Emergence of the natural history of Myhre syndrome: 47 patients evaluated in the Massachusetts General Hospital Myhre Syndrome Clinic (2016–2023)
Abstract
Myhre syndrome is an increasingly diagnosed ultrarare condition caused by recurrent germline autosomal dominant de novo variants in SMAD4. Detailed multispecialty evaluations performed at the Massachusetts General Hospital (MGH) Myhre Syndrome Clinic (2016–2023) and by collaborating specialists have facilitated deep phenotyping, genotyping and natural history analysis. Of 47 patients (four previously reported), most (81%) patients returned to MGH at least once. For patients followed for at least 5 years, symptom progression was observed in all. 55% were female and 9% were older than 18 years at diagnosis. Pathogenic variants in SMAD4 involved protein residues p.Ile500Val (49%), p.Ile500Thr (11%), p.Ile500Leu (2%), and p.Arg496Cys (38%). Individuals with the SMAD4 variant p.Arg496Cys were less likely to have hearing loss, growth restriction, and aortic hypoplasia than the other variant groups. Those with the p.Ile500Thr variant had moderate/severe aortic hypoplasia in three patients (60%), however, the small number (n = 5) prevented statistical comparison with the other variants. Two deaths reported in this cohort involved complex cardiovascular disease and airway stenosis, respectively. We provide a foundation for ongoing natural history studies and emphasize the need for evidence-based guidelines in anticipation of disease-specific therapies.
1 INTRODUCTION
Since the first description in two unrelated male patients (Myhre et al., 1981), Myhre syndrome (MIM #139210, ORPHA #2588) has been increasingly recognized as a distinctive short stature syndrome with a recognizable facial appearance, hearing loss, and progressive abnormalities of the cardiovascular system, upper airway, lungs, skin, bones, and joints. An extremely variable neurobehavioral phenotype has emerged, which often includes developmental delay and/or autism spectrum disorder (ASD). The molecular basis of Myhre syndrome was reported as missense heterozygous changes affecting the Ile500 residue (amino acid changes to valine, threonine, and methionine) of the SMAD4 gene (chromosome 18q12.2, NM_005359.6): c.1498A > G (p.Ile500Val); c.1499 T > C (p.Ile500Thr), c.1500A > G (p.Ile500Met), and later as c.1486C > T (p.Arg496Cys) (Caputo et al., 2012; Caputo et al., 2014; Le Goff, Mahaut, Abhyankar, et al., 2011; Le Goff, Mahaut, Wang, et al., 2011; Michot et al., 2014). The molecular mechanisms underlying Myhre syndrome remain incompletely understood, but data support activating variants rather than loss of function variants in SMAD4 as the pathogenic mechanism of disease (Piccolo et al., 2014).
Ongoing phenotype delineation began with the recognition that Myhre syndrome shared the same locus with the laryngeal, arthropathy, prognathism, and short stature (LAPS) syndrome (Hopkin et al., 1998; Lindor et al., 2002; Lindor et al., 2012; Oldenburg et al., 2015). The international literature has expanded from case reports and small series (listed in order of publication as Soljak et al., 1983; García-Cruz et al., 1993; Titomanlio et al., 2001; Whiteford et al., 2001; Davalos et al., 2003; Lopez-Cardona et al., 2004; Rulli et al., 2005; van Steensel et al., 2005; Becerra-Solano et al., 2008; Bachmann-Gagescu et al., 2011, McGowan et al., 2011; Starr et al., 2015; Wurfbain et al., 2023; Hui et al., 2023) to larger reviews (Cappuccio et al., 2022; Garavelli et al., 2016; Lin et al., 2016; Starr et al., 2022; Yang et al., 2022). Population-based studies have not been conducted; nevertheless, Myhre syndrome can be considered an ultrarare disease which is typically defined as having a birth prevalence of fewer than one per 50,000 (reviewed by Smith et al., 2022).
This state-of-the-art review studied patients evaluated at the Massachusetts General Hospital (MGH) Myhre Syndrome Clinic. We expand on the type, frequency, pattern, and clinical course of abnormalities within nearly every organ system, including neuropsychology, behavior, and neoplasia. We evaluate patterns (phenotypes) when possible, perform genotype and phenotype correlations, and assess progression across the lifespan. We propose that the systematic evaluation of these patients in a multi-specialty academic program creates a Myhre syndrome “medical home.” This model can assist the local providers, provide a favorable environment for management across the lifespan (natural history), and prepare for future clinical trials.
2 METHODS
2.1 Editorial policies and ethical considerations
This research was approved by the MGH Institutional Review Board under two protocols: #2015P001173 and #2000P001531. The study design was a retrospective cohort study with prospective data collection, and clinical reports of the two oldest patients.
2.2 The MGH Myhre Syndrome Clinic
During a 7-year period (July 1, 2016 to June 30, 2023), patients with Myhre syndrome were either self-referred or referred by a medical provider. We abstracted information from our institution's electronic health system which allows us to also view reports from selected participating institutions (details in Supplementary File Methods).
2.3 Diagnosis and definitions
The diagnosis of Myhre syndrome was confirmed by clinical or research-based genomic DNA diagnostic sequencing and patients were confirmed to have a germline SMAD4 pathogenic variant (details in Supplementary File Methods). Throughout this article, we generally refer to the SMAD4 affected protein residue for brevity rather than the complete nomenclature with transcript, nucleotide change, and predicted protein changes (Table 1).
| Short form SMAD4 variant | Complete name | Transcript: NM | Coding | Predicted protein |
|---|---|---|---|---|
| Ile500Val | NM_005359.6(SMAD4):c.1498A > G (p.Ile500Val) | NM_005359.6 | c.1498A > G | Ile500Val |
| Ile500Thr | NM_005359.6(SMAD4):c.1499 T > C (p.Ile500Thr) | NM_005359.6 | c.1499 T > C | Ile500Thr |
| Ile500Met | NM_005359.6(SMAD4):c.1500A > G (p.Ile500Met) | NM_005359.6 | c.1500A > G | Ile500Met |
| Ile500Leu | NM.005359.6(SMAD4):c.1498A > C (Ile500Leu) | NM_005359.6 | c.1498A > C | Ile500Leu |
| Arg496Cys | NM_005359.6(SMAD4):c.1486C > T (p.Arg496Cys) | NM_005359.6 | c.1486C > T | Arg496Cys |
2.4 Severity analysis
Patients were classified according to the presence or absence of “severe” features which were defined as needing surgical or other invasive treatment or representing a known risk factor for mortality in the general population. Further classification as mild or moderate severity was not possible because of the highly subjective view of many physical and functional features.
2.5 Diagnostic testing
As appropriate for age, diagnostic testing for all patients included transthoracic echocardiography, electrocardiography (ECG), computed tomography angiography (CTA) of the aorta (usually without anesthesia, assisted by the Child Life specialist), and pulmonary function testing. Magnetic resonance imaging (MRI) of the brain and spinal cord, and CT of the spine or temporal bones were also performed. Outside imaging was reviewed by our team, and included CT of the skull, spine, facial, or temporal bones, and MRI of the brain or spine. Certain studies usually performed before the patient's visit included chest radiographs, skeletal survey and long bone radiographs to assess for fractures.
Laboratory testing included both outside test results, and those ordered during the MGH visit. Aside from DNA-based confirmation of Myhre syndrome, there were no obligatory lab tests because evidence-based diagnostic batteries have not yet been established.
3 CLINICAL REPORTS
To enhance the natural history analysis, we describe the two oldest patients in our cohort (Table 2).
| Feature | Number patients (%)a |
|---|---|
| Sex: Female | 26 (55%) |
| Age (years) at diagnosis (n = 47), age at last follow-up (n = 46) | |
| 0–3 | 17 (36%), 0 (0%) |
| 4–12 | 24 (51%), 33 (72%) |
| 13–18 | 2 (4%), 5 (11%) |
| 19–30 | 1 (2%), 4 (9%) |
| Older than 30 | 3 (6%), 4 (9%) |
| Paternal age at birth, mean (n = 45) (years) | 37 |
| Race | |
| White | 36 (77%) |
| Asian (includes south Asian) | 0 (0%) |
| American Indian or Alaska Native | 1 (2%) |
| Black or African American | 1 (2%) |
| Native Hawaiian or Other Pacific Islander | 0 (0%) |
| Other | 2 (4%) |
| Not stated | 7 (15%) |
| Ethnicity | |
| Hispanic or Latino | 7 (15%) |
| Not Hispanic or Latino | 40 (85%) |
| Ordering provider | |
| Geneticist | 40 (85%) |
| Neurologist | 3 (6%) |
| Genetic counselor | 1 (2%) |
| Developmental physician assistant | 1 (2%) |
| Research studies | 2 (4%) |
| SMAD4 affected protein residue | |
| p. Ile500Val | 23 (49%) |
| p. Ile500Thr | 5 (11%) |
| p. Ile500Met | 0 (0%) |
| p. Ile500Leu | 1 (2%) |
| p. Arg496Cys | 18 (38%) |
| First tier genetic testing | |
| Karyotype only | 5 (11%) |
| FISH analysis for deletion 22q11.2 | 3 (6%) |
| Chromosome analysis and/or microarray | 44 (94%) |
| Mitochondrial analysis (sequence analysis and deletion testing; muscle biopsy) | 6 (13%) |
| Prior targeted single gene or gene panel testing which did not include SMAD4 | 22 (47%) |
| DNA-based analyses which led to diagnosis | |
| Targeted gene analysis | 4 (9%) |
| Panel for autism/ID | 4 (9%) |
| Panel for cancer screening | 1 (2%) |
| Panel, other | 1 (2%) |
| Exome sequencing clinical | 33 (70%) |
| Exome sequencing, research-based | 1 (2%) |
| Genome sequencing clinical | 1 (2%) |
| Genome sequencing, research-based | 2 (4%) |
| Pathogenic mutation, or likely causative variant, total | 3 (6%) |
| Lamellar ichthyosis due to compound heterozygous mutations in TGM1 R126H (maternal) and Y134C (paternal) | 1 (2%) |
| …PITX3c.662_663delinsA, p.(G221Dfs*88) | 1 (2%) |
| …CYP2C19 | 1 (2%) |
| Co-occurring chromosome abnormalities | 1 (2%) |
| Balanced Robertsonian translocation, verified with lab report | 1 (2%) |
- Abbreviations: CMA, chromosome microarray; ID, intellectual disability; IEM, inborn error of metabolism; NA, not available; PCP, primary care provider, pt, patient; VUS, variant unknown significance.
- a Total of percentages may not equal 100% due to rounding.
3.1 Patient 1
The oldest known person with Myhre syndrome is a 53-year-old woman. She was found to have a rare a SMAD4 variant, p.Ile500Leu (figure 6B in Lin et al., 2022). A socially active college graduate who is married, she serves as a patient advocate for the Myhre Syndrome Foundation (MSF) support group. After three decades pursuing a genetic explanation for multiple unexplained features, especially hearing loss, she was diagnosed with Myhre syndrome at age 49 years by exome sequencing which excluded other genetic variants for sensorineural hearing loss. Prior testing included a normal chromosome microarray as well as repeat expansion testing for myotonic dystrophy type 1 and type 2. Her variant is unique in our cohort, and her features are listed in individual columns in supplemental tables.
Patient 1 self-reports as “short” (154.1 cm), has progressive bilateral sensorineural hearing loss and has good word recognition with hearing aids, hypernasal speech due to mild velopalatal insufficiency, difficult to control insulin-requiring diabetes mellitus, elevated BMI (over 40), thickened skin, urinary incontinence, and sleep apnea treated with continuous positive airway pressure. She has progressive joint contractures, restrictive lung disease conferred by the progression of chest wall restriction, cervical and lumbar spinal stenosis with spinal cord compression, and chronic severe pain. Multiple fractures (from 18 months to 28 years) involved the left radius, phalanges, fifth metatarsal and right tibia and fibula, and were usually caused by minor trauma which healed well. Fracture of the fifth metatarsal on the right foot resulted from torsion of the ankle and followed by prolonged healing and surgical repair of peroneal tendon. Vitamin D deficiency was noted in adulthood (exact date unknown) and successfully treated. A recent DXA scan was normal. The onset of puberty was early with thelarche at age 8 years. Menstruation with heavy flow began at age 9 years, was irregular and ceased at age 15 years attributed to ovarian insufficiency. At age 23 years, oral contraception was used to regulate her cycle. Infertility led to five rounds of unsuccessful artificial insemination.
Recent echocardiography showed “small proximal ascending aorta of 23 mm and a small mid-ascending aorta of 26 mm.” Measurements by CTA showed a proximal descending thoracic aortic measurement of 20 mm, a mid-descending thoracic aortic diameter of 15 mm and a distal descending thoracic aortic diameter of 15 mm. Mild airway narrowing was identified and followed by the laryngology service using serial upper airway endoscopy. Mild bronchial thickening was identified by CT as well. At age 30 years, she developed frequent premature ventricular beats which were treated with metoprolol and at age 44 years, non-sustained ventricular tachycardia was detected following a stress test. Coronary CTA showed very mild nonobstructive coronary artery disease.
Despite the patient's successful employment into the fifth decade, increasing fatigue and difficulty with ambulation necessitates nearly constant medical evaluations preventing ongoing work. Her management team includes cardiology, pulmonology, orthopedic (spine) surgery, sleep medicine, pain management, and rehabilitation. To cope with increasing chronic disease, mental health and palliative care services have initiated discussion about advanced care planning.
3.2 Patient 2
The second oldest patient in our cohort is a 42-year-old woman whose past medical history, including endometrial cancer, was reported in a case series about neoplasia in Myhre syndrome (Lin et al., 2020; Lin et al., 2024). In addition to the pathogenic variant SMAD4 p.Arg496Cys, reanalysis of exome sequencing showed a pathogenic variant in PITX3, specifically, c.662_663delinsA, p.(G221Dfs*88) which explained the etiology of congenital cataracts in this patient (Table 2). From age 35 years, recurrent nephrolithiasis required multiple surgeries which provided relief in the past year. Similar to Patient 1, she experienced urinary incontinence (which improved with an implantable bladder device), obstructive sleep apnea, difficult to control insulin requiring diabetes, elevated BMI, and restrictive lung disease.
Her current weight is 68.9 kg, height is 157.5 cm and occipitofrontal circumference (OFC) is 56.5 cm (>98th percentile). Increasing orthopedic disability has resulted from spinal cord stenosis caused by progressive multi-site spondylosis with ankylosis of the cervical vertebrae which necessitated spinal surgery. Further progression intrinsic to Myhre syndrome has led to striking limitation of head and neck movement, severe contractures of large and small joints. Her habitus and truncal fat distribution resembles lipodystrophy, currently, an unclassified type (Garg, 2011), not previously noted in Myhre syndrome. Echocardiography has not shown aortic narrowing. She continues to work as a teacher.
4 RESULTS
In the 14 supplemental tables that report organ system and features, 47 patients with Myhre syndrome are classified by SMAD4 variant and current age. In addition to the data collected systematically, infrequent information is discussed in footnotes and/or text.
4.1 Descriptive epidemiology
In the absence of population-based epidemiology, we used the number of Massachusetts residents followed in the MGH clinic cohort as a crude proxy for cases within the state given the presence of our unique program. We estimate that the minimum prevalence of Myhre syndrome in Massachusetts based on five (in our cohort) patients per seven million (state population), for approximately one per 1.4 million, consistent with ultrarare diseases (Smith et al., 2022).
Of 47 patients studied, four (9%) were previously reported (cited in chronologic order as patient 24 in Michot et al., 2014, patients 1 and 4 in Lin et al., 2016; patient 1 in Lin et al., 2020; Alape et al., 2020, patient 4 in Starr et al., 2022; patient 2 in Cappuccio et al., 2022, patient 15 in Starr et al., 2022) and characterized in greater detail in this review. Follow-up (defined as an in-person visit, medical record review and/or virtual visit) included 38 (81%) patients seen at least twice and 22 (47%) who were evaluated three or more times. Five (11%) patients lived outside of the United States with one each from the United Kingdom (seen only as a virtual visit with no follow-up) and South America, and three from Canada. During a virtual visit, a modified video exam was based on multiple photographs provided by the family (including face, full body, body parts) and the video encounter itself (e.g., asking the patient to speak, interact with parents and/or examiner, move around). During the 2020–2021 COVID-19 pandemic, three (6%) patients were seen only as virtual visits with medical record review.
Mean age at diagnosis was 8.3 years (median 5.0 years), with 8 (17%) currently older than 18 years and the majority female (55%).
Longitudinal data were available for 46 (98%) patients. There were two (4%) deaths, both of whom had been reported in several publications. Briefly, a 32-year-old male had a history of pericarditis requiring pericardial stripping, severe progressive multilevel airway occlusion extending from the choanae to bronchi, severe contractures, and restrictive thorax (patient 4 in Lin et al., 2016; Alape et al., 2020; patient 4, table 1 in Starr et al., 2022). An 8-year-old boy had tetralogy of Fallot (TOF) and major aortopulmonary collateral arteries (MAPCAs) palliated in infancy with unifocalization of the collaterals, followed by complete repair at age 11 months with pericardial stripping. His course was complicated by progressive pulmonary hypertension and restrictive cardiomyopathy (patient 2 in Cappuccio et al., 2022, patient 15 in Starr et al., 2022). Postmortem examinations were not performed in either patient. We reviewed nine previously reported deaths (Table 3) and noted that the cause was usually cardiovascular (64%) and/or respiratory (27%) failure, or complications thereof, including a 22-year-old male who died following a choking episode (McGowan et al., 2011, patient 3; Michot et al., 2014), an 8-year-old female that experienced an intracerebral bleed while on extracorporeal membrane oxygenation support with transition to comfort care (Starr et al., 2015), and a 43-year-old female with “presumed cardiac arrhythmia shortly after evaluation” (Oldenburg et al., 2015, patient 3); the cause of death was unspecified in one patient. The paucity (18%) of autopsy data led to a reliance on clinical interpretation.
| Author, year, patient number (previous reports) | Pt. No. | Sex | Age at death (yrs) | SMAD4 protein varianta | Airway, lungs | Cardiovascular | Joint stiffness | Surgery, procedures | Autopsy |
|---|---|---|---|---|---|---|---|---|---|
Current study (Lin et al., 2016, pt. 4) (Alape et al., 2020) (Starr et al., 2022, pt. 5) |
1 | M | 32 | Ile500Val | Multilevel airway stenosis with extensive fibrosis (COD) Restrictive thorax |
Pericarditis with pericardial effusion. High origin of coronary arteries |
Severe | Pericardial stripping. Serial balloon dilatation of airways |
No |
Current study (Cappuccio et al., 2022, pt. 2) (Starr et al., 2022, pt. 15) |
2 | M | 8 | Ile500Val | Restrictive thorax | TOF, MAPCAs. Mediastinal fibrosis. RCM (COD) |
Severe | Unifocalization of MAPCAs and central shunt. Severe peritoneal adhesions |
No |
| Cappuccio et al., 2022 | 1 | F | 17 | Ile500Val | Mediastinal fibrosis | TOF RCM (COD) |
Severe | Repair of TOF | No |
| Starr et al., 2022 | |||||||||
| (Starr et al., 2015, pt 3) | 1 | F | 26 | Ile500Val | Restrictive thorax (interstitial, pleural, and subpleural fibrosis) | Progressive AoV stenosis and LV hypertrophy. RCM (COD) |
Severe | AoV balloon valvuloplasty (twice) | Yes |
| (Starr et al., 2015, pt. 1) | 2 | F | 8 | Ile500Thr | Recurrent choanal stenosis. Possible restrictive lung disease |
ASD secundum. Polyvalvar dysplasia, progressive AoV and MV stenosis (fibroelastic thickening and fibromyxo-matous degeneration), multiple levels, with LV hypertrophy. Severe COA. Mediastinal fibrosis. RCM (COD). |
Moderate | Balloon aortic valvuloplasty (twice). Surgical AoV replacement and TV repair. Pacemaker placement. Heart transplantation |
No |
| (Oldenburg et al., 2015, pt. 4) | 4 | F | 25 | Ile500Val | Subglottic and tracheal stenosis. Interstitial lung disease (nonspecific interstitial fibrosis) (COD). Abnormal pulmonary arteries and veins with intimal proliferation and medial hypertrophy. |
RV hypertrophy and dilatation. MV perforation Abnormal cardiac myocyte morphology. Small aorta. |
Not stated | Palatoplasty for velopharyngeal insufficiency. | Yes |
(Whiteford et al., 2001) (McGowan et al., 2011) (Le Goff, Mahaut, Abhyankar, et al., 2011; Le Goff, Mahaut, Wang, et al., 2011) (Michot et al., 2014) |
9 | M | 22 | Ile500Met | Restrictive lung disease, “bronchiolitis obliterans” (COD) | PDA Peripheral pulmonic stenosis |
Not stated | No | |
| Yang et al., 2022 | 7 | F | Child-hood | Ile500Val | “Pleurisy” | VSD | Yes | Not stated | No |
| 8 | F | Early adolescence | Ile500Val | “Respiratory insufficiency” Laryngeal stenosis. “Pleurisy” |
ASD. Vascular stenosis, NOS Pulmonary hypertension (COD) |
Not stated | Not stated | No | |
| (Michot et al., 2014) | 10 | M | Late adolescence | Ile500Val | Septal defects NOS. AoV stenosis Mesenteric ischemia (COD). |
Not stated | Not stated | No | |
| Vadeboncoeur & McHardy, 2018: Pt. 7 | 1 | M | 7 | Ile500Thr | COA, AoV stenosis. RCM, pulmonary hypertension (COD)b |
Yes | Coarctation repair. Balloon angioplasty of recoarctation. | No | |
| Total 11 | F 6 (54%) | Mean (n = 8) 18 yrs |
Ile500Val 8 (73%) Ile500Thr 2 (18) Ile500Met 1 (9) Arg496Cys 0 |
10 (91%) COD 3 (27) |
10 (91%) COD 7 (64) |
7 (64%) | 6 (54%) | 2 (18%) |
- Abbreviations: AoV, aortic valve; ASD, atrial septal defect; COA, coarctation; COD, cause of death; F, female; M, male; MAPCAs, major aorto-pulmonary collateral arteries; MV, mitral valve; PDA, patent ductus arteriosus; Pt, patient; RCM, restrictive cardiomyopathy; RV, right ventricular hypertrophy; TOF, tetralogy of Fallot; TV tricuspid valve; VSD, ventricular septal defect; yrs, years.
- a In addition to the SMAD4 protein variants (p.Ile500Val; p.Ile500Thr; p.Ile500Met) listed above, the respective nucleotide variants were c.1498A > G; c.1499 T > C, and c.1500A > G.
- b Suspected as the primary cause of death based on clinical review (COD).
All patients manifested some degree of Myhre syndrome features, although there was a broad spectrum of the facial, cardiovascular, cognitive, and social ability phenotypes. Only a minority (26%) of patients had a “severe” feature (as defined above) which included restrictive cardiomyopathy, pericardial disease requiring catheter treatment or surgery, severe left-sided CHDs, TOF, and/or progressive airway obstruction (Table 4).
| Severity | Pts (%) |
|---|---|
| I. No severe features | 35/47 (74%) |
| II. Severea features | 12b/47 (26%) |
| Restrictive cardiomyopathy | 2 (4%) Ile500Val (2) |
| Pericarditis or pericardial effusion requiring catheter treatment or surgery | 3 (6%) Ile500Val (2), Ile500Thr (1) |
Left-sided cardiac outflow defects
|
10 (21%) Ile500Val 5 Ile500Thr 3 Arg496Cys 2 |
| Tetralogy of Fallot with MAPCAS | 1 (2%) Ile500Val |
| Multilevel airway stenosis requiring tracheostomy, balloon dilatation, or other procedure | 1 (2%) Ile500Val |
- Abbreviations: CHD, congenital heart defect; MAPCAs, multiple aortopulmonary collateral arteries; pts, patients.
- a Severe features required, or may need in the future, surgical or other invasive treatment, or if the feature has been established as a risk factor for mortality in the general population.
- b Total does not equal 11 since 3 patients had more than one abnormality.
Mean maternal and paternal ages at delivery were 32 years and 37 years respectively. Five (11%) patients were conceived with the assistance of in vitro fertilization (IVF) or intrauterine insemination (IUI). Twinning was overrepresented in this series. Of five (11%) pairs, three had the Ile500Val variant and two had the Arg496Cys variant. All pairs were dizygotic and involved a female co-twin with an unaffected male co-twin and were associated with IVF in two (40%) and IUI in one (20%).
4.2 Genetic analyses
Exome sequencing was the most common diagnostic test, followed by targeted gene panels for autism/ID, hearing loss, targeted SMAD4 analysis, cancer screening panel, and genome analysis were performed in one each (Table 2). Compared with our initial series (Lin et al., 2016), more patients were diagnosed using exome sequencing (34, 72%). The most common SMAD4 pathogenic variant involved p.Ile500Val (23, 49%), followed by p.Arg496Cys (18, 38%), p.Ile500Thr (5, 11%), and p.Ile500Leu (1, 2%); there were no patients with the variant p.Ile500Met. Co-occurring pathogenic sequence variants associated with a second genetic disorder (“dual diagnosis”) were noted in three (6%) patients, and a coexisting chromosomal translocation was detected in one (2%) patient (Table 2). Seventeen (36%) patients had a variant of unclear significance or copy number variant, in addition to the SMAD4 pathogenic variant (data not shown). Patients had various common genetic “first tier” tests, mitochondrial, targeted gene panel testing, and/or also, targeted single gene analyses before confirmatory DNA-based genetic testing.
Genotype–phenotype analyses were performed on selected features when the number of patients was 10 or more. Compared to the SMAD4 Ile500Val variant, patients with the variant p.Arg496Cys showed no difference regarding the frequency of any CHD, moderate/severe aorta hypoplasia, abnormal sleep, constipation, precocious puberty, keratosis pilaris, keloids, macrocephaly, astigmatism, contractures, or brachydactyly. Comparing patients with the SMAD4 Ile500Val to those with the Arg496Cys variant, significant differences were noted among patients with any CV abnormality (0.96 vs. 0.50, p-value <0.001), any hypoplasia (0.78 vs. 0.28, p-value <0.001), any arterial abnormality (0.78 vs. 0.33, p-value 0.003), hearing loss (0.48 vs. 0.17, p-value 0.037), short stature more than 2 standard deviations (SD) below the mean (0.96 vs. 0.33, p-value <0.001), sacral dimple (0.78 vs. 0.17, p-value <0.001), hyperopia (0.65 vs. 0.33, p-value 0.044), and stiff joints (1.0 vs. 0.83, p-value 0.043). In each case, the Ile500Val patients showed greater phenotypic involvement than p.Arg496Cys patients.
The significance of the Ile500Thr variant in predicting overall severity could not be assessed because of the small (n = 5) number of patients. However, severe or unusual features with this genotype included moderate–severe aortic obstruction (3, 60%), duodenal obstruction (2, 40%), and one each with severe pericardial disease and malrotation. The single patient with the p.Ile500Leu variant has normal cognitive abilities with no ASD as an adult, although she reported social disability through adolescence.
4.3 Cardiovascular abnormalities
All patients had echocardiography performed at MGH except for three patients evaluated virtually during the COVID-19 pandemic for whom echocardiography and cardiology consultation(s) were performed at their home institution (Supplemental Table 1). Complete aortic imaging by CTA was performed to delineate the entire aorta in 36 (77%) of all patients with 29 (62%) completed at MGH and seven (15%) at a home institution. As noted on Supplemental Table 1, 36 (77%) of all patients had at least one type of cardiovascular abnormality, emphasizing the importance of SMAD4 in cardiovascular biology. CHDs were present in 22 (47%) patients which included atrial and/or ventricular septal defects (n = 4), patent ductus arteriosus (PDA) (n = 6, isolated in 2), pulmonic valve stenosis (n = 2), various levels of left heart obstruction (n = 10), aberrant right subclavian artery (n = 2), and one each with TOF, anomalous coronary artery, and sub-aortic membrane. One child had multiple levels of left-sided obstruction. Increased left ventricular (LV) trabeculations with preserved systolic function were noted in 8 (17%) of patients but did not meet echocardiographic criteria for LV noncompaction cardiomyopathy (Monda et al., 2024).
Cardiovascular surgery or interventional catheterization was performed in eight (17%) patients. Five (11%) patients underwent surgical PDA ligation, including one patient who first underwent an unsuccessful Amplatzer® device closure. The patient with TOF and multiple aortopulmonary collaterals underwent standard staged surgery (Cappuccio et al., 2022), and was included with other patients in that report who had various neural crest-derived anomalies.
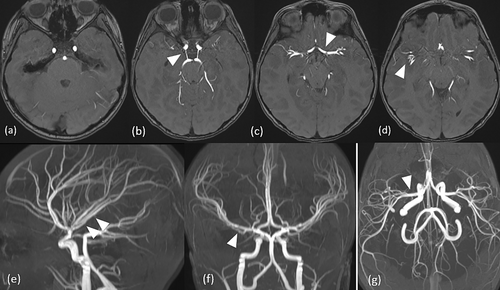
Long segment aortic hypoplasia was present in 28 (60%) individuals. It was mild in 18 (38%) and moderate–severe in 10 (21%), which included the four patients with coarctation (Figures 1 and 2). These four subjects underwent relief of severe aortic arch obstruction in infancy at their home institutions. Of note, none had simple discrete juxtaductal involvement. Instead, all had diffuse narrowing of the aortic arch and measurable obstruction (>15 mmHg gradient on four extremity blood pressure). One female had subclavian flap augmentation of the aortic arch via thoracotomy and later underwent end-to-end anastomosis after re-coarctation. Another female had end-to-end anastomosis and near occlusion at the site of the re-coarctation. Postoperative cardiac catheterization showed long segment coarctation beyond the region which could be reached surgically (20–30 mmHg gradient). Balloon angioplasty resulted in an enlarged aorta, but unchanged gradient. A third female had an end-to-end anastomosis, followed by balloon angioplasty 3 months postoperatively. A fourth male patient had subclavian flap repair performed when end-to-end anastomosis could not be achieved, and which was followed by balloon dilatation of re-coarctation 7 months postoperatively. In three patients, the aortic wall was reported by the surgeon to be thickened, although histology is not available. It is notable that all four patients who had coarctation repair needed reintervention for re-coarctation. Balloon dilatation of various levels of the aorta were unsuccessful as the initial treatment but was useful when applied after surgery. Two patients with aortic reconstruction had mild postoperative aortic root dilatation.
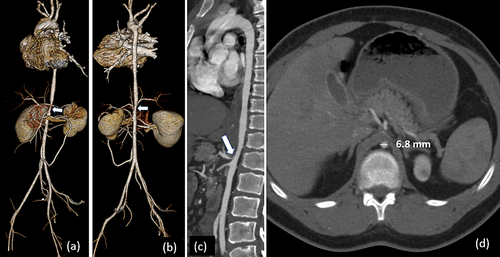
One additional patient had aortic obstruction below the thoracic region. As a 9-year old (now 21-year-old), this male with the SMAD4 variant p.Ile500Thr had a CTA at an outside hospital which showed a 7 cm narrowed portion of the abdominal aorta beginning just below the diaphragmatic hiatus to below the level of the renal arteries resulting in a 50 mm gradient, with proximal stenosis of the superior mesenteric artery. Balloon angioplasty using cutting balloons on this long segment narrowing was performed twice at a pediatric cardiology center with mild reduction in pressure gradient, but systemic hypertension persisted. No further intervention was attempted.
A predisposition to hypoplasia of the aorta and left heart structures as a fetal developmental anomaly was suggested in two patients where fetal echocardiography noted a discrepant right and left ventricle size. In both fetuses, mitral and aortic annular hypoplasia and arch hypoplasia were noted, as well as a hypoplastic, but apex-forming left ventricle. The families were counseled regarding likely arch repair and the possibility of single ventricle palliation. The mothers each delivered at a tertiary pediatric hospital, and in both, postnatal echocardiography confirmed hypoplasia of multiple left sided structures. Both infants initially required only arch repair and were reported to have subsequent growth of the left ventricle.
Additional arterial anomalies included six (13%) patients with renal artery stenosis, five of whom were among those with moderate/severe aorta hypoplasia. In one boy with no underlying structural defects or aortic obstruction, CTA detected subtle nonobstructive intimal flaps involving the renal arteries, and possibly the splenic arteries, consistent with possible dissection.
Pericardial disease was noted in six (13%) patients, four of whom had self-limited pericardial effusion, and two patients had severe pericardial disease with constriction treated with pericardiocentesis, pericardial window or stripping, or pericardiectomy; one boy had the pericardium removed at the time of his TOF surgery. Traditional pharmacologic measures to treat pericarditis included nonsteroidal anti-inflammatory drugs (NSAIDs). High dose prednisone and colchicine were also used (two patients each) but did not have a measurable impact.
Restrictive cardiomyopathy without pericardial disease was noted in two patients each of whom had an associated abnormality, that is, unrepaired descending aortic hypoplasia in one patient, and TOF with MAPCAs in the second. The former is a now 26-year-old woman who was reported in detail (Lin et al., 2016) and who developed protein losing enteropathy (PLE) at age 15 years, which has been well-managed over the last 11 years with attentive fluid management, diuretics, and budesonide. Pulmonary hypertension was not consistently evaluated in our series, but was present in the two patients with restrictive cardiomyopathy, one as isolated cardiomyopathy and another associated with repaired TOF (treated with sildenafil); a third child had transient pulmonary hypertension.
Coronary atherosclerosis was noted in two patients by coronary CTA at ages 37 and 50 years (Cury et al., 2022). Of note, coronary CTA was not systematically performed. Patient 2 in the clinical summaries had significant coronary atherosclerosis on gated cardiac CTA performed at age 37-years involving severe stenosis of the posterior LV branch arising from a dominant right coronary artery. Exercise testing on the same date demonstrated no specific signs of ischemia (77% of age-predicted maximum heart rate). Subsequent cardiac MRI at another institution demonstrated no significant abnormalities in delayed gadolinium enhancement, suggesting no prior ischemic myocardial injury. This patient has a history of insulin requiring type II diabetes—associated with increased BMI likely contributing significantly to premature coronary atherosclerosis. Lack of demonstrable myocardial ischemia may be secondary to collateral supply to the territory supplied by the affected coronary branch. Another patient had minimal coronary atherosclerosis noted incidentally on coronary CTA performed at 50 years of age at another institution.
4.4 Ear, nose, throat, and upper airway features
Almost half (47%) of patients were evaluated by the MGH ear, nose and throat (ENT) specialist, and an audiogram was reviewed in 28% (Supplemental Table 2). Hearing loss, present in 18/47 (38%) of all patients, was usually conductive or mixed; one patient had isolated sensorineural hearing loss. Hearing loss was always bilateral, and in those with hearing loss, it was stable in 3/18 (17%) and progressive in 6/18 (33%); information was unavailable in 9 (50%). Inner ear anomalies were noted in 9/47 (19%), 8 of whom had hearing loss. Habilitation included hearing aids in 10/18 (56%) and bone-anchored hearing aid (Baha) in 3 of 18 (17%). Because ENT follow-up is pending in a substantial additional one-third of all patients, these figures may increase in the near future.
Most (77%) patients with Myhre syndrome had recurrent otitis media, and 55% required pressure equalization (PE) tubes. Cerumen in Myhre syndrome was usually copious and often mixed with keratinaceous debris requiring frequent ear cleaning. The most extreme example was a boy with Myhre syndrome and co-occurring ichthyosis whose bilateral hearing loss normalized after cleaning “plugs” of debris under anesthesia. Cleft lip and palate were present in one, submucosal cleft with velopharyngeal insufficiency (VPI) in two, and isolated VPI in nine patients.
Laryngotracheal defects in six patients included four with mild sub-glottic stenosis which was suspected after intubation when stridor was reported. None progressed either as a clinical symptom (stridor) or after additional intubation for a subsequent procedure. One toddler male had a very small mouth with reduced opening and short aryepiglottic folds. A young adult male was noted as an adolescent to have tonsillar hypertrophy with limited view of glottis and retroflexed epiglottis which also obstructed view and did not allow intubation; the trachea was normal.
Striking airway pathology in a seventh patient included multilevel airway stenosis which began in this male at 8 years of age with progressive nasal obstruction following adenotonsillectomy and myringotomy tubes for recurrent otitis media. CT scan at age 10 years demonstrated complete closure of the posterior nasal cavity and surgery was performed at age 14 years to relieve complete bilateral choanal and nasopharyngeal stenosis. Surgery was repeated a few months later for choanal atresia, additionally including the trachea and which failed to improve the respiratory problems necessitating tracheostomy at age 24 years. At age 25 years, targeted gene analysis confirmed a pathogenic SMAD4 Ile500Val variant consistent with Myhre syndrome. He required serial balloon dilations until his death at age 32 years (Alape et al., 2020; Lin et al., 2016; Starr et al., 2022); postmortem examination was not performed.
4.5 Pulmonary features
Seventeen patients were able to complete spirometry; all (17/17, 100%) were found to have spirometric restriction (decreased Forced Expiratory Volume, FEV and/or Forced Vital Capacity, FVC with normal FEV1/FVC), with a mean FVC of 57.2% predicted (SD 14.4) (Supplemental Table 3). Two patients underwent oscillometry testing, which demonstrated increased resistance at 5 and 20 Hz and increased reactance. A CT scan of the chest was obtained in over half (32, 68%) of patients, and showed regional/segmental differences in attenuation consistent with air trapping mosaic attenuation in seven (22%). In addition to the spirometry findings, physical examination by the geneticist or pulmonologist noted restriction of the thorax (by either observation of a stiff chest wall or reduced inspiration) in all 17 and in at least one additional patient.
Asthma (sometimes reported as reactive airway disease) was noted in 36% of all 47 patients, with bronchodilator responsiveness in five of seventeen (29%) tested.
In our program, sleep was evaluated by several specialists, but consistently by the pulmonologist because of the possible role of an obstructive airway in sleep-disordered breathing. Obstructive sleep apnea (OSA) was reported in 16 (34%). Thirty-one patients (66%) had disordered sleep treated with trazodone, suvorexant, ramelteon, and melatonin (over-the-counter) in 15%, 2%, 2% and 11%, respectively. Medication reporting reflected its use at any time in the course of reporting. Nine (19%) patients had restless leg syndrome and/or periodic limb movement disorder. Until recently, iron deficiency anemia was not consistently evaluated as a risk factor for sleep dysregulation, and the results of laboratory testing obtained by the primary care provider (PCP) were not always available. However, we noted low ferritin in at least 4 (9%) and anemia in at least 8 (17%) patients, usually associated with heavy menstrual periods or prematurity. Iron replacement therapy was instituted in 19 (40%) patients either empirically or based on abnormal testing.
4.6 Gastroenterology
Constipation was a nearly universal complaint in Myhre syndrome (Tabbers et al., 2014) (Supplemental Table 4). In some patients, constipation was severe enough to require bowel “clean out” at home or in the hospital. Many of these patients also had fecal incontinence and toileting delay (typically bowel). Medication for constipation and/or reflux was used in 27 (57%) including polyethylene glycol, bisacodyl, senna, and omeprazole. One boy received botulinum toxin injections for severe constipation due to functional outlet obstruction.
Patients also experienced feeding difficulties, most commonly a selective diet as “picky eaters.” Poor weight gain was common in infancy and young childhood. Short stature (more than 2SD) was common which resulted in a normal BMI since height and weight were proportional. Twelve (26%) patients had dysphagia, and abdominal pain of any type was reported in 19 (40%).
Gastrointestinal procedures included liver biopsy (two), colonoscopy (five), and endoscopy/esophagogastroduodenoscopy (13); during scoping procedures, biopsies were usually obtained. Additional surgical procedures not listed in Supplemental Table 4 were performed in two patients who developed postoperative adhesions consistent with abdominal serositis. An adult male (SMAD4 Ile500Val variant) with multilevel airway stenosis had ischemic enteritis, small bowel resection and re-anastomosis complicated by pneumatosis coli and mesentery fibrinopurulent serositis. An adult female SMAD4 p.Arg 496Cys had laparoscopic appendectomy complicated by lysis of adhesions, and 10 years later, was found to have severe pelvic adhesions at the time of myomectomy for uterine fibroids. Two patients who had major gastrointestinal surgery did not develop adhesions. These include Patient 2, the adult female (SMAD4 p.Arg496Cys) treated for endometrial cancer with hysterectomy and bilateral salpingo-oophorectomy, accompanied by ileocecal resection and hemicolectomy and an infant male (SMAD4 p.Ile500Thr) with malrotation of the small intestine repaired with the Ladd procedure, appendectomy repair and duodenojejunostomy.
“Fatty liver” was reported in two patients and nonalcoholic steatohepatitis (NASH) in an additional three patients with onset in the second, fourth and sixth decade. An additional three children who had gastrointestinal issues had elevated liver function tests (LFTs) identified as part of chemistry panels. Self-limited hypoalbuminemia developed in a 10-year-old male (currently, 15 years) in the setting of recurrent pleural and pericardial effusions without a diagnosis of PLE or restrictive cardiomyopathy, but with chronic renovascular disease.
4.7 Endocrinology and gynecology
Thirty-five (74%) patients have established care with an endocrinologist at home and/or at MGH (Supplemental Table 5). Care established in early childhood was often to evaluate for short stature. Growth restriction noted in utero or at birth was reported in 53%, and short stature defined as height 2 SD below the mean for age was seen in 72%. Short stature seemed more common in youths less than 18 years with the p.Ile500Val variant (18/19, 95%) compared with the Arg496Cys variant (5/16, 31%). Short stature was associated with advanced bone age in 3/9 (33%) individuals, all of whom had the variant Ile500Val. Short stature persisted in all four individuals over 18 years with the p.Ile500Val variant and one of the two adults with the Arg496Cys variant. A few of the children had been treated with growth hormone to enhance their height, but an increase in height was not consistently documented.
Many of the patients had early or precocious puberty (Gohil & Eugster, 2020). Precocious puberty was reported in 8/26 (31%) females, and 5/21 (24%) males. Three of six (50%) female adults (one each with Ile500Val, Ile500Leu, and Arg496Cys variants) had a history of precocious puberty as did the one adult male with a p.Ile500Thr variant. Four of 12 (33%) children were treated with gonadotropin releasing hormone analogs for true precocious puberty. The mean age of menarche in eight females was 9.5 years compared to the national estimate of 11.9 (1995 through 2013–2017, Martinez, 2020).
Testicular size was not measured in all males. Seven of 21 (33%) with a mean age of 11.9 years underwent an evaluation by the MGH pediatric endocrinologist for premature puberty. Although premature adrenarche was reported in some by history, of the five examined over the age of 9 years, testicular size was appropriate for age ranging from 8 to 20 ml (Rosenfield, 2021). One boy who had required surgery for an undescended testis had one testis of 20 ml, and the other, of only 1.5 ml. Relatively early puberty starting by 11 years, was reported by families but could not be objectively confirmed in this small group.
Obesity (BMI greater than 30) was reported in six (13%) patients (three male, three female). Precocious puberty occurred with obesity in two males (one with the Ile500Val variant and one adult with Ile500Thr variant). As described in the clinical summaries, Patient 2 had adipose distribution suggestive of lipodystrophy.
Adult women with either the p.Ile500Val or p.Arg496Cys variant tended to have large breasts, menstrual dysfunction, and in several cases had been given a diagnosis of polycystic ovarian syndrome (PCOS). Given the frequency of increased body weight, and other disorders including reports of endometrial cancer and infertility one may surmise that many others likely have undiagnosed PCOS.
As noted in the clinical summaries, Patient 2 had endometrial cancer (Lin et al., 2020; Lin et al., 2024). Both Patient 1 and 2, one each with a SMAD4 p.Arg496Cys and p.Ile500Leu variant attempted pregnancy unsuccessfully before their subsequent diagnosis of Myhre syndrome.
Sex hormone medications to manage menometrorrhagia included oral contraceptive (7/26 females, 27%) and one with a hormone-eluting intrauterine device. Gynecologic surgery included in one each with myomectomy, salpingo-oophorectomy, reduction mammoplasty, oophorectomy, and omentectomy. Hysterectomy was performed in two patients for management of dysfunctional uterine bleeding.
Metabolic laboratory testing was not part of the baseline evaluation or surveillance. However, abnormal laboratory tests ordered by various providers detected a few patients with vitamin D deficiency (two), hypertriglyceridemia (one), and hypercalcemia (one).
4.8 Renal and urology
Renal scarring was noted in four (9%) patients, and chronic kidney disease in three (6%), one each with ntial intrinsic renal hypertension and two with renovascular hypertension (Supplemental Table 6). Hypertension (18, 38%) and elevated blood pressure (4, 9%) were treated in 17 (36%), 9 (53%) of whom used more than one medication over their lifetime. The most common antihypertensive medications among all 47 patients: 17 who were treated with losartan (8 patients, 17%, 47%); amlodipine (6 patients, 13%, 35%); and atenolol (5 patients, 11%, 29%).
Congenital and acquired urinary tract and genital anomalies are common in Myhre syndrome (Supplemental Table 6). Undescended testicles (38%) and hypospadias (10%) occurred more frequently than in the general population. Cryptorchidism was most common in the p.Ile500Val and p.Ile500Thr genotypes and hypospadias was observed primarily in the p.Ile500Val genotype (Supplemental Table 6). These conditions should be apparent on routine physical exam. In addition to typical operations for circumcision, hypospadias, and undescended testes, genitourinary procedures included sacral neuromodulation and bladder botulinum toxin (performed because of non-co-apting bladder neck).
Urinary incontinence defined as patients older than 4 years with daytime and/or nocturnal enuresis was reported in 26 (55%) and was common across all genetic variants. Management was difficult, rarely responding to traditional fluid management and behavioral interventions. Approximately 15% (all of those who were symptomatic) were evaluated with urodynamics. Many of these patients have difficulty recognizing bladder fullness or have an inability to voluntarily withhold urine or initiate a urinary stream. One patient underwent placement of a bladder stimulation device. Most underwent renal sonography, but significant structural abnormalities were uncommon.
Urinary tract infection was uncommon. Nearly 10% of patients had urolithiasis. Among them was Patient 2 with severe nephrolithiasis which first presented in her 30s who had an obstructing 7 mm right ureteral calculus with mild upstream ureteral dilation and wall thickening as well as a non-obstructing four mm stone within the bladder near the ureterovesical junction. Urine calcium excretion was quite high in this patient.
4.9 Dermatology
The skin in Myhre syndrome feels firm or stiff and continues to thicken over time (Supplemental Table 7). Noted even in early childhood, it is more commonly appreciated by late childhood although there are rare adolescents and adults who do not have clinically appreciable thickened skin (Lin et al., 2016; Yang et al., 2022). Keratosis pilaris is another hallmark cutaneous finding of Myhre syndrome. Unlike what is commonly seen in the general population, this “bumpy skin” is more widespread anatomically affecting chest, back, legs (in addition to the usual upper arm involvement). Additionally, the keratin plugs clinically appear thicker. Due to the high degree of comorbid autism spectrum disorder diagnoses, which commonly results in sensory atypicalities, many patients and their families find topical treatments difficult. Because the keratosis pilaris is often asymptomatic, and patients may be reluctant to use topical medications, it is not known if the keratosis pilaris is more recalcitrant to treatment.
Abnormal scarring is also commonly seen, ranging from hypertrophic scars after surgery to thin hypopigmented linear scars secondary to routine activities that in most individuals would not leave behind any scar. Subcutaneous nodules were noted in three patients in various locations. Most were small (the largest measured was 2.7 cm). A male patient had a mass over his left shoulder region that was resected at age 2 years which showed fibro-histiocytic proliferation. At age 16 years, he developed a compressible mass on the dorsum of the right foot which was not an exostosis, but was diagnosed by orthopedics as a benign bursa sac. Additional eruptions were noted in a boy with elbow papules which may be benign frictional lichenoid eruption, and a boy and girl with likely sterile folliculitis on the buttocks and posterior legs.
4.10 Brain and spinal cord
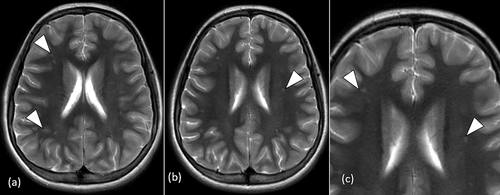
Subtle radiological findings such as thickened calvarium (11%) or white matter injury (WMI), described by some as white matter hyperintensities, were likely under-ascertained (38% of all patients, 53% of those who were imaged) (Supplemental Table 8). Because imaging was not part of our protocol, there was variable testing and likely underreporting. Medical record abstraction was supplemented by review of the actual radiological studies (CT or MRI) in 22/34 (65%) of those who had imaging.
The age-matched head circumference was generally larger (38/47, 81%) compared to expected measurements based on height, with absolute macrocephaly defined as OFC more than 3SD from norm was noted in only one female. Thus, 37 (79%) patients had “relative” macrocephaly. A few (3/47, 6%) patients had microcephaly (less than 3 SD). Major brain malformations were infrequent except for two toddlers with a Chiari malformation. One girl required decompressive neurosurgery at a home institution, and postoperative imaging suggested the development of a syrinx. Corpus callosum anomalies (including hypoplasia or dysplasia) were noted in 21% of patients.
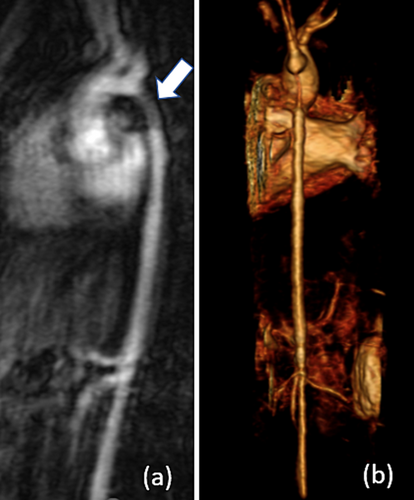
We identified neurovascular phenotypes in subjects with available brain and cerebrovascular imaging consisting of a large vessel arteriopathy having decreased tortuosity, branching abnormalities (9/9, 100%) (Figures 3 and 4) and small vessel disease (18/34, 53%). Cerebral small vessel disease patterns included T2-weighted/FLAIR WMI, prominent perivascular spaces and consistent with lacunar ischemic infarcts. In this limited cross-sectional study, we did not find significant associations between large or small vessel disease and brain malformations, atrophy, age, and the diagnosis of intellectual disability (ID) or ASD (Figure 4). In 12/34 (35%) patients, we did not have access to the actual studies and relied on reports.
Caudal spinal cord pathology was clinically suspected by a deep sacral dimple (55% of all patients) or deep gluteal crease (13%), and radiographically, by sacralization of L5 (28%), platyspondyly (19%), and/or coccygeal anomalies (17%). Subsequent spinal cord MRI imaging (24/47, 51%) as well as incidental detection on chest CT (36, 77%) identified a low-lying conus in eight (17% of all patients, 33% of those imaged by any modality) and a filar lipoma was noted in seven (15% of all patients). Symptoms such as toe walking and stool or urine incontinence commonly associated with spinal cord dysfunction are likely to have a behavioral contribution (ASD) and autonomic dysfunction derived from WMI. Tethered cord release was performed to prevent progression on four patients at MGH and three patients at outside hospitals. An eighth patient with SMAD4 p.Ile500Thr has both clinical and radiological findings of tethered cord and is being monitored for future surgical intervention. Spinal stenosis was present in three symptomatic adults, and in one female child whose imaging was performed for tethered cord which also detected the stenosis. Surgery was performed in two adult females and a favorable outcome occurred in Patient 1, whereas Patient 2 did not have relief from spinal cord compression.
4.11 Ophthalmology
At least one ocular (including visual and structural) abnormality was noted in 43 (91%) of patients (Supplemental Table 9). Refractive error was common and included astigmatism (64%), hyperopia (55%), and myopia (13%). In patient with strabismus, esotropia was most common (19%), and exotropia occurred less frequently (4%). Amblyopia was reported in 11%. Disorders of the lacrimal system were reported in 45%. Optic nerve abnormalities were observed in 36% which were characterized by others as blurred disc margins or “pseudopapilledema.”
Cataracts were noted only in Patients 1 and 2. The age of onset in the oldest patient was 50 years and her examination was consistent with age-related cataracts. In the second patient, cataracts presented in her second decade with subsequent removal of bilateral polar cataracts. She was later found to have a likely pathogenic variant in the PITX3 gene which is associated with cataracts (Semina et al., 1998).
4.12 Immunology
A comprehensive immunology consult at MGH was completed in eight patients (Supplemental Table 10). IgM levels were normal in all eight (100%) patients. Three (38%) patients required additional vaccination to further assess for specific antibody deficiency. Prophylactic antibiotics were prescribed for two patients. IgG2 was low in one patient and borderline normal in another, while an IgG1 deficiency was observed in an additional patient. IgG4 was elevated in one patient.
An additional 13 patients had immunology evaluations with variable lab testing (most commonly, quantitative immunoglobulins) at outside institutions, seven (54%) of whom had hypogammaglobulinemia, all (7/7, 100%) with low IgG for age and 3/7 (43%) with low IgA. One patient with hypogammaglobulinemia had PLE (Lin et al., 2016), and required additional vaccinations to further assess for specific antibody deficiency. She received IgG infusions. Then, 2 of 13 (15%) patients had elevated IgA and one patient had unspecific elevated immunoglobins.
While mild infections were noted, including recurrent otitis media, sinusitis, and mastoiditis, there were no severe, invasive, or atypical infections; sepsis was present in one patient secondary to dental infection.
4.13 Craniofacial and dental
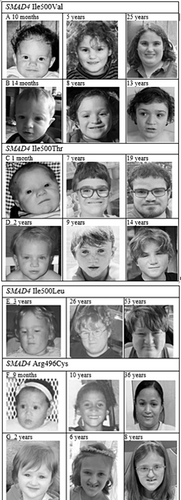
Measurement of facial features was attempted early in the study but was not feasible for many children with neurodevelopmental and behavioral disabilities. The OFC was obtained in all patients and ear length in many (Supplemental Table 11). The characteristic facial appearance of Myhre syndrome (i.e., short palpebral fissures, mid-facial hypoplasia, short philtrum, narrow mouth, thin upper lip, small ears, prominent nasal tip) was noted in all except one woman. A prominent chin, often characterized as prognathism when severe, was noted in 35 (74%) patients, 7 (20%) of whom had severe involvement. Five (11%) patients were referred to the oral maxillofacial surgeon for evaluation of restricted mouth opening (two), prominent chin (two), and impacted wisdom teeth which were later removed (one). No patient required orthognathic surgical intervention. Figure 5 shows that the facial features generally changed over time but are similarly mild in children younger than 3 years.
One patient had repair of cleft lip and palate, and two patients had unrepaired submucosal cleft. In addition to these three patients, nine (19%) had VPI which was managed with speech therapy.
4.14 Musculoskeletal, including physical therapy
A complete skeletal survey was performed in 14 (30%) (Supplemental Table 12). We noted that minor anomalies of the fingers and toes including brachydactyly (30, 64%), clinodactyly (33, 70%), camptodactyly (8, 17%), syndactyly of toes 2 and 3 (31, 66%), and overlapping toes (8, 17%). There were 11 ribs in 23 (49%) patients, fractures in 13 (28%), scoliosis in 10 (21%), and exostoses in 16 (34%). Additional minor, infrequent abnormalities are reported in the footnote of Supplemental Table 12.
Leg pain (usually involving the calf) was reported in 12 (26%), stiff joints with an abnormal gait in 44 (94%) and severe contractures (diffuse arthropathy) in 5 (11%) with less severe contractures (stiff joints) in 23 (49%). A PT evaluation was performed at MGH in 38 (81%) and addressed patient mobility, exercise tolerance, progression of contractures (noted at the earliest in a 26-months-old female) and participation in activities. The familiar abnormal “stiff” gait was defined by the lack of heel strike, upper body rotation and arm swing, short steps, externally rotated hips and out-toeing feet. Walking and running on toes was noted. The 6-min walk test was performed in 9 of 38 (23%) to measure functional status and aerobic capacity but was not widely administered due to limitations in participation. Distances walked in the 6-min walk test were less than the predicted distances for all patients based on age, height, weight and gender. Then, 2 of the 9 (22%) patients walked distances in the low end of the normal range based on their age and gender and 7 (78%) walked distances below the normal range (Enright & Sherrill, 1998; Geiger et al., 2007). The degree of joint limitations was assessed by measuring the popliteal angle in 30 (79%) patients, dorsiflexion in 17 (45%) and shoulder flexion in 20 (53%). These measurements were established as a baseline to monitor progression of contracture. Follow-up was possible in 14 (30%) patients, but the rate of progression of contracture as well as the impact of physical therapy (PT) is unknown. Compliance with therapy and home programing was inconsistent.
4.15 Developmental, neuropsychological, and psychiatric issues
The majority (70%) of patients with Myhre syndrome had neuropsychological testing at least once, and 26% had been evaluated by a psychiatrist (Supplemental Table 13). Nearly all patients experienced developmental delays in multiple domains.
The diagnosis of intellectual disability (ID) (32%) required assessment of cognitive assessment and adaptive functioning, but data were insufficient to categorize the severity of ID. Academic accommodations (including a 504 educational plan or Early Intervention Program) were reported in 44 (94%) of all patients. Nearly all (91%) patients had significant social challenges reported by parents or providers. The majority (72%) met full diagnostic criteria for autism spectrum disorder (ASD) per the medical record. The social presentation in Myhre syndrome is complex and includes difficulty engaging with peers, lack of friends and/or understanding social cues.
The most common psychiatric comorbidities included attention-deficit/hyperactivity disorder (ADHD) (53%) and anxiety disorders (40%). It appears that ADHD may be undertreated, as only 15% of patients ever received psychopharmacologic treatment for ADHD. Mood disorders and obsessive–compulsive and related disorders were rarely observed. Sleep dysregulation was discussed in Section 4.5.
4.16 Neurologic features
Epilepsy was diagnosed in four (8%) patients, three of whom (all with the Arg496Cys variant) are taking an anti-seizure medication including lamotrigine and levetiracetam (Supplemental Table 14). In an additional nine (19%) patients, there were seizure-like movements (e.g., tic-like, tonic movements, staring spells) for which the EEG was normal or not obtained.
5 DISCUSSION
The ideal natural history study for a rare disorder would begin on the first day that a patient is evaluated at a syndrome specific center with unlimited clinical and research support, and offering easy access to people of diverse geographic, socioeconomic, and racial backgrounds. Technically, “natural” history refers to organ systems that have not been subjected to treatment, and instead, “clinical” history is more accurate (Pyeritz, 2019). Like others (Garavelli et al., 2016; Yang et al., 2022), we use “natural” history since patients with Myhre syndrome often require lifesaving surgery and medical treatment.
In the absence of data obtained from evidence-based guidelines, we omitted multivariable analyses in favor of descriptive data that included self-reported (patient or parent) data. The specialists in our clinic followed relatively standardized evaluations which were modified over the years to accommodate younger patients, challenging neurobehavioral phenotypes (ASD, ADHD, ID), and the reality of time-limited visits. Photographs taken in clinic or taken at home allowed subjective assessment (Figure 5). Certain tests were not obligatory at this time, which may change if this study contributes to future evidence-based guidelines. Skeletal survey or brain MRI imaging was generally performed by referring primary or specialty providers, we increasingly performed brain MRI/MRA at our center when intracranial vasculopathy was recognized in this cohort. Early in the study, we recognized the necessity of detailed imaging of the aorta and added CT angiography as part of the cardiovascular evaluation. Airway evaluation with nasoendoscopy may be needed to assess airway diameter and changes over time.
5.1 Descriptive epidemiology
Not surprisingly, patients with an ultrarare syndrome may be reported by previous authors. In our prior review, there were four new patients, two of whom (patients 1 and 4) (Lin et al., 2016) are included in current research. To enhance consistency of this current research, we did not include cases from the literature. The estimated prevalence of one per 1.2 per million is likely an underestimate considering the likely scenario of patients who remain undiagnosed, or not referred to the MGH clinic. Fetal diagnosis (Rodríguez et al., 2024) will likely increase in the future and those that result in termination of pregnancy (Hui et al., 2023) would reduce the live birth prevalence.
5.2 Clinical characteristics and genetic testing
With the exception of a few families with the SMAD4 p.Arg496Cys variant (Demir et al., 2023; Meerschaut et al., 2019), patients with Myhre syndrome are born to unaffected parents who do not carry the mutation. Unassisted conception has not been reported in a woman with Myhre syndrome. The Myhre syndrome phenotype can vary significantly ranging from a severely affected fetus (Hui et al., 2023) to highly functional adults. This would be further impacted by the detection of germline mosaicism (which is speculative at present). Potential disease modifier genes also influence the severity of the condition, and thus detection rate. Our genotype–phenotype was limited by the often small (<10) number of patients. We observed that patients with the variant Arg496Cys had fewer CV abnormalities of any type, less aortic hypoplasia or arterial abnormality, hearing loss, short stature, sacral dimple, hyperopia, and stiff joints. Similarly, Yang et al. (2022) reported greater severity, including deaths, in patients with the Ile500Val variant. Patient 1 is the first well-phenotyped person with Myhre syndrome due to the SMAD4 variant p.Ile500Leu. This variant had be reported in a boy with microcephaly and ID who had a co-occurring variant in WDR62 (Slezak et al., 2021). Although the published photo suggested Myhre syndrome, delineation of his phenotype has not yet been reported.
Table 2 is not an exhaustive list of every variant reported by the diagnostic labs. Future research would require parental testing and more extensive clinical correlation. Table 3 reports deaths in the literature (n = 9) and our series (n = 2). Although the frequency of SMAD4 variants is noted, this table should not be used for genotype/phenotype analysis because of possible reporting bias as we are aware of unreported deceased individuals. Table 4 notes that most (74%) patients with Myhre syndrome do not have severe features such as restrictive cardiomyopathy, pericarditis, severe left-sided cardiac outflow defects (multiple levels of obstruction, severe aorta hypoplasia), complex CHD, or multilevel airway stenosis. Importantly, three patients had more than one severe abnormality. The combination of aortic obstruction and RCM predicts higher morbidity and mortality. This classification was unable to capture other impactful features especially orthopedic limitations which should be studied in the future.
Because of the young mean and median ages (12.9 and 10 years, respectively), features such as abnormal puberty or hypertension may not have presented. We have observed changes in our older patients consistent with a progressive condition, and accordingly, medical needs may increase with age.
Formal morphometrics on physical examination were not performed consistently, and the photo montage in Figure 5 demonstrates that there is no single “Myhre syndrome facies” because of the broad phenotypic spectrum and changes with aging. Although many patients in our series were diagnosed using autism gene panels, others have been detected as part of defect-specific gene screening without prior suspicion (Wurfbain et al., 2023).
The literature reporting cardiovascular abnormalities has progressed from general reviews (Lin et al., 2016; Michot et al., 2014) to more specific reports of pericardial disease (Garavelli et al., 2016; Picco et al., 2013; Starr et al., 2015). Abnormal wound healing with an exuberant fibroproliferative response during operative procedures, including orthotopic heart transplantation for restrictive cardiomyopathy (Starr et al., 2015) poses as an enormous management challenge. Losartan is generally accepted as a treatment for hypertension, and its role in reducing fibrosis (Piccolo et al., 2014; Cappuccio et al., 2021) indicates a need for clinical trials.
Formal parental age analysis was not performed. Preconception genetic counseling generally includes a discussion about the risk for an autosomal dominant disorder increasing with advanced paternal age.
The detection of a co-occurring Mendelian or chromosome disorder is essential to determine if a feature represents expansion of the core Myhre syndrome phenotype or a distinct disorder (“dual diagnosis”) (Posey et al., 2017). For example, conductive hearing loss due to the accumulation of scale associated with ichthyosis resolves with ear cleaning and classically attributed to lamellar ichthyosis (Richard, 2023). Desquamation related to Myhre syndrome may have also contributed in our patient. Amidst great phenotypic diversity, at least two complex patterns (endophenotypes) were recognized independent of genotype. Stiff joints, stiff gait and thickened skin usually progressed to severe contractures and greatly reduced mobility. Additionally, patients with one level of airway stenosis generally progress to multilevel stenosis.
5.3 Cardiovascular abnormalities
Common cardiovascular abnormalities in Myhre syndrome include CHDs, hypoplastic aortopathy, and pericardial disease. This cohort also describes RCM and coronary artery disease. Aside from one patient in our cohort who was included in a series of seven patients with TOF (six with TOF with pulmonary atresia and multiple aorto-pulmonary collaterals, and another with TOF with absent pulmonary valve) (Cappuccio et al., 2022). CHDs were common, but typically not complex. Given the high frequency of CHDs and aortic abnormalities, fetal CHD diagnosis may be an impetus for prenatal exome sequencing which could detect Myhre syndrome. For example, an aberrant right subclavian artery, persistent left superior vena cava, thickened pericardium and mild pericardial effusion were detected in a 19-week gestational male (Hui et al., 2023). The authors suggested “possible cardiomyopathy” but did not further define. After exome sequencing performed on amniotic fluid at 23 weeks detected a SMAD4 variant Ile500Thr, the pregnancy was terminated; autopsy was not performed (Hui et al., 2023). However, the most common CHDs in Myhre syndrome, ASD, VSD, and aortic hypoplasia, are among lesions that can be challenging to diagnose in the fetus.
In one male in our cohort with severe aortic disease, the use of losartan led to an expected decrease in systolic blood pressure, but an increase in diastolic blood pressure. Further research is needed to determine the role of this medication among all patients with aorta obstruction.
At least in this series, coarctation of aorta was not present in the classic juxtaductal region. All patients who had surgical repair of coarctation had recurrent obstruction. The literature often reports coarctation without describing whether there was a shelf-like indentation or fusiform narrowing (Michot et al., 2014). Data is insufficient to correlate severity with the location of the hypoplasia (ascending, arch/isthmus, descending or abdominal aorta). Treatment may be needed to relieve postoperative systolic hypertension, but a second procedure should be anticipated. Given the strong association between Myhre syndrome and left-sided lesions/aortic hypoplasia, we would consider Myhre syndrome a “hypoplastic aortopathy” with similarities to Williams syndrome/elastin arteriopathy, Alagille syndrome and neurofibromatosis type 1 (Parker & Landstrom, 2021). Of note, the latter three are the most common genetic etiologies of mid-aortic syndrome which involves narrowing of the descending thoracic or abdominal aorta (Warejko et al., 2018) and has been used to describe Myhre syndrome patients (Brunet-Garcia et al., 2023), which we consider inappropriate. The aorta in Myhre syndrome has not been examined to determine if there is disruption of elastin fibers or increased proliferation of smooth muscle cells as in Williams syndrome (Urbán et al., 2002).
It is our impression that the aortic hypoplasia does not change very quickly and that it is appears to result from a lack of proportional aortic growth to match somatic growth. We perform CTA of the entire aorta in patients without anesthesia, generally over the ages of five to 7 years or whenever the child is behaviorally suitable to delineate the aortic morphology. This could be repeated every 5 years or sooner if there is unexplained hypertension. CTA is the preferred imaging modality at our institution because of brevity which allowed us to omit anesthesia in most (26 of 29, 90%) patients and adoption of low-radiation dose protocols for CTA. A Child Life Specialist who provided developmentally appropriate education and preparation for the scan helped to alleviate fear and anxiety and offer distraction and hands on support to create a less stressful environment. MRA can be performed without sedation after age 9–11 years in some children and may be an alternative to minimize radiation.
Reviews of pericardial disease in the adult may omit genetic syndromes which tend to affect pediatric patients (Dudzinski et al., 2012). Myhre syndrome may be the most common multiple anomaly syndrome (Table III in Lin et al., 2016) with pericardial disease in 15% of patients in this study, consistent with others (Garavelli et al., 2016; Yang et al., 2022). Pericardial disease included transudative and exudative pericardial effusions, acute and subacute/chronic pericarditis, and pericardial constriction (with tamponade physiology). At least one patient with “effusion” was noted to have CT evidence of a small nearly circumferential layer of organized material in the pericardial space which may reflect a more complex disease process. When suspected, echocardiography should be performed promptly since the clinical evaluation and chest radiograph are insufficient. Future research could evaluate serial measurements of the pericardium. There are currently no specific medical treatments for pericardial disease in Myhre syndrome, and standard therapies, especially NSAIDs have been utilized (Dudzinski et al., 2012) with variable results. Surgical intervention should be undertaken without delay when there is hemodynamic compromise, and may include pericardiocentesis, pericardial window or pericardial stripping. The co-occurrence of pleural effusions (which can also persist as a fibrinous collection), ascites and/or peritoneal adhesions supports the hypothesis that mechanism in Myhre syndrome involves serositis.
The genetic basis of RCM among all cardiomyopathies continues to be delineated (Ware et al., 2022), its occurrence in Myhre syndrome remains rare (less than 5%) (Lin et al., 2016; Lodato et al., 2022). Considering the rarity of RCM in the general population, two cases in the cohort of 47 patients is significant and needs to be kept under consideration during clinical evaluation. Echocardiography alone is insensitive to diagnose some patients with RCM as one patient had elevated filling pressures on catheterization without typical echocardiographic features of restriction such as bi-atrial enlargement. Additional testing such as cardiac catheterization should be considered in patients who have symptoms or signs rising suspicion of RCM.
As people with Myhre syndrome enter the fourth decade of life, greater attention should be given to the surveillance for coronary artery and peripheral vascular disease following evidence-based guidelines (Grundy et al., 2018). The detection of premature coronary artery disease in two women is notable, but its occurrence in Myhre syndrome is complicated by the chronic, complex co-morbidities including diabetes, overweight, and reduced activity. Lower radiation testing such as coronary calcium scoring should be considered for adults patient without additional risk factors (Greenland et al., 2018). Patients with additional comorbid conditions that increase the risk of atherosclerosis, such as diabetes may warrant consideration of a coronary CT.
Pulmonary hypertension has been associated with interstitial lung disease with RCM, unilateral stenosis of the left pulmonary artery, mitral valve disease (Shone complex), pulmonary sequestration, and chronic obstructive lung disease (McGowan et al., 2011; Starr et al., 2015; Yang et al., 2022). In our cohort, aside from one infant with pulmonary hypertension of prematurity, there was one patient with RCM and elevated pulmonary pressures, and another patient with RCM and pulmonary hypertension in the setting of postoperative TOF (Cappuccio et al., 2022). Evaluations of pulmonary hypertension in Myhre syndrome must include imaging and hemodynamic studies to determine if it is primary or secondary. Ultimately, post-mortem examinations are needed to determine underlying histology, anatomy, and correlation to clinical diagnoses (Table 3).
5.4 Ear, nose, throat, and upper airway features
Hearing loss is well-characterized and should be managed with a variety of modes of habilitation. Audiologic testing should include tympanometry and behavioral audiometry in children who can condition to these testing modalities. As children with Myhre syndrome may fall along the autistic spectrum, definitive audiometric testing may not be achievable in which cases auditory brainstem response testing under anesthesia may be required. In such cases it may be prudent to perform temporal bone imaging to detect inner ear anomalies under the same anesthetic. Interventions for children with hearing loss include classroom accommodations including preferential seating, use of hearing assistive devices such as Bluetooth® wireless technology or Hearing Assistive Technology, and consultation with an educational audiologist or teacher of the deaf to optimize the acoustic environment. Specific interventions will depend on the type and degree of hearing loss (conductive involvement is far more common than isolated sensorineural). For nonverbal patients or those with severely limited expressive speech, we endorse communication using many modalities including American sign language and electronic assistive technologies.
Small external ear canals may limit visualization of the tympanic membrane which is necessary to diagnose and treat middle ear disease. Excessive ear cerumen is often also atypical in quantity, color, and consistency and may be admixed with keratinaceous debris. When obstructive debris is present, regular removal by the ENT provider may be required to prevent infection, discomfort, and conductive hearing loss. Recurrent otitis media and other ear pathologies may prompt a referral for surgery including PE tube insertion. The ENT surgeon should counsel the parents about potential increased risks of PE tube insertion due to Myhre syndrome pathophysiology, which can include an increased risk of scarring and attendant risks of anesthesia. Likewise, surgery to remove enlarged tonsils and adenoids can be performed with prudent counseling.
Cleft palate and/or lip is rare and requires surgical treatment with awareness of potential scarring. For other palatal anomalies, including submucous cleft palate or VPI, nonsurgical management with speech therapy should be attempted, although it is not curative. The frequent occurrence of opacified mastoids, sinusitis and opacified sinuses in 30, 38, and 13% may reflect a noninfectious process consistent with Myhre syndrome.
5.5 Lower airway and pulmonary features
Myhre syndrome airway anomalies represent an expansion of the original name of this syndrome LAPS syndrome (Hopkin et al., 1998). Most parents and patients are aware of multilevel airway stenosis and fear its typical progression. However, it is rare and not directly related to a single intubation. We hypothesize that the severe multilevel airway stenosis is multifactorial in which a developmental anomaly is vulnerable to proliferative desquamation which leads to narrowing of tubular structures and spaces. This has not been proven by serial endoscopy beginning in infancy because of the concern, at least by our group, that procedures to image the airway may stimulate stenosis. From the head and neck region, progressing distally, we propose that copious debris leads to occlusion in the external ear canals, mastoids, nasolacrimal ducts, sinuses, choanae, posterior nasopharynx, larynx, trachea, and bronchi. However, despite our descriptive data and recognition that multilevel stenosis is typically lethal, we are unable to prognosticate who will be affected. Additional patients have been reported (patient 6 in Starr et al., 2022; Yang et al., 2022). The youngest reported patient (Jeon et al., 2021) with severe multilevel airway stenosis was identified at birth and followed to 21 months. He was reported to have lung fibrosis (not specified if biopsy was performed), and mild aortic stenosis associated with the SMAD4 Ile500Thr variant, and thus, the pathogenic variant may be a predictor of severity. Much of the current airway management is preventive, rather than therapeutic, and involves education for the families and providers, especially anesthesiologists (see Table 5 for guidelines).
| Specialty | Test or procedure | Initial | Follow-up | Comments |
|---|---|---|---|---|
| Genetics | ||||
| DNA-based genetics analysis for SMAD4 |
|
|
|
|
| Genetic counseling by geneticist and/or genetics counselor |
|
|
|
|
| Cardiovascular | ||||
| Blood pressure, upper and lower extremities at baseline. Measure right upper arm BP at each visit if tolerated. |
|
|
|
|
| Consultation by cardiologist trained in congenital heart disease |
|
|
|
|
| Two-dimensional echocardiography with Doppler |
|
|
|
|
| CT or MR angiography of aorta |
|
|
|
|
| Cardiac catheterization |
|
|
||
| Cardiac pathology |
|
|||
| Coronary CTA |
|
|
|
|
| Referral to transplantation service |
|
|
||
| ENT, airway | ||||
| Ear examination by ENT specialist |
|
|
|
|
| Audiogram |
|
|
||
| Auditory brainstem response test |
|
|
|
|
| CT with bone windows inner ear |
|
|
||
| Airway evaluation with nasal endoscopy |
|
|
|
|
| Pulmonary | ||||
| Airway evaluation with laryngoscopy and bronchoscopy |
|
|
|
|
| Oxygen saturation |
|
|
|
|
| Chest radiograph |
|
|
|
|
| Pulmonary function tests |
|
|
|
|
| CT angiography of pulmonary artery |
|
|
||
| 3 and 6-min- walk test |
|
|
||
| Sleep study |
|
|
|
|
| Gastroenterology | ||||
| Examination by pediatric gastroenterologist |
|
|
|
|
| Abdominal X-ray |
|
|
|
|
| Consultation with dietician |
|
|
|
|
| Abdominal ultrasound |
|
|
|
|
| Anorectal Manometry |
|
|
|
|
| Endocrinology | ||||
| Examination by pediatric endocrinologist |
|
|
||
| Nephrology, urology | ||||
| Genital exam |
|
|
||
| Renal and bladder ultrasonography |
|
|
|
|
| Renal ultrasonography with Doppler |
|
|
|
|
| Urodynamics |
|
|
|
|
| Functional testing for vesicoureteral reflux (VCUG or ceVUS) |
|
|
||
| Dermatology | ||||
| Skin evaluation by dermatologist |
|
|
|
|
| Neurosurgery, neurology | ||||
| MRI of spine |
|
|
|
|
MRI Brain MR Angiogram head and neck |
|
|
|
|
| CT spine |
|
|
|
|
| EEG |
|
|
|
|
| Ophthalmology | ||||
| Eye exam by ophthalmologist |
|
|
|
|
| Immunology | ||||
| Infectious history |
|
|
|
|
| Oral maxillofacial surgery (OMFS) | ||||
| Evaluation by dentist |
|
|
|
|
| Musculoskeletal | ||||
| Evaluation by orthopedic surgeon |
|
|
|
|
| Skeletal survey |
|
|
|
|
| Region specific radiographs |
|
|
|
|
| Physical therapy | ||||
| Evaluation by physical therapist |
|
|
|
|
| 3 or 6-min-walk test |
|
|
|
|
| Recommend therapies |
|
|
|
|
| Neurodevelopmental evaluation (by psychiatrist, psychologist, child neurologist, developmental behavioral pediatrician, or neurodevelopmental specialist) | ||||
| Early intervention and special education services (United States) |
|
|
Determines eligibility for state- and federally supported developmental services, including occupational therapy, physical therapy, speech and language therapy, applied behavioral analysis (ABA), learning, and adult transition supports. Services may be provided at home, in schools, or in the community. | |
| Neurodevelopmental or developmental behavioral pediatrics |
|
|
|
|
| Neuropsychology) |
|
|
|
|
| Psychiatry |
|
|
|
|
| Psychotherapy |
|
|
|
|
| Palliative or supportive care | ||||
| Consultation to assist the patient and family |
|
|
|
|
| Laboratory tests | ||||
| Electrolytes, BUN, creatinine, urinalysis, basic metabolic panel |
|
|
|
|
| IgG, IgA, IgM, IgE |
|
|
|
|
| Ferritin level |
|
|
|
|
| B-type natriuretic peptide (BNP) |
|
|||
| Liver function tests, albumin, protein |
|
|
||
| ESR, CRP |
|
|||
| HbA1C |
|
|||
- Abbreviations: AMBP; ambulatory blood pressure measurement; ASD, autism spectrum; CeVUS, contrast-enhanced voiding urosonography; CMA, chromosome microarray; C-reactive protein; ES, exome sequencing; ESR, erythrocyte sedimentation rate; GS, genomic sequencing; ID, intellectual disability; MRI, magnetic resonance imaging; PCP, primary care provider; RCM, restrictive cardiomyopathy; VCUG, voiding cystourethrogram.
Several types of pulmonary abnormalities in Myhre syndrome have been previously reported including restrictive and obstructive ventilatory deficits, which may be attributable to abnormalities in the chest wall, airways, or lung parenchyma. The most common imaging abnormality noted on CT scans was mosaic attenuation, which may reflect different expiratory time constants due to airway fibrosis (in areas of decreased attenuation) or subclinical interstitial fibrosis (in areas of increased attenuation). Yang et al. (2022) reported “nonspecific” pulmonary microcalcifications in three patients.
Pulmonary pathologic findings have included interstitial fibrotic lung disease (McGowan et al., 2011; Oldenburg et al., 2015; Starr et al., 2015) and one report of bronchiolitis obliterans (cryptogenic organizing pneumonia) suggesting an inflammatory pathology (McGowan et al., 2011). Histological descriptions are rare (table 1 in Starr et al., 2022). Lung biopsy detected diffuse interstitial fibrosis with copious collagen and smooth muscle hyperplasia of the airways suggesting interstitial pathology (Starr et al., 2015; Starr et al., 2022).
Improved delineation of the pulmonary features of Myhre syndrome will require increased pulmonary function testing in cooperative older children, exploration of alternative pulmonary function testing platforms (e.g., oscillometry, lung clearance index), CT angiography, lung biopsy, and postmortem examination (Starr et al., 2020). The recommendation to use incentive spirometry was not successful because of patients who were young, had ASD, or were not motivated. Physician diagnosis of “asthma” is notoriously non-specific and may not actually represent true asthma/reversible obstruction. A previous diagnosis of asthma should be reconsidered in the absence of spirometric evidence.
5.6 Gastroenterology
The frequency of abdominal pain (40%) can be difficult to interpret given the multiple potential contributors including constipation, foregut stenoses, peritoneal adhesions, and visceral hypersensitivity. Constipation in Myhre syndrome is common, often severe, and likely multifactorial. There may be components of slow transit as well as pelvic floor dysfunction due to functional outlet obstruction and low muscle tone. Dyssynergic defecation as reported in two males is currently unexplained (Tabbers et al., 2014). People with ASD often have a restricted diet which can further contribute to constipation. Treatment may require multiple laxatives including osmotic laxatives, stimulant laxatives, and secretagogues. Treatment with usual doses may be insufficient to prevent stool retention and patients sometimes need to be admitted for an aggressive cleanout. “Overflow” fecal incontinence can also occur in the setting of sub optimally treated constipation and often resolves with effective management of the constipation. Anorectal manometry can provide important information regarding the presence and potentially the etiology of dyssynergic defecation. Since the incidence of celiac disease In Myhre patients in this review was 6% compared to 1% in the general population, screening for celiac disease should be considered.
The development of peritoneal adhesions is consistent with the pericardial and pleural serositis, and a source of serious morbidity. These did not develop in all patients who had intra-abdominal surgery, and lysis was needed in only two patients.
Some of the feeding challenges may be due to primary behavioral or sensory-related food preferences but may also be secondary to gastrointestinal discomfort from symptoms of reflux, constipation, or other specific gastrointestinal diagnoses seen in this population. However, the co-occurrence of stenosis (one each with pyloric and duodenal involvement) and aortic hypoplasia may be evidence of Myhre syndrome pathophysiology involving ischemia or fibrosis. At present, there is no histological evidence of this from endoscopic biopsy or postmortem examination.
The occurrence of NASH (now called metabolic dysfunction-associated steatotic liver disease) (Eskridge et al., 2023), nonspecific “fatty liver,” and elevated LFTs alert us to the likelihood of liver involvement as patients age. Lifestyle (mainly exercise, diet, and overweight) and co-occurring diabetes are factors to be considered in pathogenesis.
5.7 Endocrinology and gynecology
Underascertainment of premature onset of puberty could be attributed to the young age (33% younger than age 12 years) in this series. There are also 15 children for whom follow-up after their examination at MGH is pending which could expand the natural history of this feature. At the original exam, puberty was not noted, nor reported by outside providers. To enhance management, consultation with a endocrinology specialist should be sought.
The use of growth hormone was not recommended at our center due to lack of evidence that there is a consistent increase in height velocity (Yang et al., 2022) despite anecdotal reports suggesting an association (Wu et al., 2021). Longitudinal studies will be needed to assess sexuality and fertility which was not studied yet in this cohort. In addition, the prevalence and etiology of glucose intolerance, diabetes, polycystic ovary syndrome, and aspects of metabolic syndrome, deserve further longitudinal evaluation.
5.8 Renal and urology
Angiotensin-Converting Enzyme Inhibitors/Angiotensin II Receptor Blocker/ARB are typically avoided in those with chronic kidney disease due to hypoperfusion/renovascular compromise. However, the choice of anti-hypertensive agent is often a collaborative choice between cardiology and nephrology, the former favoring it for its combined properties of afterload reduction and its theoretical effect on fibrosis. Therefore, for most patients with hypertension and intact renal function, we endorse the use of ARB agents, most commonly, losartan. While there are 22 patients with hypertension or elevated blood pressure, only 17 (77%) were treated with anti-hypertensive medication, and another five are being monitored to determine if medication should be started. Evidence is not yet available to support the use of losartan for fibrosing symptoms, although a small pilot study was supportive (Cappuccio et al., 2021).
We recommend that patients with Myhre syndrome undergo annual genital and exam and assessment of urinary tract function with periodic renal/bladder ultrasound. Incomplete bladder emptying can result from detrusor sphincter discoordination and can be complicated by constipation. Management of urinary incontinence is individualized. Patients with hydronephrosis and voiding dysfunction need more aggressive treatment and close follow-up.
5.9 Dermatology and connective tissue
The most common skin abnormality is “stiff skin” which is frequently self-reported or noted by a specialist. Skin thickening is likely progressive, and easily detected on the shoulder/upper arm region, and distal extremities. Another manifestation of skin thickening is fewer and less prominent facial rhytides (fine lines and creases). The dramatic skin thickening has been incorrectly diagnosed as scleroderma (Jensen et al., 2020). Both light and electron microscopy have confirmed densely packed dermal collagen fibers in the skin of affected adults with Myhre syndrome. Whereas transmission electron microscopy showed “an irregular elastin core with globular depositions, peripheral fragmentation and almost absent surrounding microfibrils” in the skin of affected children and adults (Meerschaut et al., 2019), light microscopy examination alone has not detected elastic fiber changes in the skin biopsies of affected individuals (Starr et al., 2022). Keratosis pilaris, a term that is used interchangeably with “hyperkeratosis” pilaris (Maghfour et al., 2022) may be reported by the parents as “bumpy skin” or “goose bumps.” This is a well-known feature in cardio-facio-cutaneous syndrome (Siegel et al., 2011).
Hair loss in Myhre syndrome has not yet been fully examined but appears to afflict affected individuals at a younger age compared to their family members. The distribution is consistent with androgenetic alopecia, but there is no histological confirmation as to why the terminal scalp hairs are miniaturizing sooner than expected. In addition to the features reported in Supplementary Table 7, there was a boy who had co-occurring familial lamellar ichthyosis. Several patients had abnormal scars which were neither hypertrophic nor “fine white lines”; they were widened, shinier, and more hypopigmented than the average well healed scar.
5.10 Brain and spinal cord
In light of this expanded description of intracranial arteriopathy (Yang et al., 2022), we recommend that MRI imaging with MR angiography of the brain be performed in all newly diagnosed patients. We hypothesize that the frequency of WMI may be more common than noticed in this study. The full phenotype is incomplete, and there may be patients with steno-occlusive arteriopathy in adulthood. The WMI itself warrants referral to neuropsychological testing, especially cognitive functions such as processing speed which can be affected by multifocal WMI (Guo & Shi, 2022). When possible, central visual and auditory processing testing should be performed to determine the need for educational resources and devices.
The suspicion for tethered cord was typically raised in the setting of a certain lumbosacral skin anomaly (deep gluteal creases), disproportionate reduction in nervous system function of the lower trunk and lower extremities, severe constipation, scoliosis, and/or leg pain. When these symptoms and signs are present, a spine MRI is indicated. The long-term impact of detethering surgery is not yet available to determine if progression was prevented.
5.11 Ophthalmology
Prior data on the ophthalmological manifestations of patients with Myhre syndrome are limited. In one case series of two patients, retinal findings including photopic dysfunction consistent with a maculopathy and retinitis pigmentosa were reported (Al Ageeli et al., 2012). Neither of our oldest patients had retinopathy. Another case of a toddler with a p.Ile500Val mutation had corectopia of the pupil and TOF (Alagia et al., 2018) suggesting neural crest cell dysregulation.
Our report significantly expands the ocular characterization with the most common findings being visually significant refractive error, anomalous optic nerve appearance, strabismus, and lacrimal system abnormalities. With respect to hyperopic refractive error and crowding at the optic nerve head or “pseudopapilledema,” further work is needed to determine whether these findings may be the result of a shorter axial length of the eye leading to hyperopia which may co-occur with a short stature syndrome (Bonnel et al., 2000; Moshirfar et al., 2022; Nowaczyk et al., 2022).
Because many of these ocular features may adversely impact visual development and function, we advocate for Myhre patients to have complete ophthalmological evaluations to monitor for and treat these findings.
5.12 Immunology
Recurrent sinopulmonary infections are frequently encountered in Myhre syndrome. While this traditionally is associated with the aforementioned airway abnormalities prior cohorts have described individuals with humoral immunodeficiency that responds to immunoglobulin replacement therapy. A recent study (Yang et al., 2022) described hypogammaglobulinemia in 4/12 patients with Myhre syndrome, two of which had low IgG and required replacement immunoglobulin therapy until middle childhood; the remaining two patients manifested with IgA and IgG subclass deficiency not requiring treatment. There are other reports of IgG and IgA deficiency (Hartono et al., 2023), IgA deficiency (Garavelli et al., 2016), and unspecified humoral immunodeficiency (Michot et al., 2014), along with two additional individuals requiring replacement immunoglobulin therapy (Starr et al., 2015). More comprehensive immune phenotypes have been investigated with some suggestion of low baseline antibody titers, and decreased memory T and B cells compared to age matched controls (Bukhari et al., 2020; Hartono et al., 2023). The prevalence of atopic disease (allergic rhinitis, atopic dermatitis, asthma, food allergy) had not been previously reported. In our cohort we describe a high percentage of evaluated patients with hypogammaglobulinemia, although few received replacement antibody therapy. We recommend consideration of measuring immunoglobulins (IgG, IgA, IgM, IgE) in those with recurrent sinopulmonary infections with frequency or severity out of proportion of what is typically observed in Myhre syndrome and/or once school age is reached. Measurement of specific antibody titers to pneumococcus, and tetanus with additional vaccination, prophylactic antibiotics and replacement antibody therapy can be considered in conjunction with a clinical immunology consultation.
5.13 Craniofacial and dental
The striking prominent jaw that was depicted in the initial patients described by Myhre et al. (1981) is not ubiquitous but can appear in some children and progress (Figure 5). We agree that prognathism may not be due to absolute mandibular overgrowth, but from disharmonious growth of the mandible or relative to maxillary hypoplasia (Yang et al., 2022).
5.14 Musculoskeletal features, including physical therapy
In an exhaustive review, Costantini et al. (2023) note that the skeletal findings in Myhre syndrome can be classified as an acromelic dysplasia with metaphyseal dysplasia (Unger et al., 2023). Common features include short stature, skeletal connective tissue abnormalities, and cardiorespiratory complications. This large group of disorders are the result of pathogenic genes which are members of the TGF-β superfamily or regulate TGF-β bioavailability. Cardiospondylocarpofacial syndrome (stiff spine, tarsal, and elbow joints) overlaps because of contractures and hearing loss. Despite the common pathway, Myhre syndrome differs greatly from syndromes with tall stature, joint laxity, and aortic dilation (table 1 in Costantini et al., 2023).
Stiff joints may progress to severe arthritis and contractures which impair the quality of life. The impact of physical therapy intervention has not been studied in the Myhre population; however, current management emphasizes the importance of physical therapy to promote mobility and function as well as reduce the risk of orthopedic complications. With a program of physical therapy in young patients, we hope to reduce progression, although compliance may be difficult due to lack of engagement and behavior. Parents endorsed keeping their children as active as possible with dance, sports, theater, and general play. Recommendations were made regarding PT services, equipment and bracing needs, and home programs.
Fractures may be at least 20 times more common (28%) in Myhre syndrome since the annual occurrence rate for children (0–19 years) is approximately 10 per 1000 (1%) (Naranje et al., 2016). Correlation to vitamin D deficiency was not possible since we do not consistently obtain vitamin D levels. Both patients 1 and 2 had vitamin D deficiency with multiple fractures occurring only in patient 1. Dual-energy X-ray absorptiometry scans are not currently recommended as surveillance and could be studied for low bone density in the future. In general, childhood activities should not be curtailed.
5.15 Development, neuropsychology, psychiatry, and neurology
SMAD4 impacts the brain widely. The range of developmental, behavioral, and neurologic abnormalities in Myhre syndrome is large. Improved delineation of the baseline prevalence and natural history will require more frequent early childhood assessment, serial neuropsychological testing, psychiatric and neurologic examinations, and EEG testing. Global developmental delay is nearly ubiquitous, incorporating motor (fine and gross) and speech and language delays. Approximately one-third of patients met diagnostic criteria for an ID. Social communication difficulties are also common with the majority of patients meeting diagnostic criteria for ASD; however, unlike other genetic syndromes which have a distinctive behavioral profile (Palumbo & McDougle, 2018; Thom, 2023), Myhre syndrome patients display a more variable phenotype.
ADHD, characterized by challenges with attentional regulation and often executive functions, was also present in approximately half of patients. Although the number of patients was too small to classify by variant and age (or if unspecified), overall, 14 (56%) had combined inattentive and hyperactive ADHD. However, the numbers of patients taking medication to treat ADHD symptoms was considerably smaller, suggesting that there may be undertreatment. Treating ADHD (assuming current treatments are successful), could have a positive effect on daily functioning. Similarly, co-morbid mental health concerns may exacerbate cognitive and social difficulties, and anxiety was common (approximately 40% of patients).
Identifying and addressing the neuropsychiatric challenges that these patients may face is critical for improving quality of life and functioning. Reassuringly, we have not observed dementia in the three adults in our sample. Though not observed in our cohort, mental illness including schizophrenia (Inoue et al., 2021), affective disorder (Artemios et al., 2019), “affective psychotic” disorder (Bhushan et al., 2023) and “hallucinations and aggressiveness” (Yang et al., 2022) have been noted. When suspected, these should be evaluated by a psychiatrist with experience in working with patients with neurodevelopmental disorders.
5.16 Infrequent features
As noted in the clinical summary section, endometrial cancer occurred in one woman in our cohort with a SMAD4 Arg496Cy pathogenic variant (patient 2, Lin et al., 2020). Although it was reported originally that all three women with endometrial cancer had the Arg496Cys variant, the Corrigendum (Lin et al., 2024) noted that one patient (Table 1, patient 3 in Lin et al., 2020) had a pathogenic variant in NM_005359.6(SMAD4):c.1499 T > C (p.Ile500Thr) (Table 3, patient 2 in Oldenburg et al., 2015). It is unclear whether the association of endometrial cancer correlates with untreated PCOS.
This same patient 2 also developed diabetes requiring insulin at age 15 years which could also reflect a pattern of diabetes associated with insulin resistance, PCOS, and obesity. Two additional patients have type 2 diabetes that require both high dose insulin as well as a GLP-1 receptor agonist.
5.17 Comparison with other syndromes
Although people with Myhre syndrome, especially toddlers, can be suspected of having another syndrome, it is our impression that there is greater awareness of the distinctive facial appearance, habitus, and cardiovascular anomalies. As noted (Lin et al., 2016), Myhre syndrome can be confused with William syndrome, Alagille syndrome and the Ras-MAPK pathway syndromes which are also associated with coarctation of the aorta, and/or reduced aortic caliber, and valve dysplasia (Lin et al., 2011; Pober, 2010; Spinner, 1999). We propose the term, “hypoplastic aortopathy” for these disorders (and others) which includes variable involvement of the aorta and branches, cervical, cerebral, and retinal arteries. This distinguishes them from the familiar phenotypes of thoracic aortic aneurysm and dissection in which aortic enlargement and tortuosity are the hallmarks.
The overlap of pericardial disease in Myhre syndrome and at least three other disorders was noted previously (table III, Lin et al., 2016). Myhre syndrome should not be mistaken for Cantu syndrome (Grange et al., 2006; van Bon et al., 2012) or the Camptodactyly-Arthropathy-Coxa vara-Pericarditis syndrome (Faivre et al., 2000; Taşar et al., 2014). MULIBREY dwarfism is an autosomal recessive syndrome-, caused by mutations in TRIM37, associated with both pericardial constriction and myocardial restrictive disease (Eerola et al., 2007; Lipsanen-Nyman et al., 2003). But distinguished by volume restriction of the bell-shaped thorax with thin ribs, failure of sexual maturation, liver disease, and frequent tumors (Karlberg et al., 2009; Sivunen et al., 2020). Aside from these multiple anomaly syndromes, RCM can be seen with several inborn errors of metabolism (Sen-Chowdhry et al., 2010).
5.18 Pharmacotherapy
As noted in the individual specialty sections above, multiple drugs were used without identifying any which were clearly superior or detrimental. The exception is the recommendation to use an angiotensin II receptor blocker agent based on involvement of the TGF-ß signaling pathway. This is largely due to the small number of patients. One area to be explored would be medication metabolism.
5.19 Genetic insights
The SMAD4 gene encodes a critical component of the TGF/BMP/SMAD signaling pathway, playing a pivotal role in various cellular processes, including cell growth, differentiation, migration, adhesion, organization, and apoptosis. Dysregulation of SMAD4 function is associated with a spectrum of human diseases, such as malformations, vascular diseases, skeletal and muscular dysfunction, tissue fibrosis, inflammation, and cancer predisposition syndromes (figure 1 in Massagué & Sheppard, 2023). Intriguingly, Myhre syndrome is uniquely linked to two missense mutations at Ile500 and Arg496 in SMAD4. The variant location and restricted spectrum of Myhre syndrome-causing mutations suggest that these alterations have distinct consequences on SMAD4 functions.
Current understanding posits that these mutations lead to an elevated TGF-β superfamily signaling activity, termed a “gain-of-function” mode of action. This hypothesis is supported by evidence linking excessive TGF-β signaling to fibrotic diseases (Hu et al., 2018; Walton et al., 2017). Additionally, human disorders caused by loss of function mutations in the canonical TGF-β signaling cascade, such as Marfan syndrome or Loeys–Dietz syndrome (LDS), also have cardiac, pulmonary, and skeletal abnormalities, but the phenotype is opposite that of Myhre syndrome (Gheewalla et al., 2022). Diseases resulting from reduced TGF-β superfamily signaling exhibit features distinct from Myhre syndrome. For instance, loss-of-function mutations (including large deletions and nonsense variants) in SMAD4 or BMPR1A result in juvenile polyposis/hereditary hemorrhagic telangiectasia syndrome, which markedly elevates susceptibility to tumorigenesis and aneurysm. Similarly, LDS caused by loss-of-function mutations in TGFBR1, TGFBR2, SMAD3, TGFB2, or TGFB3 genes, also presents a multisystem connective disorder despite reduced protein function.
The gain-of-function hypothesis is supported by observations that a SMAD4 mutation stabilizes the protein, increasing SMAD4 levels in human skin fibroblasts (Piccolo et al., 2014). However, conflicting studies propose impaired TGF-β-mediated transcriptional activity induced by Myhre SMAD4 mutation with reports of reduced ubiquitination and downstream target gene expression in fibroblasts from Myhre patients (Alankarage et al., 2022; Le Goff, Mahaut, Abhyankar, et al., 2011; Le Goff, Mahaut, Wang, et al., 2011).
The Ile500 residue lies in the MH2 domain at the C terminus of the SMAD4 protein. MH2 domain is indispensable for SMAD oligomerization, which is required for TGF-β/BMP signal transduction. However, the MH2 domain mediates interaction with a wide variety of proteins, providing specificity and selectivity to SMAD4 function. According to the crystal structure of SMAD4 (Chacko et al., 2004; Qin et al., 1999; Shi et al., 1997), Ile500 is close to the protein surface and is surrounded by and interacts with the hydrocarbon part of the side chains of residues Arg496, Arg497, Arg502, Glu526, and His528. These surrounding residues are highly conserved in SMAD4 orthologs and paralogs and constitute a binding site for anions (Qin et al., 1999; Shi et al., 1997). The solvent-exposed location of this region and its highly charged character make it a likely candidate for protein–protein interactions. Based on this information, it is reasonable to speculate that the substitution of Ile500 by other amino acids in SMAD4 would impact intermolecular interactions between SMAD4 and other signaling partners. However, whether or not this leads to paradoxical elevation in TGFβ-BMP-SMAD signaling remains to be addressed. Cross-talk between SMAD4 mutations and TGF-ß/IFNγ signaling can lead to cellular senescence (Kandhaya-Pillai et al., 2021). The molecular mechanisms underlying Myhre syndrome, particularly the consequences of SMAD4 pathogenic variants, remain incompletely understood and require further study, particularly if we are to identify potential treatments for this condition.
6 STUDY STRENGTHS AND WEAKNESSES
The strength of this work is the extensive, systematic cataloguing of the pleiotropic clinical features with an emphasis on a practical evaluation of affected patients. However, despite the extensive amount of data, and longitudinal data for some patients, we are unable at present time to discern which patterns of disease progression are likely to progress in most patients with Myhre syndrome. The exceptions would be joint stiffness, for which we endorse baseline physical therapy and orthopedic evaluations, appropriate exercises as tolerated, and avoidance of sedentary lifestyle. This cross-sectional retrospective analysis characterizes the natural history for certain patients with Myhre syndrome. There is a bias of ascertainment if diagnostic testing was performed for symptoms already present, in contrast to underascertainment if testing could not be completed due to young age or ASD.
This is the largest (total 47, new 43) prospective study of carefully phenotyped patients with Myhre syndrome by an inter-specialty team at an academic institution, although the actual number of patients is small. There was no person with the pathogenic variant in SMAD4 Ile500Met. Robust care coordination, consistent examinations and access to state-of-the-art diagnostic imaging allowed enhanced delineation of characteristic phenotypes and natural history assessment. Outreach from the “MGH Myhre syndrome medical home” to local providers promotes care and stimulates feedback to continue longitudinal analysis. Because these were fee-for-service evaluations usually covered by insurance (rarely, as self-pay), ascertainment bias is acknowledged. The COVID-19 pandemic delayed in-person evaluations, but telemedicine was a pragmatic short-term substitute, for which in-person follow-up encounters are steadily being completed.
Despite differences in study design and patient enrollment, the frequency and age of onset of selected findings was generally similar to Yang et al. (2022) (Table 6). Information about features which predict greater morbidity and mortality may provide an answer to the question of “what to expect” but lead to great distress about prognosis. We strongly endorse the role of palliative and supportive care (Vadeboncoeur & McHardy, 2018) which helps a patient and family “live the best life” in addition to anticipating terminal events. When adolescents and young adults are involved in the discussion, autonomy of future decision making can be promoted.
| Feature | Yang et al. (2022)a | Present study | Comparison with Yang et al. (2022) |
|---|---|---|---|
| Number patients, total (%) | 12 (100%) | 47 (100%) | Larger cohort |
| Age (years): mean | 22 | 12.9 | Younger cohort |
| New patients | 6/12 (50%) | 43/47 (91%)b | Greater number of new patients |
| Sex (female) | 9/12 (75%) | 31/47 (66%) | Similar female excess |
| SMAD4 variants reported in both studies | |||
| Ile500Val (c.1498A > G) | 9/12 (75%) | 23/47 (49%) | Less common variant |
| Ile500Thr (c.1499 T > C) | 2/12 (17%) | 5/47 (12%) | Similar |
| Arg496Cys (c.1486C > T) | 1/12 (8%) | 18/47 (38%) | More common variant |
| Growth | |||
| IUGR | 12/12 (100%) | 25/47 (53%) | Less frequent |
| Overweight | 4/12 (33%) | 6/47 (13%) | Onset younger: Middle childhood |
| Pseudomuscular hypertrophy | 9/12 (75%) | 27/47 (57%) | Middle childhood |
| Short stature | Not stated | 34/47 (72%) | Middle childhood |
| Facial features | |||
| Prognathism, maxillary hypoplasia, narrow palpebral fissure, thin upper lip, short philtrum | 5–11/12 (42–92%) | 46/47 (98%) | Recognition at a younger age, mild: Early childhood |
| Sensory | |||
| Refractive errors | 9/12 (75%) | Early childhood | |
| Hearing impairment | 7/12 (58%) | 18/47 38% | Less frequent Similar onset early childhood |
| Musculoskeletal | |||
| Joint limitations | 8/9 (89%) | 44/47 (94%) | Detection at younger age: Toddler |
| Brachydactyly | 11/11 (100%) | 30/47 (64%) | Toddler |
| Two to three toe syndactyly | 2/9 (22%) | 31/47 (66%) | Toddler |
| Clinodactyly | 4/8 (50%) | 33/47 (70%) | Toddler |
| Camptodactyly | 2/8 (25%0 | 8/47 (17%) | Toddler |
| Cardiovascular | |||
| Pericarditis | 2/9 (22%) | 7/47 (15%) | Middle childhood |
| CHD | Septal defect 3/11 (27%) PDA 3/9 (33%) COA 2/9 (22%) AoVS 3/10 (30%) |
See Supplemental Table 1 | Infancy |
| Restrictive cardiomyopathy | 2/47 (4%) | Adolescence | |
| Vascular hypoplasia | “Stenosis” 3/7 (43%) | Mild 18/47 (38%) Mod-severe 10/47 (21%) Total 28/47 (60%) |
Detection at younger age: Toddler |
| Systemic hypertension | 3/11 (27%) | 18/47 (38%) | New: Early childhood? |
| Neurodevelopmental | |||
| Intellectual deficit | 9/12 (75%) | 15/47 (32%) | Toddler |
| Developmental delay | 9/12 (75%) | 47/47 (100%) | Toddler |
| Autistic-like behavior | 1/9 (11%) | 42/47 (89%) | More frequent, younger age: Early childhood |
| ADHD | Not stated | 25/47 (53%) | Middle childhood |
| Anxiety | Not stated | 19/47 (40%) | Middle childhood |
| Airway, lungs | |||
| Laryngeal or tracheal stenosis | 2/12 (17%) | Multilevel 1/47 (2%) | |
| Gastrointestinal | |||
| Constipation | Not stated | 32/47 (68%) | Toddler |
| Gastrointestinal stenoses | 2/12 (16%) | 3/47 (6%) | Toddler |
| Miscellaneous | |||
| Precocious puberty (male, female) | 8/11 (73%) | 5/21 (24%) males 8/26 (31%) females |
Middle childhood |
| Thickened skin | 8/12 (75%) | 38/47 (81%) | Earlier: Young childhood |
| Cancer | 0 | 1/26 females | Adults |
| Infertility | 1 | 2/26 females | Adult |
| Diabetes | 1 | 2/47 (4%) | Adult |
- Abbreviations: ADHD, attention-deficit/hyperactivity disorder; AoVS, aortic valve stenosis; CHD, congenital heart defect; COA, coarctation; FTT, failure to thrive; IUGR, intrauterine growth retardation; OSA, obstructive sleep apnea diagnosed by sleep study; PF, Palpebral fissures.
- a Ages of onset (adapted from Yang et al., 2022): infancy (<12 months); toddler (12 months—2 years); early childhood (2–5 years); middle childhood (6–11 years); adolescence (12–18 years); and adult (>18 years).
- b Four patients previously reported in Michot et al. (2014), Lin et al. (2016), Lin et al. (2020), Cappuccio et al. (2022), and Starr et al. (2022).
7 UPDATED RECOMMENDATIONS
Using the additional information from this personal experience, Table 5 expands on the recommendations in GeneReviews (Lin et al., 2022). Although these are not currently evidenced-based guidelines and reflect our “expert” opinion, they are pragmatic suggestions. Medical articles are increasingly read by patients and families who should discuss this information with their primary care provider and a Myhre syndrome specialist, typically a medical geneticist. The MSF serves as a global clearing house for information, including a network of knowledgeable providers.
We urge providers to refrain from diagnosing a patient as having Myhre syndrome or “Myhre syndrome-like” if SMAD4 variant confirmation is negative or has not been performed (Bachmann-Gagescu et al., 2011), especially in a patient with atypical features. Appropriate genetic testing should be pursued.
8 FUTURE DIRECTIONS
Extended natural history studies with larger cohort size and racial diversity are essential to calculate survival. Further research should be directed to understanding the general connective tissue disorder which leads to fibrosis, stenosis, scarring and proliferation at many sites. The paucity of pathologic examination in general, including tissue sampling during life (e.g., endoscopic biopsies) and postmortem examination (autopsy) means that histological delineation of tissues is lacking which would be useful to interpret clinical symptoms (Starr et al., 2022). Prospective neuropsychological and behavioral testing is necessary to define cognitive abilities and the prevalence of ASD. Deep phenotyping such as this study will hopefully complement animal model research and other tissue studies. Further basic science investigations are essential to unravel the molecular intricacies of the SMAD4 pathogenic variants, potentially identifying targets for therapeutic interventions. Targeted gene therapy will be influenced by the priorities of the patients and parent community, and the abnormalities which are amenable to intervention.
9 CONCLUSIONS
This article presents a comprehensive overview of the clinical features, including physical findings and multisystem investigations as well as detailed genetic analysis of patients with this ultrarare condition, studied at an academic medical center. A syndrome specific inter-specialty clinic facilitates the prospective acquisition of clinical data, which is more specific, and at the same time, more generalizable than single case reports and small series. The purpose is to promote longevity and better treatment. Myhre syndrome patients with mild facial features, normal stature, intact social skills, and structurally normal hearts may not be diagnosed in early childhood. However, in patients with autism, the striking cardiovascular abnormalities or airway anomalies should be tested for Myhre syndrome without hesitation. This research should be used to support compensation for genetic testing. The propensity for progressive involvement of nearly every lumen and potential space in the body which leads to high morbidity and mortality mandates development of translational drug research.
MGH MYHRE SYNDROME STUDY GROUP
The authors are grateful to many colleagues who referred patients or to MGH colleagues who evaluated them as members of the Myhre Syndrome Study Group.
Luisa Paredes Acosta.
Jennifer A. Bassetti.
Sarah Bowdin.
Joy A. Bress.
Joseph A. Camarda.
Joanne S. Chiu.
C. Eduardo Corrales.
Gregory Costain.
Mary Beth P. Dinulos.
Rajiv Devanagondi.
Emily S. Doherty.
John Dykes.
Ann-Christine Duhaime.
Robert F. English.
Elizabeth Fieg.
Nora D. B. Friedman.
Carl P. Garabedian.
Samantha Glowacki.
Barbara R. Gottlieb.
Mary Hope Griffin.
Frances J. Hayes.
Stephanie R. Hicks.
Alicia M. Hinze.
Brigette A. Jason.
Joel Krier.
Kristen Lindgren.
Michael Lyons.
Adnan Majid.
Hannah C. Mannem.
Marie McDonald.
Vinod Misra.
Amy Morgan.
Barbara J. Nath.
Michele Ploutz.
Eloise J. Prijoles.
Margaret B. Pulsifer.
Alicia M. Quesnel.
Farrah Rajabi.
Mersedeh Rohanizadegan.
Ana Maria Rosales.
Holly Rothermel.
Edith Schussler.
Elizabeth A. Sellars.
Joseph Shieh.
Stephanie Sherrill.
Heidi Taska-Tench.
Matthew Thompson.
George E. Tiller.
Stephanie E. Vallee.
David Viskochil.
Stephanie Ware.
Rachel C. Whooten.
Samuel Yang.
Elaine H. Zackai.
Dala Zakaria.
AUTHOR CONTRIBUTION STATEMENT
Conceptualization: A.E.L., E.R.S., M.E.L.; methodology and data curation: A.E.L., E.R.S., E.C., M.E.L., L.A.S.; funding acquisition: A.E.L., M.E.L; statistical analysis: E.R.S.; writing-original draft: A.E.L., E.R.S. All listed authors meet authorship criteria, certifying active participation, and individual contributions. Collectively, they take public responsibility for content, manuscript submission, and approval of the final draft; all but three (E.C., K.D.D., and H.M.) were directly involved in patient care.
ACKNOWLEDGMENTS
The authors express their sincere gratitude to the many families and patients with Myhre syndrome who inspired this research, and who have been their teachers and partners in clinical care and research. The authors thank the MSF Board of Directors and extend their gratitude to many MGH support staff especially medical assistants, patient service coordinators, and administrative staff. This research would not be possible without the support of many generous donors to the MGH Myhre Syndrome fund. Dr. Christina Vadeboncoeur and Mindy McHardy provided supplemental information for Table 3 about their patient (Vadeboncoeur & McHardy, 2018). Dr. Robert Smigiel provided brief follow-up about the patient who had a SMAD4 Ile500Leu variant (Slezak et al., 2021). Dr. Lindsay reported research support from Angea Biotherapeutics, LLC.
FUNDING INFORMATION
The Clinical Research Coordinator position for the Myhre Syndrome Clinic is supported in part by the Myhre Syndrome Foundation and donors to the MGH Myhre Syndrome Clinic Sundry Fund.