised of 42 genes can be constructed to describe 12 related endophenotypes (Braff, 2015). Many of these genes have been identified in studies examining schizophrenia per se, such as COMT (Williams, Owen, & O'Donovan, 2007), NRG1, and ERBB4 (Braff, 2015).
The study of endophenotypes for understanding genetic underpinnings of schizophrenia and related spectrum disorders shows enormous promise. Even in the early 1900's, researchers were discerning that a single gene could not be responsible for these disorders and they must be multifactorial in origin, involving many genes and many possible environmental factors (Gottesman, 1991). However, the recent advent of endophenotype research has allowed researchers to close in on knowledge about some of the critical genes affecting these disorders. Nonetheless, this research is still in its infancy, and more replication studies are necessary before we can feel confident that relevant genes are correctly identified. Bear in mind that each gene accounts for a very small percent of the variability in each endophenotype, making reliable identification of relevant genes difficult. We feel confident that many of the research findings thus far are putting us on track to identify relevant genes. Even though genetic influences on endophenotypes of schizophrenia are not already clearer than those for schizophrenia per se, findings from groups such as COGS suggest that large samples using multiple methodologies may converge on comparable findings sometime in the not too distant future.
4.2 Autism spectrum disorder (ASD)
The study of endophenotypes for ASD is complicated by the fact that ASD is a developmental disorder, meaning that expression of the phenotype as well as expression of any endophenotypes change developmentally over time (Viding & Blakemore, 2007; Volkmar & McPartland, 2014). In addition, there are varying degrees of symptoms due to the wide range of expression of ASD, and intellectual functioning can vary widely as well (Viding & Blakemore, 2007). For these reasons, the search for endophenotypes is complex and may benefit from a focus on specific characteristics of ASD rather than considering the disorder as a whole. Endophenotypes also may be useful to help identify etiologically distinct subgroups of ASD in terms of diagnoses.
Researchers have considered a number of mental functioning abilities as possible endophenotypes for ASD. Some of these endophenotypes may be more related to certain symptom presentations, whereas other endophenotypes may be more related to other symptom sets. These abilities can be classified as endophenotypes as long as they are more directly impacted by genes than are classic ASD symptoms, and as long as they are related to ASD symptoms. Some of the endophenotypes that have been identified for studying ASD include theory of mind, language skills, social skills, and certain brain functions. Although aspects of these are used to diagnose ASD, people with ASD show greatly different levels of severity (Viding & Blakemore, 2007), and thus variability within each of these behaviors can be informative in terms of studying genetic influences on ASD. Each of these appears to hold promise for leading the way to particular genes that comprise the family of genetic influences on ASD.
Because of the developmental and diverse nature of ASD symptoms, studies of endophenotypes have been disparate and require replication. It is important to consider different subgroups of children with ASD, which can include subgroups based on level of intelligence, symptom severity, or functional impairment. The utility of endophenotypes will differ depending on the nature of the genetic influences that vary among these populations. For instance, Alarcon, Yonan, Gilliam, Cantor, and Geschwind (2005) used data from the Autism Genetic Resource Exchange (AGRE), which included nuclear families that had two or more children with possible ASD. They found that children with ASD who spoke their first word at much younger ages differed in terms of a QTL on chromosome 7, suggesting that language ability may discriminate children with ASD in terms of underlying genetic influences. These researchers demonstrated the possible value of considering age at first spoken word, age at first spoken phrase, and repetitive or stereotyped behaviors as endophenotypes for ASD, given that these behaviors show variability across children with ASD. Also, it is important to recognize that these may have other important causal factors such as parent IQ and parenting behaviors. The researchers identified specific susceptibility QTLs for each of these endophenotypes on several chromosomes, especially chromosome 3.
Using the same large AGRE sample, Lowe, Werling, Constantino, Cantor, and Geschwind (2015) examined social responsiveness rather than language as an ASD endophenotype. Social responsiveness differs from typical endophenotypes in that it is less reliable and less neurological than many other endophenotypes typically considered. However, reliability of their measure of social responsiveness was improved by using both parent and teacher ratings. This suggested phenotype does appear to be valuable; the researchers identified a strong effect for a QTL on chromosome 8. They note that the locus linkage peak for social responsiveness overlaps with a linkage signal for ASD (Lowe et al., 2015). Furthermore, the particular region of interest has been noted as relevant to other chronic disorders significantly associated with functional impairment (e.g., epilepsy and schizophrenia) using different linkage approaches (Lowe et al., 2015). However, Lowe et al. noted that their findings lack consistency with previous studies of social responsiveness as an ASD endophenotype. They noted that other studies have shown linkage on other chromosomes (e.g., chromosomes 11 and 17) and have failed to find an effect for a QTL on chromosome 8. Thus, there appears to be genetic heterogeneity for social responsiveness as an ASD endophenotype, and further replication studies are needed.
Increased variability across trials in neural activity in response to certain stimuli may be an endophenotype closer to an actual genetic mechanism (David et al., 2016). Specifically, David et al. suggest that asynchronization of neural activity in individuals with ASD can be seen using techniques such as EEG or magnetoencephalography (MEG), and these responses can be identified as valuable endophenotypes for ASD. Although this has not yet been used to identify specific genes related to this behavior and therefore to ASD, it appears to be an excellent candidate for an endophenotype. Similarly, functional magnetic resonance imaging (fMRI) has been used to examine brain responses to emotional faces in siblings of children with autism versus controls (Spencer et al., 2011). These siblings show subtle impairments in their responses to emotional faces compared to controls, and this can be measured using fMRI. The study by Spencer et al. demonstrated reduced activation in the fusiform face area (FFA) of the brain as well as other related areas, as measured with fMRI, when adolescents and their siblings were shown emotional faces. This differed significantly from responses of control adolescents. As with the neural activity asynchronicity, this brain response to emotional faces may be an important endophenotype to explore further to identify specific genes related to ASD. Many other researchers are beginning to identify endophenotypes for ASD at the neurological level that should be useful for future research in identifying specific related genes (e.g., Moseley et al., 2015; Sacco et al., 2010).
5 CONCLUSION
Our appreciation of endophenotypes has come a long way since its initial introduction by Gottesman (Gottesman & Shields, 1967). Endophenotypes are quantitative measures that are closer to the gene action than is the psychiatric disorder, can be used in qualitative analyses, and are genetically less complex than the psychiatric disorder (Braff & Tamminga, 2017). Schizophrenia and autism are complex psychiatric disorders (David et al., 2016) characterized by a spectrum of related phenotypes, notably with family members showing some deficits typical of the disorder but without having the full-blown disorder themselves. Thus, they are excellent disorders for examining endophenotypes, behaviors that are shared by family members because of shared genes, even though the disorder may not be fully expressed among all family members. Some evidence suggests that the two disorders share an underlying genetic etiology (Ishizuka et al., 2016; Ripke et al., 2014), and therefore further study of their endophenotypes will allow researchers to address this (Chisolm, Lin, Abu-Akela, & Wood, 2015). Because of the link between genes, endophenotypes, and disorder, identification of endophenotypes is useful for beginning the search to identify specific genes that affect these disorders. This work is still in its infancy and there are great difficulties to overcome, such as the polythetic nature of these disorders, with symptoms varying across individuals even within a diagnosis (Swerdlow et al., 2015). Additionally, the ethical issues that must always be considered when studying genetics of behavior are varied and numerous. For instance, if we identify genotypes that represent an increased risk for an endophenotype associated with schizophrenia, is it appropriate to intervene prenatally? There are huge pharmacotherapy and ethical concerns about doing this (Braff, 2015), especially when the risk is not 100% (which it never will be, as endophenotypes are not linked 100% with the disorder). At this time, there still is not clear evidence that identified genes related to specific endophenotypes parallel those for the actual disorders. Nonetheless, by beginning to identify the genetic underpinnings of disorders such as these, clinicians and doctors will be better poised to accurately diagnose and treat disorders that may alter normative functioning.
ACKNOWLEDGMENT
We would like to acknowledge and thank Dr. Irving I. Gottesman, whose prior mentorship has shaped our ways of viewing the world.