Exploring the evolving roles of clinical geneticists and genetic counselors in the era of genomic medicine
Abstract
The increased utilization of clinical genomic sequencing in the past decade has ushered in the era of genomic medicine, requiring genetics providers to acquire new skills and adapt their practices. The change in workplace responsibilities of clinical/medical geneticists (CMGs) and genetic counselors (GCs) in North America, due to the evolution of genetic testing, has not been studied. We surveyed CMGs (n = 80) and GCs (n = 127) with experience in general/pediatric genetics to describe their current practice of clinical tasks and the change in regularity of performing these tasks over the past 5–10 years. Currently, complementarity of responsibilities between CMGs and GCs clearly exists but providers who have been in the field for longer have noted role changes. Trends indicate that fewer experienced CMGs perform physical exams and select genetic tests than before and fewer experienced GCs complete requisitions and write result letters. The frequency of CMGs and GCs who investigate genetic test results, however, has increased. This study provides insight into the changing landscape of clinical genetics practice. Our findings suggest that the roles and responsibilities of CMGs and GCs have shifted in the past decade.
1 INTRODUCTION
Genetics healthcare has been gradually shifting into an era of precision genomic medicine over the past few decades. The evolution of next generation sequencing (NGS) and the subsequent development of exome and genome sequencing (ES/GS), in particular, have been integral to this shift. Since its first use for clinical diagnosis in 2010, the application of ES/GS has expanded to include prediction of disease presentation, prognostication, and guidance of treatment decisions (Bertier et al., 2016; Schuler et al., 2013). The advances in sequencing capabilities and its utility in medicine have also led to increased use of ES/GS in clinical care among different non-genetic specialties such as neurology, cardiology, and nephrology (Amendola et al., 2021; Barozzi et al., 2019; Fogel et al., 2016; Groopman et al., 2019).
The utilization of ES/GS in clinical medicine has also brought about various practice changes among genetics providers including a more genotype-first approach to the diagnostic process (Dwarte et al., 2019). This strategy arguably decreases the reliance on a physical exam, traditionally performed by clinical/medical geneticists (CMGs), during the pre-test diagnostic stage (Schaaf, 2021). The increased use of ES/GS has also necessitated CMGs and genetic counselors (GCs) to become more familiar with some aspects of variant interpretation science and the processes for reanalysis of previously uncertain results. The responsibility of initiating variant reanalysis and reinterpretation has primarily fallen on genetics providers since there is no current consensus or practice guidelines about who the responsibility should belong to (Berger et al., 2022). This lack of consensus in the field leaves these tasks occurring on an ad hoc basis, and adds them to clinical providers' already long list of other responsibilities (Carrieri et al., 2017; Dheensa et al., 2017).
The shift to genomic medicine in the last decade has required both CMGs and GCs to learn new skillsets and take on new tasks in the clinical setting. Understanding how the clinical responsibilities of genetic professionals have changed since ES/GS was introduced is important in order to provide insight into how best to support current providers in their ongoing professional skill development and prepare the incoming workforce to meet the demands of this evolving field.
Little is known about the changes in CMG and GC workplace responsibilities in North America in the advent of the genomic medicine era. Previous studies have investigated the roles, responsibilities, and benefits of different genetics professionals in the healthcare setting (Jenkins et al., 2021; NSGC, 2022; Paneque et al., 2017; Pestoff et al., 2015; Schaaf, 2021; Tromans & Barwell, 2022), but no formal exploration of the interrelated roles of CMGs and GCs has been conducted since the implementation of genomic testing in the last decade. This cross-sectional study aimed to fill this knowledge gap by surveying CMGs and GCs in general or pediatric genetics clinics about their current roles and skillsets and how they have evolved over the past decade.
2 MATERIALS AND METHODS
2.1 Participants and recruitment
CMGs and GCs in North America who had experience working in a patient-facing role in pediatrics or general genetics clinics were recruited (Supplementary Figure 1). CMGs were eligible for the study if they had an M.D. or D.O. degree and completed an Accreditation Council for Graduate Medical Education accredited residency in Medical Genetics and Genomics. To maximize the number of CMG participants, we conducted an online search of general and pediatric genetics clinics to identify CMGs and invited them to participate in the study using publicly available email addresses. Up to two email reminders were sent to CMGs to complete the study survey. GCs were invited to participate through an e-blast sent to the National Society of Genetic Counselors' (NSGC) listserv in July 2022 with a reminder email sent in August 2022. GCs were eligible for the study if they received a master's degree in genetic counseling from a program accredited by the Accreditation Council for Genetic Counseling (ACGC) and obtained certification or were eligible to obtain certification from the American Board of Genetic Counseling (ABGC). GCs who were not eligible for the study were automatically excluded from participation through screening questions. Invitations included a short introduction to the study and a link to the study survey (described below). Everyone who completed the survey had the option of entering a raffle to win a $100 gift card.
2.2 Survey
An online survey was administered to eligible participants via Qualtrics, a web-based data collection platform. Three GCs, one CMG, and a genetic counseling graduate student developed the survey. It consisted of questions related to demographics, clinical work experience, and skills/tasks and responsibilities associated with general and pediatric genetics appointments. Sixteen clinical tasks derived from the American Board of Medical Genetics and Genomics' (ABMGG) guidelines for residency training in medical genetics and the Accreditation Council for Genetic Counseling's (ACGC) core competencies were chosen to investigate. For each task, participants were asked (1) if they currently perform the task and (2) how the frequency of performing the task changed from earlier in their career. The survey was estimated to take between 5 and 10 min to complete and the questions were presented in a combination of multiple choice, ordinal scale, and open-ended formats. Survey responses were collected from June until November 2022 and were anonymous.
2.3 Data analysis
Demographic data were analyzed using frequencies and percentages to describe the survey respondents. We used two proportion Z tests to compare the current proportion of performing certain clinical tasks with profession (CMGs or GCs) and the change in task performance with different career lengths for each cohort. For the clinical tasks shown to have a significant association between career length and task performance, observed patterns or trends in the data were described. The two-tailed alpha value was set at 0.05.
3 RESULTS
3.1 Participants
A total of 260 individuals started the survey, of whom 19 were not clinicians with patient-facing time in a general/pediatric genetics clinic and were therefore screened out automatically for ineligibility, and 34 were eligible but did not complete the survey and were excluded from analysis. Responses from the remaining 207 participants were included in the final analysis (80 CMGs and 127 GCs). In the CMG cohort, the majority of participants were female (57.5%), worked in an academic center (91.2%), and were employed full time (87.5%). Almost equal proportions of geneticist participants reported 2–5 CMGs (43.7%) and 2–5 GCs (42.5%) working in their clinic and had mostly worked in the field for over 20 years (37.5%). Enrolled participants were from 30 different states in the United States of America. In the GC cohort, the majority of participants were female (92.1%), worked in an academic center (73.2%), and were employed full time (96.1%). Most GCs worked in a clinic with 2–5 CMGs (43.3%) and 2–5 GCs (50.4%). GCs who had responded had mostly worked in the field for less than 5 years (56.7%). Participants were from 37 American states, 2 participants were from the District of Columbia, and 4 participants were from Canada. Demographic data of participants are given in Table 1.
| Geneticists (n = 80) | Genetic counselors (n = 127) | |
|---|---|---|
| % (n) | % (n) | |
| Age | ||
| 20–29 years | 0 (0) | 38.58 (49) |
| 30–39 years | 12.5 (10) | 39.37 (50) |
| 40–49 years | 20.0 (16) | 7.09 (9) |
| 50–59 years | 18.75 (15) | 4.72 (6) |
| >60 years | 22.5 (18) | 0.79 (1) |
| Unknown | 26.25 (21) | 9.45 (12) |
| Sex | ||
| Female | 57.5 (46) | 92.13 (117) |
| Male | 40.0 (32) | 6.30 (8) |
| Unknown | 2.5 (2) | 1.57 (2) |
| Clinic specialty | ||
| Pediatrics only | 6.25 (5) | 23.62 (30) |
| General only | 45 (36) | 7.87 (10) |
| Both pediatric and general | 47.5 (38) | 68.5 (87) |
| Unknown | 1.25 (1) | 0 (0) |
| Length of career | ||
| Less than 5 years | 6.25 (5) | 56.69 (72) |
| 5–9 years | 18.75 (15) | 30.71 (39) |
| 10–14 years | 20.0 (16) | 4.72 (6) |
| 15–19 years | 17.5 (14) | 1.57 (2) |
| 20 or more years | 37.5 (30) | 6.29 (8) |
| Employment status | ||
| Full time | 87.5 (70) | 96.06 (122) |
| Part time | 11.25 (9) | 3.15 (4) |
| NA | 1.25 (1) | 0.79 (1) |
| Practice setting | ||
| Academic center | 91.25 (73) | 73.23 (93) |
| Regional/community hospital | 6.25 (5) | 18.11 (23) |
| Private practice | 2.5 (2) | 1.57 (2) |
| Other | 0 (0) | 7.09 (9) |
| Genetic counselors in clinic | ||
| None | 3.75 (3) | 0 (0) |
| 1 | 1.25 (1) | 11.02 (14) |
| 2–5 | 42.5 (34) | 50.39 (64) |
| 6–10 | 32.5 (26) | 26.77 (34) |
| 10–15 | 8.75 (7) | 9.45 (12) |
| 16+ | 11.25 (9) | 2.36 (3) |
| Clinical geneticists in clinic | ||
| None | 0 (0) | 6.30 (8) |
| 1 | 6.25 (5) | 20.47 (26) |
| 2–5 | 43.75 (35) | 43.31 (55) |
| 6–10 | 33.75 (27) | 23.62 (30) |
| 10–15 | 8.75 (7) | 5.51 (7) |
| 16+ | 7.5 (6) | 0.79 (1) |
| Patients per week | ||
| Less than 4 | 6.25 (5) | 13.39 (17) |
| 4–10 | 33.75 (27) | 43.31 (55) |
| 11–15 | 23.75 (19) | 25.98 (33) |
| 16–20 | 15 (12) | 13.39 (17) |
| 21–25 | 15 (12) | 1.57 (2) |
| 26–30 | 5 (4) | 0.79 (1) |
| Over 30 | 1.25 (1) | 1.57 (2) |
| % time patient facing | ||
| Less than 20% | 13.75 (11) | 7.09 (9) |
| 20% | 16.25 (13) | 19.69 (25) |
| 40% | 20 (16) | 29.13 (37) |
| 60% | 28.75 (23) | 22.83 (29) |
| 80% | 16.25 (13) | 9.45 (12) |
| 100% | 5 (4) | 11.81 (15) |
| Non-outpatient related tasks | ||
| Teaching | 96.3 (77) | 74.8 (95) |
| Inpatient care | 86.3 (69) | 40.9 (52) |
| Administrative roles | 70 (56) | 61.4 (78) |
| Research | 83.8 (67) | 33.9 (43) |
3.2 Current prevalence of clinical tasks performed
Of the CMG cohort, every respondent (100%) currently performs the tasks of providing medical management recommendations, explaining a differential diagnosis, and selecting an appropriate genetic test. Tasks that the least number of CMGs currently perform include completing genetic test requisitions (58.75%) and writing result letters (62.5%). The majority of CMGs also reported performing other, non-outpatient related responsibilities including teaching (96.3%), inpatient care (86.3%), administrative roles (70%), and research (83.75%) (Table 1). Of the GC cohort, the tasks that the highest number of participants currently perform are investigating genetic test results (99.2%), obtaining consent for genetic testing (99.2%), and collecting family history (99.2%). Fewer GCs reported providing medical management recommendations (72.4%) and providing medical referrals (61.4%). GCs also reported performing responsibilities related to teaching (74.8%), inpatient care (40.9%), administrative roles (61.4%), and research (33%) (Table 1). The frequency of CMGs and GCs currently performing each of the 16 clinical tasks was assessed and is displayed in Figure 1.
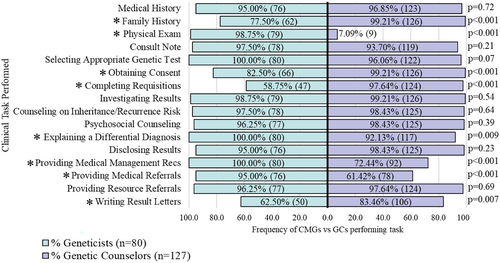
When comparing current prevalence of task performance between both cohorts, CMGs are significantly more likely to perform a physical exam (p < 0.001), explain a differential diagnosis (p = 0.009), provide medical management recommendations (p < 0.001), and provide medical referrals (p < 0.001) than GCs. On the other hand, GCs are significantly more likely to gather family history (p < 0.001), obtain consent for genetic testing (p < 0.001), complete order requisitions (p < 0.001), and write genetic test result letters (p = 0.007) than geneticists.
3.3 Association of practice settings with current task performance
The likelihood of CMGs currently performing any of the listed clinical tasks was not associated with their patient volume, the amount of patient-facing time they had in their job, or the length of their career. However, CMGs who reported fewer GCs working in their clinic were more likely to complete test requisitions (p = 0.03) and write result letters (p = 0.049) (Supplementary Tables 1–4).
In the GC cohort, no significant associations were identified between GCs' current performance of any of the clinical tasks and their patient volume, their years of work experience, or the number of GCs and CMGs in their clinic. However, the GCs with more patient-facing time in their job were more likely to select genetic tests (p = 0.043) and write result letters (p = 0.040) (Supplementary Tables 5–8).
3.4 Change in clinical task performance
To assess change in performance frequency of different clinical tasks, we divided the CMG cohort into experienced CMGs who have worked in the field for ≥10 years (eCMGs; n = 60) and newer CMGs who have worked for <10 years (nCMGs; n = 20). eCMGs noted changes in how often they perform several clinical tasks over the past 10 years when compared to changes noted by nCMGs from the start of their careers. eCMGs were significantly more likely to have changed how frequently they perform physical exams (p = 0.040), select appropriate genetic tests (p = 0.040), obtain consent (p < 0.001), complete order requisitions (p = 0.020), investigate results (p = 0.002), psychosocially counsel (p = 0.022), and disclose genetic test results (p = 0.005). Trends indicated decreased regularity of performance over time by sizeable proportions of eCMGs for obtaining consent for genetic testing (56.7%), completing test requisitions (50%), disclosing genetic test results (45%), psychosocial counseling (23.3%), performing physical exams (23.3%), and selecting appropriate genetic tests (16.7%). The only task that saw a trending increase in performance regularity among eCMGs was investigating genetic test results (28.3%). Table 2 displays the comparison of associations between career length of CMGs and change in frequency of performing different clinical tasks between eCMGs and nCMGs.
| Task | Number of geneticists whose task performance frequency changed | Number of genetic counselors whose task performance frequency changed | ||||
|---|---|---|---|---|---|---|
| Career length (<10 years) (n = 20) | Career length (≥10 years) (n = 60) | P value | Career length (<5 years) (n = 72) | Career length (≥5 years) (n = 55) | P value | |
| Medical history | 8 | 16 | 0.260 | 17 | 18 | 0.255 |
| Family history | 6 | 31 | 0.092 | 6 | 12 | 0.031a |
| Physical exam | 1 | 16 | 0.040a | 29 | 24 | 0.704 |
| Consult note | 4 | 18 | 0.386 | 21 | 21 | 0.285 |
| Selecting appropriate genetic test | 1 | 16 | 0.040a | 30 | 28 | 0.300 |
| Obtaining consent | 7 | 47 | <0.001a | 14 | 15 | 0.298 |
| Completing requisitions | 9 | 44 | 0.020a | 18 | 28 | 0.003a |
| Investigating results | 2 | 30 | 0.002a | 24 | 29 | 0.028a |
| Counseling on inheritance/recurrence risk | 5 | 29 | 0.068 | 8 | 12 | 0.101 |
| Psychosocial counseling | 3 | 26 | 0.022a | 15 | 13 | 0.706 |
| Explaining a differential diagnosis | 3 | 12 | 0.620 | 23 | 16 | 0.730 |
| Disclosing results | 7 | 42 | 0.005a | 18 | 19 | 0.241 |
| Providing medical management recs | 2 | 16 | 0.122 | 25 | 22 | 0.542 |
| Providing medical referrals | 3 | 19 | 0.148 | 28 | 23 | 0.739 |
| Providing resource referrals | 5 | 30 | 0.051 | 23 | 9 | 0.045a |
| Writing result letters | 9 | 39 | 0.114 | 25 | 30 | 0.025a |
- a Implies two-tailed significance value of less than 0.05.
Among the GCs, we divided the cohort into experienced GCs who have worked in the field for ≥5 years (eGCs; n = 60) and newer GCs who have worked for <5 years (nGCs; n = 20) to assess the change in how often the clinical tasks are performed. eGCs were significantly more likely than nGCs to have changed how frequently they gather family history (p = 0.031), complete order requisitions (p = 0.003), investigate results (p = 0.028), provide resource referrals (p = 0.045), and write result letters (p = 0.025). Of these five tasks, observed trends suggest high proportions of eGCs noted decreased performance of writing result letters (30.9%) and completing requisitions (29.1%), while a small number of eGCs decreased how frequently they obtain family history (12.7%). Just as with the CMGs, a large proportion of eGCs noted increased performance of investigating genetic test results (49.1%) and a smaller number noted an increase in providing resource referrals (14%). Table 2 compares the associations between the career length of GCs and the change in frequency of performing different clinical tasks between eGCs and nGCs.
Overall, both eCMG and eGC subcohorts reported that their frequency of performance had not changed for a majority of the clinical tasks. Table 3 summarizes the number of eCMGs and eGCs who noted changed in frequency of performing different tasks.
| Geneticists career length ≥10 years (n = 60) | Genetic counselors career length ≥5 years (n = 55) | Geneticists career length ≥10 years (n = 60) | Genetic counselors career length ≥5 years (n = 55) | ||
|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | ||
| 1. Medical history | 9. Counseling on inheritance/recurrence risk | ||||
| Performance increased | 15.0 (9) | 10.9 (6) | Performance increased | 23.3 (14) | 18.2 (10) |
| Performance stayed the same | 73.3 (44) | 67.3 (37) | Performance stayed the same | 51.7 (31) | 78.2 (43) |
| Performance decreased | 11.7 (7) | 21.8 (12) | Performance decreased | 25.0 (15) | 3.6 (2) |
| 2. Family history | 10. Psychosocial counseling | ||||
| Performance increased | 18.6 (11) | 7.3 (4) | Performance increased | 20.0 (12) | 12.7 (7) |
| Performance stayed the same | 49.2 (29) | 78.2 (43) | Performance stayed the same | 56.7 (34) | 76.4 (42) |
| Performance decreased | 33.3 (20) | 14.5 (8) | Performance decreased | 23.3 (14) | 10.9 (6) |
| 3. Physical exam | 11. Explaining a differential diagnosis | ||||
| Performance increased | 3.3 (2) | 5.5 (3) | Performance increased | 11.7 (7) | 16.4 (9) |
| Performance stayed the same | 73.3 (44) | 56.4 (31) | Performance stayed the same | 80.0 (48) | 70.9 (39) |
| Performance decreased | 23.3 (14) | 38.2 (21) | Performance decreased | 8.3 (5) | 12.7 (7) |
| 4. Consult note | 12. Disclosing results | ||||
| Performance increased | 13.3 (8) | 23.6 (13) | Performance increased | 25.0 (15) | 30.9 (17) |
| Performance stayed the same | 70.0 (42) | 61.8 (34) | Performance stayed the same | 30.0 (18) | 65.5 (36) |
| Performance decreased | 16.7 (10) | 14.5 (8) | Performance decreased | 45.0 (27) | 3.6 (2) |
| 5. Selecting appropriate genetic test | 13. Providing medical management recommendations | ||||
| Performance increased | 10.0 (6) | 41.8 (23) | Performance increased | 21.7 (13) | 21.8 (12) |
| Performance stayed the same | 73.3 (44) | 49.1 (27) | Performance stayed the same | 73.3 (44) | 60.0 (33) |
| Performance decreased | 16.7 (10) | 9.1 (5) | Performance decreased | 5.0 (3) | 18.2 (10) |
| 6. Obtaining consent | 14. Providing medical referrals | ||||
| Performance increased | 21.7 (13) | 16.4 (9) | Performance increased | 21.7 (13) | 20.0 (11) |
| Performance stayed the same | 21.7 (13) | 72.7 (40) | Performance stayed the same | 68.3 (41) | 58.2 (32) |
| Performance decreased | 56.7 (34) | 10.9 (6) | Performance decreased | 10.0 (6) | 21.8 (12) |
| 7. Completing requisitions | 15. Providing resource referrals | ||||
| Performance increased | 23.3 (14) | 21.8 (12) | Performance increased | 30.0 (18) | 12.7 (7) |
| Performance stayed the same | 26.7 (16) | 49.1 (27) | Performance stayed the same | 50.0 (30) | 83.6 (46) |
| Performance decreased | 50.0 (30) | 29.1 (16) | Performance decreased | 20.0 (12) | 3.6 (2) |
| 8. Investigating results | 16. Writing result letters | ||||
| Performance increased | 28.3 (17) | 49.1 (27) | Performance increased | 18.3 (11) | 16.4 (9) |
| Performance stayed the same | 50.0 (30) | 47.3 (26) | Performance stayed the same | 35.0 (21) | 45.5 (25) |
| Performance decreased | 21.7 (13) | 3.6 (2) | Performance decreased | 46.7 (28) | 38.2 (21) |
- Abbreviations: CMGs, clinical/medical geneticists; GCs, genetic counselors.
4 DISCUSSION
Despite the significant advancements in genomic medicine over the past decade, our understanding of the evolving job responsibilities of CMGs and GCs in North America remains limited. In addressing this gap, we surveyed CMGs and GCs and established central themes involving their current roles and how they have changed over the last decade.
4.1 Complementarity in roles
In general, the current landscape confirms that there is complementarity in the roles of CMGs and GCs; while this may not be unexpected, it is important to formally note as the interrelated roles of CMGs and GCs have not been assessed in the current era. Of the 16 clinical tasks assessed for current prevalence of task performance, CMGs were more likely to perform tasks such as explaining a differential diagnosis, providing medical management recommendations, and performing physical exams. In contrast, GCs were more likely to gather family history, obtain consent for genetic testing, complete order requisitions, and write genetic test result letters. These findings reflect both unique and shared skill sets and training of each profession, as well as support the existing literature describing the clinical roles of GCs and CMGs (Jenkins et al., 2021; Schaaf, 2021; Tromans & Barwell, 2022). Furthermore, these data echo the studies of European genetic professionals showing the distribution of clinical tasks, especially the responsibility of administrative work completed by GCs (Paneque et al., 2017; Pestoff et al., 2015). CMGs with more GCs in their workplace were less likely to perform administrative tasks in a session, but most CMGs still complete many of the administrative tasks measured. This responsibility of administrative work is further endorsed by previous studies, wherein the time spent performing indirect patient care by general/pediatric genetics providers consumed most of their time (Attard et al., 2019; Sukenik-Halevy et al., 2016).
CMGs and GCs are also filling more roles outside of the outpatient clinic. Nearly all CMGs and 75% of GCs reported teaching as an additional role, which may reflect the current emphasis on recruiting and training more genetics professionals, as well as educating non-genetics providers on genomic medicine (Crellin et al., 2019; Maiese et al., 2019).
4.2 Change in roles over time
While most CMGs and GCs who have been in the field over the past decade reported that there were no changes to many of the clinical tasks they perform, several CMGs and GCs did report changes in their roles that have come about over time. Many of our experienced GC respondents noted a decrease over time in how often they perform a number of administrative tasks, especially writing result letters and completing test requisitions. Result summary letters have long been considered a standard of practice that sets apart the genetics field from many other medical specialties (Forrest et al., 2010). Multiple studies have shown that patients find summary letters to be beneficial in lowering anxiety and retaining information after receiving a diagnosis (Brown et al., 2021; Cassini et al., 2011). However, these letters tend to be long, detailed, and time-consuming to write; these challenges have likely been magnified by the increased utility of ES/GS and larger gene panels, which can discover more uncertain variants than smaller panels and single gene tests (Beaumont & Wright, 2022; van Lint et al., 2019). It is possible that the need for these letters to be written has decreased with the evolution of more patient-friendly result reports and summaries being generated directly by labs. In the past decade, genetic testing labs have introduced various efforts to ensure patients have a good understanding of their results which have included the creation and assessment of patient education materials and the employment of lab GCs to help explain results (Dwyer et al., 2021; Swanson et al., 2014). However, the financial challenges faced by commercial genetic testing companies and subsequent layoffs in recent years may see these administrative support services dwindle, thus putting the responsibility of these tasks back onto the clinician (Stoll et al., 2022; Wolff & Wolff, 2018).
The decrease in frequency of more administrative tasks such as completing requisitions in both cohorts may be indicative of an increase in employment of genetic counseling assistants (GCAs) who are taking these tasks on, or that the execution of these tasks are being automated. The impact of GCAs on clinic efficiency has been described (Hnatiuk et al., 2019; Krutish et al., 2022; Pirzadeh-Miller et al., 2017). GCAs have been reported to take on tasks such as data entry, shipping samples, research, and ordering supplies. With the additional workforce, clinics are able to significantly increase patient volume by giving GCs and CMGs more time for direct patient care (Cohen et al., 2023; Hallquist et al., 2020). Furthermore, the automation of clinical tasks, such as consenting and facilitating cascade testing with the use of chatbots has shown to free up more time for genetic professionals and increase patient volume (Schmidlen et al., 2019; Schmidlen et al., 2022). Clinical genetic testing laboratories have begun to address this administrative load as well through online portals that facilitate order requisition and consenting, alleviating genetic professionals from the task burden and allowing for more time in direct patient care (Snir et al., 2021). Artificial intelligence (AI), in addition, has made major impacts on medical genetics through automated systems such as phenotype-to-genotype mapping to identify patients with a likely genetic condition and the use of deep-learning algorithms to assist in genome annotation and variant classification (Dias & Torkamani, 2019; Solomon & Chung, 2023). As AI utilization in healthcare continues to increase, genetics professionals may see even greater decreases in their performance of certain tasks, thus making more time available for direct patient care.
Many CMGs saw a decrease in obtaining consent and disclosing results. It is possible that these tasks are being taken on more by GCs. However, the recent combination of the increased utilization of genomic testing in medicine subspecialties and shortage of genetics providers in the workforce has led to an increasing number of non-genetics providers ordering testing (Bajguz et al., 2022). This has caused more post-genetic test result referrals to the genetics clinic wherein patients are only seen by CMGs/GCs after the return of positive or uncertain results (Truong et al., 2021). This trend could be contributing to the decrease in frequency of CMGs disclosing results and obtaining consent for genetic testing.
The one task that saw a marked increase in performance frequency among sizeable groups in both cohorts was the investigation of results. This skill refers to the task of researching a genetic test result to obtain more detailed information than what is provided in a test report. It is possible that this shift is a direct result of increased next generation sequencing tests being ordered which are likely to generate a higher number of results containing variants of uncertain significance (VUS). VUS's can be reclassified, but there is currently a lack of systematic and universal methods for this interpretation (Horton & Lucassen, 2019). Recommended interpretation guidelines have been established by many professional organizations including the American College of Medical Genetics and Genomics and the Association of Molecular Pathology (Richards et al., 2015). These recommendations are helpful to guide variant interpretation but are not comprehensive and still leave much of the final determination to the judgment of the clinical laboratory, therefore creating discrepancy in how different clinical genetics laboratories interpret the same variants (Amendola et al., 2016; Horton & Lucassen, 2019). These discrepancies may prompt CMGs and GCs to do their own variant investigation, which can utilize a lot of their time (Berrios et al., 2021).
4.3 Limitations
Our data relied on self-reported information from participants and was limited to those practicing in general or pediatric genetics clinics, which may impact its generalizability to other genetic specialties. The recruitment methods differed across the cohorts, introducing potential sampling bias, specifically in the CMG cohort, as only CMGs with publicly available emails were invited to complete the survey. Moreover, the response rate to the survey was low, and a significant proportion of GCs were excluded from the temporal analysis due to their inexperience, potentially skewing the results. There were not enough GCs with 10 years of experience to have a direct comparison between the CMG and GC cohorts, which prompted us to limit the eGC cohort to those with at least 5 years of experience. 2015–2019 saw the creation of 15 GC programs across North America, increasing the number of programs by nearly 50% (NSGC, 2023). This would lead to a significant influx of new GCs with less than 10 years of experience at the time of this study, which is reflected in our data. This stratification may have skewed results, as the cohorts were asked about their task performance at different time points. The study design introduced the possibility of recall bias, as participants were asked to reflect on their clinical task performance over the past 5 or 10 years.
4.4 Future recommendations
Understanding the changes in the workplace responsibilities of clinical genetic professionals informs the field and may have important implications for designing both training and continuing education programs, such as creating continuing education modules to equip providers with the skills to address the observed increase in result investigation. The existence of these significant findings also underscores the importance of ongoing research to monitor the changes in the practice of genomic medicine over time as the field continues to evolve. The current landscape and observed changes in clinical tasks and responsibilities for genetic professionals highlight the need for ongoing education and training to ensure that providers are prepared to meet the evolving demands of their roles.
Future studies could investigate the confidence levels of the respondents in performing each task, which may give even greater recommendations for training programs. Furthermore, a change in recruitment strategy to gather a larger cohort would allow for greater generalizability of the findings. It may be beneficial to include GCAs in future studies as well to measure their impact. Finally, a future research direction could be a qualitative study with CMGs and GCs to gather more in-depth information about how their roles have changed over the past decade and to explore the factors that may be driving those changes.
4.5 Conclusion
This study provides insight into the changing landscape of clinical genetics practice in the era of genomic medicine. Our findings suggest that the roles and responsibilities of CMGs and GCs have shifted in the past decade. These changes have important implications for the training and education of future genetics professionals and highlight the need for ongoing evaluation of clinical practice to optimize patient care.
AUTHOR CONTRIBUTIONS
Conceptualization: Andrew Freiman, Aisha Rekab, Priyanka Ahimaz; Data curation: Andrew Freiman, Priyanka Ahimaz; Formal analysis: Andrew Freiman, Yuhuan Lin; Funding acquisition: Andrew Freiman, Priyanka Ahimaz; Investigation: Andrew Freiman, Aisha Rekab, Priyanka Ahimaz; Methodology: Andrew Freiman, Amanda L. Bergner, Elaine M. Pereira, Priyanka Ahimaz; Project administration: Priyanka Ahimaz; Supervision: Priyanka Ahimaz; Visualization: Andrew Freiman; Writing-original draft: Andrew Freiman; Writing: Review and editing: Aisha Rekab, Amanda L. Bergner, Elaine M. Pereira, Yuhuan Lin, Priyanka Ahimaz.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.