Dentofacial Findings and Management of two Pediatric Patients With Bainbridge-Ropers Syndrome: A Case Report
Funding: The authors received no specific funding for this work.
ABSTRACT
Bainbridge-Ropers Syndrome(BPRS) is a rare autosomal dominant genetic disorder resulting from heterozygous mutations in the ASXL3(Additional Sex Comb-Like 3) gene located on chromosome 18q12. To date, only 45 cases have been documented in the literature. BPRS is characterized by a range of clinical features, including feeding difficulties, hypotonia, distinctive dysmorphic facial features, high-arched palate, and intellectual disability. This case report aims to present two pediatric patients diagnosed with BPRS, emphasize newly identified oro-dental manifestations, and propose a comprehensive dental management plan. In Case #1, a 10-year-old female patient presented to the clinic with concerns of developmental delay and spinal deformity. Physical examination revealed trigonocephaly, thoracic kyphosis, strabismus, hirsutism, bitemporal narrowing, and bilateral coxa valga. Additionally, the patient exhibited failure to thrive, language difficulties, and mild intellectual disability. Oral examination identified a high-arched palate, fibrotic frenulum, narrow maxilla, and posterior crossbite. In Case #2, a 6-year-old female patient presented with developmental delay, language difficulties, and mouth breathing. Physical findings included trigonocephaly, bitemporal narrowing, strabismus, hirsutism, and arched eyebrows. Oral examination revealed a high-arched palate, narrow maxilla, and open bite. For both cases, preventive dental interventions were implemented, including the application of fissure sealants, fluoride varnishes, dietary regulation, and the use of interceptive orthodontic appliances. Children diagnosed with BPRS require ongoing medical and dental management through a multidisciplinary approach to address the complex and varied manifestations of the disorder effectively.
1 Introduction
Bainbridge-Ropers Syndrome (BRPS, OMIM #615485) is a rare genetic disorder first identified in 2013, caused by mutations in the Additional Sex Comb Like 3 (ASXL3) gene located on chromosome 18q12. This mutation results in a range of clinical manifestations, including developmental delay, intellectual disability, and distinct craniofacial and skeletal abnormalities (Bainbridge et al. 2013) There was no evidence-based information that gender and regional differences impact the occurrence of BRPS cases. BRPS is characterized by severe feeding issues, muscular hypotonia, facial dysmorphism, trigonocephaly, limited speech development, and profound intellectual disability. Distinctive orofacial features include a long face, arched eyebrows, downward-slanting palpebral fissures, a prominent forehead, strabismus, and a high, narrow palate. To date, only 45 BRPS cases have been documented (Bainbridge et al. 2013; Balasubramanian et al. 2017; Contreras-Capetillo et al. 2018; Dad et al. 2017; Dinwiddie et al. 2013; Hori et al. 2016; Koboldt et al. 2018; Kuechler et al. 2017; Myers et al. 2018; Srivastava et al. 2016; Verhoeven et al. 2018; Wayhelova et al. 2019). There are reports featuring people from a range of ancestry backgrounds from the United States, Sudan, China, Japan, Korea, Mexico, and the United Kingdom, and most individual case reports included information about pediatric patients (Woods et al. 2024).
The treatment of children with this rare syndrome is both critical and essential for enhancing their quality of life. This case report aims to present two previously unpublished cases of BPRS, emphasizing their novel oro-dental findings and outlining a comprehensive dental treatment plan. Notably, fibrotic frenulum, posterior crossbite, and enamel lesions were identified as unique oro-dental features, representing previously unreported manifestations of BPRS in the literature.
2 Case Report
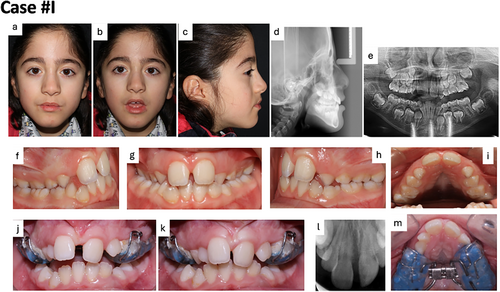
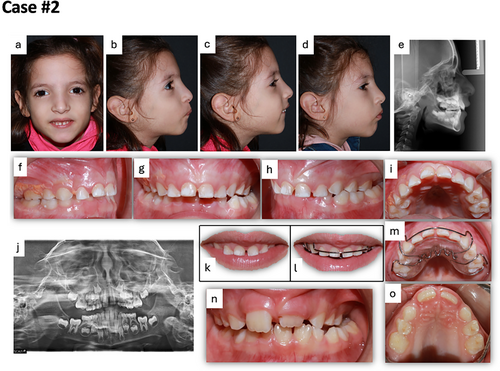
In both cases, the patients were under 18 years of age, and written informed consent for publication of identifying images or other personal or clinical details was taken from their parents. The individuals involved in case #1 and case #2 are from distinct, unaffiliated family units. Comprehensive dental and radiographic examinations (Figures 1 and 2) were conducted by two specialized pediatric dentists, while preventive orthodontic treatment was administered by an orthodontist. The clinical and oro-dental characteristics of the two BPRS patients are summarized in Table 1.
| Phenotypic features | Case #1 | Case #2 |
|---|---|---|
| Growth failure | + | + |
| Developmental delay | + | + |
| Seizures | − | − |
| Intellectual disability | + | + |
| Speech impairment | Meaningless few words | Absent of speech |
| Feeding difficulties | + | + |
| Muscular hypotonia | + | + |
| Free walking | + (with support) | − |
| Prominent forehead | + | + |
| Bitemporal narrowing | + | + |
| Trigonocephaly | + | + |
| Facial dysmorphism | + | + |
| Low anterior hairline | + | + |
| Arched eyebrows | + | + |
| Downslanting palpebral fissures | + | + |
| Strabismus | + | + |
| Hirsutism | Severe | Low |
| High arched palate | + | + |
| Narrow maxilla | + | + |
| Fibrotic frenulum | + | − |
| Posterior crossbite | + | + |
| Enamel lesions | − | + |
| Macro/microdontia | − | − |
| Hypodontia/hyperdontia | − | − |
| Mouth breathing | + | + |
| Swallow difficulties | − | − |
| Late eruption/exfoliation of teeth | − | − |
2.1 Case #1
The patient was a 10-year-old girl, the firstborn child of a healthy, nonconsanguineous Turkish couple. The patient was referred to Ege University Medical Faculty Hospital, Department of Pediatric Genetics in 2021 with the complaint of developmental delay and spinal deformity. The patient's medical history revealed a cesarean section birth at 37 weeks, with a birth weight of 2.4 kg, followed by severe developmental delays. Her history revealed a significant developmental delay; she started supported walking at age 2.5 years and only used a few meaningless words for talking at age 2 years. At age 10, there is still no improvement in walking and speech abilities. In physical examination, trigonocephaly, strabismus, prominent forehead, low anterior hairline, bitemporal narrowing, and hirsutism were observed (Figure 1a,b). Severe hypotonia was recognized in the muscular examination.
Exome sequencing (ES) analysis of the patient identified a heterozygous c.1151_1157del (p.Ser384AsnfsTer23) variant in the ASXL3 (NM_030632.3) gene, responsible for BPRS. Parental molecular analysis confirmed that the variant occurred de novo. The variant was absent in population databases (e.g., gnomAD, ExAC) and had not been previously reported in the literature. Based on the ACMG 2015 criteria (Richards et al. 2015), it was classified as “likely pathogenic” due to its frameshift nature and de novo occurrence.
The patient was referred to Ege University, Faculty of Dentistry, Department of Pedodontics for the oral examination. Fibrotic frenulum and posterior crossbite are followed in Figure 1g,k in maximum intercuspation. Fibrotic frenulum diagnosed with the blanching/tension test and no treatment was deemed necessary. The patient has no difficulty in swallowing. In the intraoral and radiologic evaluation, delayed eruption or exfoliation of teeth was not observed. In addition, no shape (macrodontia/microdontia) and number anomalies (hypodontia/hyperdontia) were found. Maxillary narrowing and high, deep arched palate are directly shown in Figure 1i. The lower third of the face appeared elongated in both frontal and resting photographs (Figure 1b), and an increased interlabial gap was evident, supporting the diagnosis of a hyperdivergent vertical growth pattern. The patient demonstrated difficulty in achieving oral closure, attributed to hypotonia, tongue dysfunction, and mouth breathing. These factors were identified as contributors to maxillary underdevelopment and the associated bilateral crossbite due to maxillary constriction. A straight facial profile was observed, characterized by reduced nasal projection, while the nasolabial angle and labiomental sulcus depth were within normal parameters (Figure 1c). Cervical vertebrae maturation analysis indicated a developmental stage between CS2 and CS3 according to Baccetti et al. (Baccetti et al. 2005) (Figure 1d). The patient presented with a bilateral posterior crossbite, a deep V-shaped palate, a fibrotic frenulum leading to a median diastema, and space deficiencies in both the maxillary and mandibular arches (Figure 1f–i). Additionally, the Curve of Spee was notably deep, and the Curve of Wilson was exaggerated (Figure 1f,h). No signs of mandibular shift or dental wear were detected. Cephalometric analysis (Dolphin, Patterson Dental Supp., Chatsworth, CA, USA) was conducted in the Department of Orthodontics. The analysis revealed a skeletal Class III relationship due to maxillary retrusion (SNA: 77.6, ANB: 0°; Wits: −1.6 mm), with the Wits value further supporting the Class III diagnosis. All vertical parameters indicated a hyperdivergent growth pattern (Y-axis: 71.0°; FMA: 35.9°; anterior facial height: 93 mm). The lower incisor angles were reduced, while the upper incisor angles were within normal limits (SN-U1: 113.7°; IMPA: 77.1°), and the overjet was decreased, similar to a camouflaged Class III patient. The treatment plan involved rapid maxillary expansion using an acrylic cap splint to address the maxillary constriction, posterior crossbite, and to improve airway function (Figure 1j,m). The appliance was activated twice daily for 14 days, with each two activations targeting 0.25 mm of expansion, continuing until a median diastema appeared as an indicator of sutural opening (Figure 1j). After activation, a periapical radiograph was taken between the upper incisors to confirm that the expansion resulted from sutural separation (Figure 1l). The appliance was retained for 4–6 months to prevent relapse, with Figure 1k showing the results 1 month after the expansion was completed.
In light of the limited published data on orthodontic and dental management for patients with this syndrome, a definitive long-term treatment plan was not formulated. Instead, the primary objectives focused on addressing the patient's immediate functional needs and evaluating her level of cooperation to inform potential future interventions.
2.2 Case #2
The patient was a 6-year-old girl, the second-born child of a healthy, nonconsanguineous Turkish couple. Her medical history indicated she was born by cesarean section at 39 weeks, with a birth weight of 3.65 kg. She had a history of a significant developmental delay; she was unable to walk and speak at the time of referral. In the physical examination, trigonocephaly, bitemporal narrowing, strabismus, hirsutism, and arched eyebrows were detected (Figure 2a,b).
ES revealed a heterozygous ASXL3 (NM_030632.3) c.1630_1636del (p.Ile544ProfsTer5) variant in the patient. Parental testing confirmed that this variant arose de novo. It was not listed in population databases such as gnomAD or ExAC, and no prior reports of this variant were found in the literature. Given its frameshift nature and de novo occurrence, it was classified as “likely pathogenic” according to the ACMG 2015 guidelines (Richards et al. 2015).
The patient was referred to Ege University, Faculty of Dentistry, Department of Pedodontics in 2022 with complaints of mouth breathing and linguistic difficulties. In the oral examination, enamel lesions, a high arched palate, a narrow maxilla, and a posterior crossbite were detected and shown in Figure 2f–i. No signs of delayed tooth eruption or exfoliation were observed, and the dentition exhibited no abnormalities in tooth morphology or number. Evaluation of the frontal photograph revealed misalignment of the pupils and a deviation of the chin toward the left of the facial midline (Figure 2a). The profile photograph revealed a convex facial profile, characterized by an inability to achieve lip closure. The patient exhibited habitual lower lip sucking in an effort to approximate the lips (Figure 2b,c). She was consistently unable to close her lips, and the family reported that she frequently sucked on her lower lip and placed her tongue between the anterior teeth when not sucking. She was in the primary dentition stage, with increased overjet and overbite. A mandibular shift and left posterior crossbite were noted due to maxillary constriction (Figure 2f–i). Severe wear was observed on the lower left lateral incisor (tooth no. 72) due to the mandibular shift. After the central incisors erupted, a fibrotic labial frenulum and a V-shaped maxillary arch were observed (Figure 2n,o). Cephalometric analysis (Dolphin, Patterson Dental Supp., Chatsworth, CA, USA) revealed a skeletal Class II sagittal relationship caused by mandibular retrusion (SNB: 72.7, ANB: 6.3°; Wits: 2.4 mm) and a hyperdivergent growth pattern (Y-axis: 69.9°; FMA: 29.9°; anterior facial height: 91.8 mm). The upper incisor angles were reduced, while the lower incisor angles were within normal limits (SN-U1: 93.4°; IMPA: 87.4°). The treatment plan involved rapid maxillary expansion to address the maxillary constriction, left posterior crossbite, and mandibular shift, though expansion was delayed until the eruption of the first molars to provide adequate anchorage. A removable acrylic tongue crib was applied to prevent lower lip sucking and tongue thrusting to assess the patient's cooperation (Figure 2m). Photos documenting the changes in lip posture after applying the tongue crib are shown (Figure 2k,l). The patient was able to use the appliance for up to 7 h daily, and at the 6-month follow-up, the overjet had decreased, and the upper and lower central incisors had erupted (Figure 2n). In the lateral photograph, the patient could now close her lips (Figure 2d). Cephalometric and panoramic radiographs were taken when the upper central incisors erupted, and a radiographic analysis was performed (Figure 2e,j). The patient demonstrated a high level of cooperation, promptly adhering to instructions and maintaining comfort during dental procedures. Although she was unable to independently insert or remove the removable appliance, her mother provided assistance with these tasks. The patient effectively communicated her desire for appliance removal through non-verbal cues.
In both cases, preventive dental applications (fluoride varnishes, diet regulation) were performed. The patients were unable to use their hands, arms, and fingers to maintain their own oral hygiene due to impaired motor skills. Parents were encouraged to implement daily plaque control and to develop anticariogenic diet habits. It was stated that tooth surfaces should be cleaned by parents after food consumption, and regular dental check-ups were instructed.
3 Discussion
Monoallelic mutations in the ASXL3 gene result in Bainbridge-Ropers Syndrome (BPRS), a rare autosomal dominant disorder first identified by Bainbridge et al. in 2013 (Bainbridge et al. 2013). Since its initial description, only 45 cases have been reported in the literature, underscoring the importance of continued documentation to refine the clinical phenotype of BPRS. Molecular characterization in all reported cases has been achieved through whole exome sequencing (WES) and whole genome sequencing (WGS) (Ababneh et al. 2019; Bainbridge et al. 2013). No significant gender difference has been observed in the incidence of the syndrome (Ababneh et al. 2019).
The ASXL gene family comprises ASXL1, ASXL2, and ASXL3, with de novo mutations in ASXL1 causing Bohring-Opitz Syndrome. This syndrome shares overlapping clinical features with BPRS, such as feeding difficulties, severe intellectual disability, and failure to thrive (Bainbridge et al. 2013; Balasubramanian et al. 2017; Kuechler et al. 2017).
Clinical features of BRPS are shown in Table 2 according to published case reports (Bainbridge et al. 2013; Balasubramanian et al. 2017; Contreras-Capetillo et al. 2018; Dad et al. 2017; Dinwiddie et al. 2013; Hori et al. 2016; Koboldt et al. 2018; Kuechler et al. 2017; Myers et al. 2018; Srivastava et al. 2016; Verhoeven et al. 2018; Wayhelova et al. 2019). In previous BRPS cases, developmental delay and intellectual impairment were consistently observed, as in the present cases.
| Clinical features | Previous case reports (n = 45) |
|---|---|
| Growth failure | 18/39 |
| Hypotonia | 38/42 |
| Downslanting palpebral fissures | 27/40 |
| Feeding difficulties | 35/41 |
| Speech impairment | 23/36 |
| Intellectual disability | 39/40 |
| Seizure | 17/38 |
| Skeletal problem | 29/36 |
| Narrow maxilla | 23/36 |
In this report, we describe two novel frameshift variants in ASXL3 (c.1151_1157del and c.1630_1636del), which have not been previously reported in the literature. These findings expand the known mutational spectrum of ASXL3 and further support the role of haploinsufficiency in the pathogenesis of BPRS. The phenotypic presentation of our patients aligns with previously reported cases.
Growth failure was noted in 18 out of 39 patients, and only half could walk independently. Around half of the patients experienced seizures or structural cognitive impairments, and severe hypotonia was observed in 90% during the neurological examination. Gastrointestinal issues and feeding difficulties affected 85% of the patients (Ababneh et al. 2019). The incidence of craniofacial findings differs between cases; strabismus in 11, open forehead in 17, arched eyebrows in 17, anteverted nares in 13, and down/upslanting palpebral fissures in 27 patients out of a total 36 were reported in the literature (Ababneh et al. 2019).
This case report is the first to evaluate the dentofacial findings with the x-rays and intraoral photographs, designing a treatment plan for a patient with BRPS by a specialized dentist. The findings in the oro-dental region in the 45 reported cases were not evaluated by the dentist and therefore it is possible that some findings were missed or underreported. Unlike other cases in the literature, case #1 displayed a fibrotic frenulum, case #2 had enamel lesions, and both patients exhibited a posterior crossbite. The novelty that this case contributes to the knowledge in comparison to those already reported was these new oro-dental features. Only one report mentioned micrognathia and macrodontia in a permanent maxillary central incisor as different dental features (Koboldt et al. 2018).
In previous case reports, a high-arched palate was a common intraoral finding, yet it remained untreated (Ababneh et al. 2019; Koboldt et al. 2018; Kuechler et al. 2017). The most clinically important symptom of maxillary narrowing is posterior crossbite. In mouth-breathing individuals, the tongue is positioned lower, resulting in a muscle balance on the upper posterior teeth. It is argued that this disrupted force balance in favor of the cheek muscles causes posterior crossbite. In both cases we report, mouth breathing and maxillary narrowing are observed and, as a consequence, posterior crossbite is also exhibited. It is known that posterior crossbite and maxillary narrowing do not correct spontaneously, and the most commonly used orthodontic treatment is the rapid maxillary expansion appliance for open midpalatal suture. In case #1, a bonded rapid maxillary expansion appliance with an acrylic cap splint was designed. As it is bonded directly to the teeth, even a patient with special care needs was able to use the appliance comfortably. Other benefits are that it can be used during the mixed dentition period and the frequency of appointments is reduced (Agarwal and Mathur 2010).
During the dental treatment, pharmacological behavior guidance techniques were not needed for BRPS patients who could not communicate verbally and needed special care. On the contrary, they showed very compliant behavior with the dentist during dental examination and treatment. Nevertheless, it should be taken into consideration that the behavioral pattern may change if more invasive and painful dental procedures are required.
Oral hygiene of BRPS patients evaluated, it should not be forgotten that these patients have retarded motor skills and limited use of their hands and arms. For this reason, they do not have the consciousness to maintain oral hygiene habits, nor do they have the physical ability to brush their teeth. Despite this, surprisingly no extensive caries and gingival inflammation were found in both patients. However, it is always recommended that the cleaning of the tooth surfaces be provided by their parents for preventing dental caries and periodontal diseases. Regular dental check-ups, anticariogenic diet, and preventive dental applications are recommendations to reduce the patient's risk of caries.
4 Conclusions
Bainbridge-Ropers Syndrome is an exceedingly rare genetic disorder characterized by developmental delay, feeding difficulties, and speech impairment, with only 45 cases documented in the literature to date. The identification of two novel ASXL3 variants in our patients further expands the genetic landscape of Bainbridge-Ropers Syndrome and reinforces the importance of comprehensive genetic testing. Our findings contribute to the growing understanding of genotype–phenotype correlations in ASXL3-related disorders and highlight the need for ongoing clinical and molecular characterization to refine the full spectrum of this rare syndrome. Due to the rarity of the syndrome, thorough documentation of each case is essential for enhancing the understanding of its clinical phenotype. Given the frequent involvement of the oro-facial region, dental evaluation by a pediatric dentist is recommended for BPRS patients, as preventive dental interventions may provide significant benefit. Continuous follow-up and coordinated care, integrating both medical and dental management, are essential for achieving the best outcomes. A multidisciplinary approach is crucial to ensure comprehensive care for the patient.
Author Contributions
A.A., D.Ç., and Ö.Ç. conceived the idea; A.A., E.C.F., E.A.D., D.Ç., T.A., A.M.E., and Ö.Ç. collected and analyzed the data; A.A., E.C.F., D.Ç., and Ö.Ç. led the writing and revised the manuscript and gave final approval of the version to be published, and agreed to be accountable for all aspects of the study.
Acknowledgments
This case presentation followed the CARE guidelines.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




