Caregiver-reported clinical characteristics and the burden associated with Kabuki syndrome
Abstract
Kabuki syndrome is a genetic disorder that can affect multiple body systems and manifest as congenital abnormalities and both developmental and socio-emotional delays. The condition is largely unknown by most primary care physicians and has no available treatment other than symptomatic management. This research sought to obtain caregiver-reported data about the experience of living with and caring for someone with Kabuki syndrome to fill a gap in the available literature. Fifty-seven caregivers participated in an online survey and reported that Kabuki syndrome affected their children in a wide variety of ways, including a high frequency of visits to various healthcare professionals. Caregivers reported their child experienced problems with hearing, eating, eyes, mouth, immune system, anxiety, depression, autism, teeth, joints, seizures, kidneys, and heart. Caregivers also described the challenges of caring for someone with Kabuki syndrome, including an impact on emotional well-being and the ability to work outside the home. This unique research characterizes the caregiver experience of living with and caring for someone with Kabuki syndrome, both through observed manifestations of Kabuki syndrome in their own children and their experience managing their treatment. Additional research is needed to investigate the patient experience of living with Kabuki syndrome.
1 INTRODUCTION
Kabuki syndrome, first described by Drs. Niikawa and Kuroki in 1981, is a rare disorder characterized by congenital abnormalities that affect the development and function of multiple bodily systems, often manifesting as impaired mental and physical growth and craniofacial, visceral, and skeletal abnormalities, among a wide variety of other abnormalities (Niikawa et al., 1988). The prevalence is estimated at one in every 32,000 live births and recent literature describes 201 missense variants (Adam & Hudgins, 2005; Bögershausen et al., 2016; Faundes, Malone, Newman, & Banka, 2019; Kasdon & Fox, 2012; Matsumoto & Niikawa, 2003).
An international group of experts created new consensus diagnostic criteria for Kabuki syndrome that includes a variant in the KMT2D or KDM6A genes and dysmorphic features (i.e., two or more of the following: “arched and broad eyebrows with the lateral third displaying notching or sparseness, short columella with depressed nasal tip, large, prominent or cupped ears, persistent finger pads”; Adam et al., 2018). Other manifestations used to assist diagnosis include: skeletal abnormalities, dermatoglyphic abnormalities, developmental delay, and short stature (Cheon & Ko, 2015; Lepri et al., 2018; Liu et al., 2015). This condition is largely unknown by most primary care physicians and may be misdiagnosed, as the phenotype evolves over time and socio-emotional delays may be mistaken for other conditions (Cheon & Ko, 2015; Kasdon & Fox, 2012).
In addition to the cardinal features, a review of Kabuki syndrome descriptions in the literature found that patients may also experience system-wide issues, including but not limited to: feeding, neurological (e.g., seizures), cardiovascular, kidney, endocrine, ophthalmologic, hearing, dental, gastrointestinal, urinary tract, musculoskeletal, and immunologic issues (Adam, Dugan, Hudgins, & Hannibal, 2010; Cheon & Ko, 2015; Dentici et al., 2015; Lepri et al., 2018) Individuals with Kabuki syndrome may also experience psychosocial issues, but are widely known to exhibit a gregarious behavior (Adam et al., 2010; Caciolo et al., 2018).
Currently, there are no effective treatments for Kabuki syndrome; the only treatment option is management of the manifestations of the condition (Lu, Mo, Ling, & Ji, 2016). Case studies describe a wide range of medical issues, developmental disorders, and socio-emotional factors that lead to variation in the management of patients; care can be complex and may include medical intervention to minimize susceptibility to infection, dental issues, or cardiac problems and/or psychotherapeutic intervention for both patients and their families (Crane, Alpert, Cyrkiel, & Jauregui, 2013; Kasdon & Fox, 2012). Treatment may also include assistance with feeding (e.g., feeding tubes), antiepileptic medications for seizures, educational assistance, and various psychological interventions (Adam et al., 2010; Kasdon & Fox, 2012; Lu et al., 2016). Kabuki syndrome is not typically associated with severe medical complications, and with proper management of congenital anomalies in childhood, prognosis for survival into adulthood is good (Adam & Hudgins, 2005; Kasdon & Fox, 2012).
Nonetheless, many patients need the assistance of a caregiver into adulthood. Caregivers often face many stressful situations while taking care of their relative or patient. Caregivers may deal with burden from physical, psychological, emotional, social, and/or financial stressors (Toledano-Toledano & Domínguez-Guedea, 2019). In general, caregivers of patients who have been diagnosed with a chronic illness often face interrupted sleep, family conflict, personal mental health struggles, and the possibility of lower quality of life (Javalkar et al., 2017).
While there are individual studies and clinical descriptions on the presentation of Kabuki syndrome, there is little information on the frequency of certain features in larger cohorts (Adam et al., 2018). Further, nowhere in the literature is the burden on the caregivers of patients with Kabuki syndrome described. Given the wide range of unique issues experienced by these patients, it is hypothesized to pose a heavy burden on the parents or primary caregiver. The purpose of this research was to obtain caregiver-reported data about the experience of living with someone with Kabuki syndrome and to better characterize the patient experience from the perspective of the caregiver via an online survey.
2 METHODS
2.1 Recruitment and eligibility criteria
- Verbal consent to be screened over the phone;
- ≥18 years old;
- Located in the United States (US) or Canada;
- Able to identify how they learned about the survey;
- Able to identify when their son or daughter was diagnosed with Kabuki syndrome;
- Able to confirm their son or daughter had at least one of the five cardinal manifestations of Kabuki syndrome): unique facial features, skeletal deformities, fingerprint abnormalities, mild or moderate intellectual disability, and/or growth deficiencies;
- Confirmation that they were able to read and complete an online survey in US English; and
- Confirmation that they were willing and able to complete an online survey that took at least 45 min to complete.
2.2 Data collection
The caregiver survey consisted of 156 multiple choice and open response questions on various topics using branched logic; caregivers answered only a portion of these questions due to skip patterns associated with their responses. It included questions such as how they found out about the study as well as their child's diagnosis, healthcare provider information, the clinical characteristics of Kabuki syndrome, and the burden of living with and caring for someone with Kabuki syndrome. For questions including medical jargon (e.g., conductive hearing loss), a brief explanation (e.g., hearing loss due to problems with the ear canal ear drum, or middle ear) was also provided to ensure understandability.
2.3 Data analysis
All data were analyzed descriptively (e.g., frequency, mean, SD, range, etc.) for all survey respondents. All open response items from the survey were analyzed using ATLAS.ti. version 7.5.18 or higher (Atlas.ti GmbH, Berlin), a software program designed specifically for qualitative data analysis.
3 RESULTS
3.1 Demographic and health characteristics
Most caregivers (n = 54, 94.7%) were female and the average age of caregivers was 40 years old (range: 21–64). Caregivers reported they had both male (n = 29, 50.9%) and female (n = 28, 49.1%) children, with their child's age ranging from one to 32 years ( = 9). Most caregivers (n = 54, 94.7%) reported their child was diagnosed with Kabuki syndrome via genetic testing and that they were diagnosed by a geneticist (n = 57, 100.0%). When asked to report which of the five characteristic manifestations of Kabuki syndrome their child exhibited, all caregivers (n = 57, 100.0%) endorsed unique facial features; the next most common characteristic reported was abnormal fingerprints (n = 53, 74.6%). See Table 1 for demographic and health information reported by caregivers.
= 9). Most caregivers (n = 54, 94.7%) reported their child was diagnosed with Kabuki syndrome via genetic testing and that they were diagnosed by a geneticist (n = 57, 100.0%). When asked to report which of the five characteristic manifestations of Kabuki syndrome their child exhibited, all caregivers (n = 57, 100.0%) endorsed unique facial features; the next most common characteristic reported was abnormal fingerprints (n = 53, 74.6%). See Table 1 for demographic and health information reported by caregivers.
| Characteristics | Total (n = 57)n (%) |
|---|---|
| Location | |
| United States | 52 (91.2%) |
| Canada | 5 (8.8%) |
| Caregiver gender | |
| Female | 54 (94.7%) |
| Male | 3 (5.3%) |
| Child gender | |
| Male | 29 (50.9%) |
| Female | 28 (49.1%) |
| Caregiver age | |
| Range | 21–64 |
| Average (SD) | 40 (8.8) |
| Child age | |
| Range | <1 year to 32 years |
| Average (SD) | 9 (7.1) |
| Genetic testing | |
| Received genetic testing | 54 (94.7%) |
| Did not receive genetic testing | 3 (5.3%) |
| Diagnosing clinician | |
| Geneticist | 57 (100.0%) |
| Characteristics | |
| Unique facial features | 57 (100.0%) |
| Abnormal fingerprints | 53 (74.6%) |
| Mild or moderate intellectual disability | 49 (69.0%) |
| Growth deficiencies | 47 (66.2%) |
| Issues with body skeleton | 32 (45.1%) |
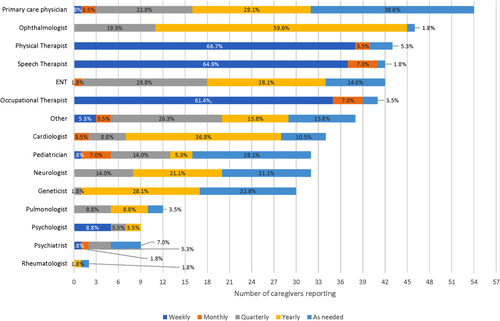
Caregivers were also asked to report on the frequency of visits to healthcare providers. A wide variety of healthcare providers was used in addition to primary care physicians and were seen either weekly, monthly, quarterly, yearly, or as needed. The most commonly seen healthcare providers were seen weekly: physical therapist (n = 38, 66.7%), speech therapist (n = 37, 64.9%), and occupational therapist (n = 35, 61.4%). See Figure 1 for a full summary of frequency of visits to treatment providers.
3.2 Caregiver-reported clinical characteristics
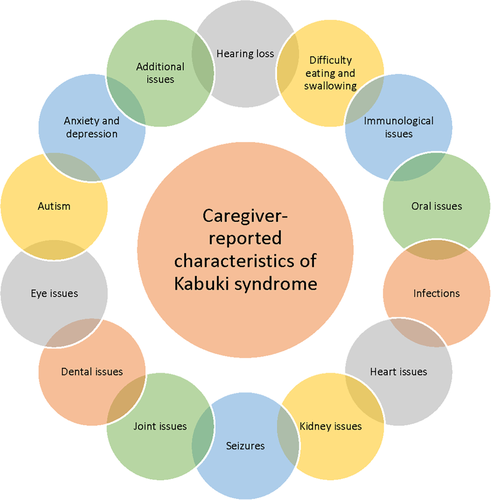
Caregivers were asked to report whether or not their child had a wide variety of characteristics and/or medical issues associated with Kabuki syndrome. See Figure 2 for an overview of caregiver-reported clinical characteristics.
3.2.1 Hearing loss
Slightly less than half of caregivers (n = 25, 43.9%) reported their child experienced hearing loss. Caregivers reported that hearing loss began, on average, at 3 years old (range: <1 year old to 13 years old). Of caregivers whose child had hearing loss, slightly less than half reported that their child wore a hearing aid (n = 12, 48.0%). The most common type of hearing loss reported by caregivers was conductive hearing loss (i.e., hearing loss due to problems with the ear canal, ear drum, or middle ear; n = 12, 42.9%), followed by unknown type of hearing loss (n = 9, 32.1%), mixed hearing loss (i.e., problems/damage in the outer or middle ear and the inner ear [cochlea] or auditory nerve; n = 5, 17.9%), and sensorineural hearing loss (i.e., hearing loss due to problems of the inner ear, also known as nerve-related hearing loss; n = 5, 17.9%).
3.2.2 Difficulty eating and swallowing
Most caregivers reported that their child was not able to swallow pills (n = 26, 59.1%) and over half reported that their child had difficulty eating foods orally (n = 25, 61.0%). The majority of caregivers reported that their child had used a feeding tube (n = 36, 60.0%), with the average age of placement at <1 year old (range: <1 year to 1 year old). Of the caregivers who reported that their child had used a feeding tube, the majority reported that it had been removed at the time of the study (n = 20, 55.6%).
3.2.3 Oral issues
Oran issues reported by caregivers included: submucosal cleft palate (i.e., a split in the roof of the mouth, either in the hard or soft portion of the palate) (n = 19, 76.0%), bifid uvula (i.e., a cleft or fork in the uvula, the part of skin that hangs down from the back part of the roof of the mouth) (n = 11, 44.0%), and velopharyngeal insufficiency (i.e., there is not enough tissue in the roof of the mouth for the palate to contact the back of the throat during speech) (n = 8, 32.0%). Further, 10 (40.0%) caregivers reported their child had surgery to repair oral issues and five (38.5%) said they were considering facial surgery.
3.2.4 Immunological issues
Twelve (21.1%) caregivers reported their child has an immune disorder or low immunoglobulins. Immune disorders reported via a write-in response on the survey were: low Immunoglobulin A (n = 4, 33.3%), low immunoglobulins (n = 3, 25.0%), low Immunoglobulin G (n = 2, 16.7%), combined variable immunodeficiency (n = 1, 8.3%), does not make influenza A or B antibodies (n = 1, 8.3%), Evans syndrome (n = 1, 8.3%), Hypogammaglobulinemia (unspecified) (n = 1, 8.3%), low response to pneumonia viruses (n = 1, 8.3%), needs intravenous immunoglobulin therapy (IVIg) (n = 1, 8.3%), and poor vaccine response (n = 1, 8.3%). Caregivers who reported that their child had antibody levels measured (n = 18, 31.6%) also reported whether IgA (n = 5, 27.8%), IgG (n = 5, 27.8%), or IgM (n = 1, 5.6%) were measured. Seven (38.9%) did not know which antibody levels were measured. Over half of caregivers who reported their child had their antibody levels measured reported their child's antibodies were lower than the expected range (n = 10, 55.6%). Types of immune disorders reported via a write-in response included: Evan's Syndrome (n = 1, 1.8%), Hashimoto's (n = 1, 1.8%), hypothyroidism (n = 1, 1.8%), immunoglobin A deficiency (n = 1, 1.8%), Lupus (n = 1, 1.8%), Vitiligo (n = 1, 1.8%), and “no immune system” (n = 1, 1.8%).
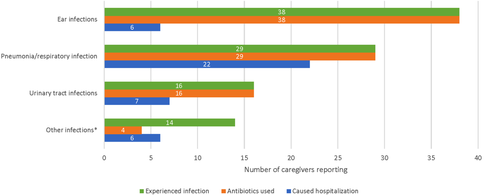
3.2.5 Infection history
The majority of caregivers reported that their child had a history of infections (n = 41, 71.9%), including ear, urinary tract, respiratory, pneumonia, and various other types of infections. See Figure 3 for a summary of infections and the number of caregivers who reported antibiotic use and hospitalizations due to those infections. The average age of onset of infections was around 1 year of age (SD: 1.5; range: <1 year old to 6 years old).
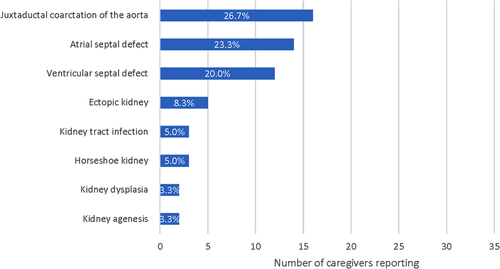
3.2.6 Heart and kidney issues
Caregivers who reported a history of heart problems reported the following conditions: juxtaductal coarctation of the aorta (i.e., narrowing of the aorta) (n = 16, 26.7%), an atrial septal defect (i.e., a hole in the wall separating the heart's upper chambers) (n = 14, 23.3%), or a ventricular septal defect (i.e., a hole in the wall separating the heart's lower chambers) (n = 12, 20.0%).
Caregivers who reported a history of renal problems reported the following conditions: ectopic kidney (i.e., kidney is in an abnormal position) (n = 5, 8.3%), kidney tract infection (n = 3, 5.0%), horseshoe kidney (i.e., two kidneys fuse together during fetal development) (n = 3, 5.0%), kidney dysplasia (i.e., kidney does not fully develop in the womb) (n = 2, 3.3%), kidney agenesis (i.e., child is born without one or both kidneys) (n = 2, 3.3%), or other kidney issues (n = 15, 26.3%). Other kidney issues reported via open response included: kidney stones (n = 5, 8.8%), kidney reflux (n = 3, 5.3%), cyst on kidney (n = 2, 3.5%), Extra duplicating system (n = 2, 3.5%), cyst on kidney in the past (n = 1, 1.8%), excess fluid (n = 1, 1.8%), pelvic kidney (n = 1, 1.8%), pelviectasis (n = 1, 1.8%), risk of kidney failure (n = 1, 1.8%), small kidney (n = 1, 1.8%), and small kidney in the past (n = 1, 1.8%). See Figure 4 for a summary of heart and kidney issues.
3.2.7 Seizure history
About a third of caregivers (n = 19, 33.3%) reported their child had a history of seizures, most of which had stopped completely without medication use (n = 8, 42.1%). Caregivers reported the average age their child's seizures started was 2 years (range: <1 year old to 7 years old) and that they had on average 2.7 seizures per year for those in which the seizures were ongoing (range: 1–4). Types of seizures reported included petit mal or absence (i.e., brief, sudden lapses of consciousness) (n = 9, 47.4%), grand mal or tonic/clonic convulsions (i.e., loss of consciousness and violent muscle contractions) (n = 5, 26.3%), temporal lobe or complex partial (i.e., often involved aura, odd feelings, and making movements with your hands or lips” (n = 4, 21.1%), and myoclonic (i.e., brief, shock-like jerks of the muscles) (n = 3, 15.8%).
3.2.8 Joint issues
Most caregivers reported that their child had a history of joint dislocations/hypermobility (n = 43, 75.4%) that did not require surgery (n = 35, 81.4%). Caregivers reported that, on average, the age of diagnosis for their child's joint issues was 2 years old (range: <1 year old to 15 years old). Types of surgeries for joint issues included: hip surgery (n = 5, 50.0%), knee surgery (n = 4, 40.0%), or surgery in some other unspecified location (n = 1, 10.0%). Additionally, 13 caregivers (22.8%) reported their child had scoliosis and that, on average, they were diagnosed at 4 years old (range: <1 year old to 14 years old); only one child was reported to receive treatment for their scoliosis.
3.2.9 Dental issues
Most caregivers reported that their child had dental issues (n = 39, 68.4%). Specific dental issues reported included: missing teeth (n = 27, 64.3%), fused teeth (n = 5, 11.9%), unusual shaped teeth (n = 18, 42.9%), and excessive cavities (n = 13, 31.0%).
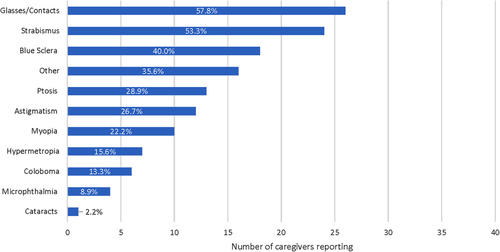
3.2.10 Ophthalmologic issues
Most caregivers reported that their child had a history of eye issues (n = 42, 73.7%). Eye issues reported by ≥50% of caregivers were wearing glasses/contacts (n = 26, 57.8%) and strabismus (i.e., eyes do not look in the exact same direction all the time, also called crossed eye) (n = 24, 53.3%). See Figure 5 for a summary of all eye issues reported. Additionally, most caregivers reported that their child sleeps his or her eyes open (n = 35, 61.4%).
3.2.11 Psychological concerns
Some caregivers reported their child had been diagnosed with anxiety (n = 15, 26.3%) and/or depression (n = 4, 7.0%). The average age of diagnosis for anxiety was 8 years old (range: 2–19 years old); for depression it was 13 years old (range: 5–20 years old). Eleven of the 15 caregivers who had children diagnosed with anxiety (73.5%) reported that the children were on medication and two of the four caregivers who had children diagnosed with depression (50.0%) reported they were on medication or in therapy. Ten (17.5%) caregivers also reported their child has autism.
3.2.12 Additional issues
Caregivers were given the opportunity to describe any additional issues their child had due to Kabuki syndrome via a write-in response on the survey. A wide range of unique responses were reported by caregivers and subsequently organized into 15 categories: behavioral problems (e.g., “obsessive behaviors” [n = 1, 1.8%]), bone, joint, muscle, or skeletal malformations (e.g., hypotonia [n = 10, 17.5%] and “limb length discrepancy” [n = 1, 1.8%]), brain/spine malformations (e.g., “Chiari 1 malformation” [n = 2, 3.5%] and “tethered spinal cord” [n = 2, 3.5%]), movement, spatial, or sensory issues (e.g., “balance issues/falling down [n = 2, 3.5%] and “motor planning challenges” [n = 3, 5.3%]), cognitive problems (e.g., “ADHD” [n = 1, 1.8%]), problems with diet or weight (e.g., “overweight” [n = 1, 1.8%]), emotional impacts (e.g., “anger issues” [n = 1, 1.8%]), gastrointestinal problems (e.g., “GI/bowel issues” [n = 4, 7.0%] and “GERD” [n = 3, 5.3%]), stunted growth (e.g., “short stature” [n = 2, 3.5%]), cardiovascular issues (e.g., “cardiac defects” [n = 2, 3.5%], pulmonary issues (e.g., “asthma” [n = 1, 1.8%]), renal issues (e.g., “kidney stones” [n = 1, 1.8%]), endocrine conditions (e.g., “Hypothyroidism” [n = 2, 3.5%]), reproductive system effects (e.g., “heavy, irregular periods} [n = 1, 1.8%]), compromised immune system (n = 1, 1.8%), and an impact on sleep (e.g., “irregular sleep” [n = 1, 1.8%]).
3.3 Caregiver life
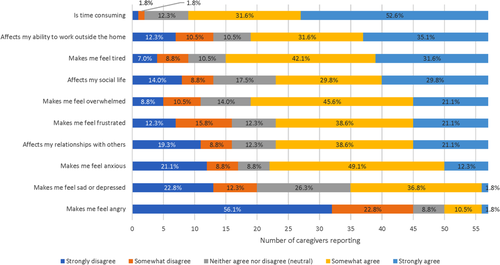
3.3.1 Caregiver burden
Caregivers were asked to rate their level of agreement with certain statements related to caring for someone with Kabuki syndrome. Caregivers most frequently “strongly agreed” with the following statements: [Caring for someone with Kabuki syndrome] “is time consuming” (n = 30, 52.6%), “affects my ability to work outside the home” (n = 20, 35.1%), and “makes me feel tired” (n = 18, 31.6%). Statements caregivers most commonly “strongly disagreed” with were [Caring for someone with Kabuki syndrome] “makes me feel angry” (n = 32, 56.1%) and “makes me feel sad or depressed” (n = 13, 22.8%). Figure 6 contains a summary of all ratings of statements related to caring for someone with Kabuki syndrome. Further, over half of caregivers (n = 34, 59.7%) reported they were not employed outside the home.
3.3.2 Most challenging aspect of caring for someone with Kabuki syndrome
Caregivers were asked to describe using free text in the survey the most challenging part about living with someone with Kabuki syndrome. A variety of unique responses were provided; the most frequent categories of responses were: frequent medical appointments (n = 9, 15.8%) (e.g., the “never ending” doctor appointments and therapy sessions that are “demanding of time, effort and money”), need for constant care (n = 8, 14.0%) (e.g., specifically, “the amount of care that goes with it,” can be “a full time job in and of itself”), and concern about the future (n = 8, 14.0%) (e.g., caregivers said it is “difficult to wonder whether or not our child will be able to do things that most people can do” and they often worry about “future health challenges”).
4 DISCUSSION
This research was conducted in order to add to the body of literature describing the characteristics and presentation of Kabuki syndrome from the novel perspective of caregivers of children with Kabuki syndrome. Caregivers are uniquely qualified to report on the multitude of health issues experienced by these patients, as they are largely responsible for their care, especially when patients are young, and can provide more reliable reports than patients who experience developmental or cognitive issues. Given the lack of patient- and/or caregiver-reported data on Kabuki syndrome found in the literature, this research helps to describe the magnitude of issues often experienced by these patients and families. Perhaps this is most evident in the frequency of visits to a wide range of treatment providers reported by caregivers and also described in existing literature, as families must find treatment providers who can help manage symptoms of physical abnormalities, cognitive impairment, socio-emotional problems, familial stress caused by chronic illness, among other various medical conditions (Kasdon & Fox, 2012). While this research does not intend to inform medical decision making in the care and treatment of patients with Kabuki syndrome, it does provide a picture of the multidisciplinary approach sought by families to manage the condition and the potential need for specialty clinics for Kabuki syndrome that seek to address these special healthcare needs and improve outcomes for this population by establishing best practices for treatment management.
The issues related to Kabuki syndrome reported by caregivers ranged from those affecting hearing, eating, and seeing (i.e., difficulty eating and swallowing, oral issues, dental issues, eye issues, hearing loss), to difficulties with the immune system and infections, to joint problems, to even more serious issues such as seizures, kidney and heart problems. Further, although not reported by the majority of caregivers, mental health issues such as anxiety and depression are also seen in this population. Even then, caregivers provided a list of additional issues not covered in the wide-ranging survey that their children experience. This both corroborates and adds to current literature describing the clinical manifestations of Kabuki syndrome and the many variations in phenotype that have been observed.
Although it is usually preferable to collect self-report of health-related quality of life, when this information is difficult to collect a proxy report is often used; in fact, the caregiver's perception of their child's health status is what determines utilization of the healthcare system (Varni, Seid, & Kurtin, 2001). As such, the difficulty in managing these many medical issues is seen in the large number of and frequency of visits to a large number of healthcare providers (in addition to a primary care physician) utilized in these patients' treatment. Caregivers also reported that one of the most challenging aspects of caring for someone with Kabuki syndrome was the frequent medical appointments. The many issues and associated need for treatment reported by caregivers suggest a significant impact on health-related quality of life in patients.
Frequent interactions with the healthcare system are just one aspect of caring for someone with Kabuki syndrome, however, and caregivers reported that living and caring for someone with Kabuki syndrome can be quite burdensome. Caregivers reported that their experience caring for someone with Kabuki syndrome was time consuming, affected their ability to work outside the home, and was tiring, among other things. In fact, many of these caregivers reported not being employed outside the home and that caring for someone with Kabuki syndrome was a “full time job.” The strain on caregivers due to the constant time commitment and worry associated with caring for Kabuki syndrome was evident in these survey responses. These data are supported by existing literature that states a patient's treatment regimen as well as their ability to manage their own illness may also lead to a greater burden on the caregiver (Javalkar et al., 2017).
Although the authors feel this novel research in caregivers of children of Kabuki syndrome is a significant addition to current literature in this disorder, there were some limitations to this survey research. Firstly, caregivers completed a screening based on self-report and no medical records were requested to verify diagnosis. However, given the active involvement of advocacy groups in recruitment and the fact the majority of participants were recruited through their outreach, the authors feel confident these caregivers were indeed members of this community. Additionally, follow-up for clarification on responses was not possible when a caregiver's answer was unclear or seemed implausible. Face-to-face interviews would allow for better assessment of caregivers' observations, thereby providing more complete data on the experience of living with someone that has Kabuki syndrome.
Of note, adults and adolescents were also asked to participate in this survey research. Adolescents were asked to complete a much shorter survey with the assistance of their caregiver if needed. Although adults were invited to participate, there was little interest from the adult community. The authors acknowledge the value of collecting patient-reported information from these groups in the future.
5 CONCLUSIONS
This research is a novel and unique characterization of the patient experience with Kabuki syndrome from the perspective of caregivers. Although there are smaller studies that summarize the clinical manifestation of Kabuki syndrome, this study is an important addition to current research given the wide range of topics covered and the large number of caregivers who participate. However, additional research is warranted to further investigate the patient perspective both in the US and other countries. Given the significant burden on both patients and their caregivers, the Kabuki syndrome community is eager to participate in and a great asset to future research endeavors, particularly because there is currently no treatment for Kabuki syndrome.
ACKNOWLEDGMENTS
Rene King, President & Founder, All Things Kabuki Inc. was essential to participant recruitment and the overall success of this study. Siobhan McDonald from Endpoint Outcomes assisted with recruitment and survey administration. Caitlin Pohl from Endpoint Outcomes contributed to the design of the study, survey administration, and data analysis. Christina Theodore-Oklota is employed by Ultragenyx Pharmaceutical Inc. who funded this research. Deborah Hartman and Deborah Hoffman were employed by Takeda Pharmaceuticals at the time this research was conducted. Chris Evans, Maggie Paulich, and Shayna Egan are employed by Endpoint Outcomes who was paid to conduct this research. Hans T. Björnsson is a consultant for Millennium Pharmaceuticals.
AUTHOR CONTRIBUTIONS
Christina Theodore-Oklota and Hans Bjornsson made significant contributions to the study design and this manuscript. CTO also gave input on data analysis. Deborah Hartman and Deborah Hoffman made contributions to the interpretation of the data and this manuscript. Shayna Egan, Chris Evans, and Maggie Paulich contributed to the study design, analyzed and interpreted all patient data collected. All authors read and approved the final manuscript.
Open Research
DATA AVAILABILITY STATEMENT
Authors can confirm that all relevant data are included in the article and/or its supplementary information files.