Myhre syndrome: A first familial recurrence and broadening of the phenotypic spectrum
Funding information: Fund for Scientific Research Flanders, Grant/Award Number: Grant G028415N to BC; Fund for Cardiac Surgery, Grant/Award Number: Grant 2015 to BC; Special Research foundation of Ghent University, Grant/Award Number: Starting grant BOFSTA2016002401 to BC
Abstract
Myhre syndrome is a rare multisystem connective tissue disorder, characterized by short stature, facial dysmorphology, variable intellectual disability, skeletal abnormalities, arthropathy, cardiopathy, laryngotracheal anomalies, and stiff skin. So far, all molecularly confirmed cases harbored a de novo heterozygous gain-of-function mutation in SMAD4, encoding the SMAD4 transducer protein required for both transforming growth factor-beta and bone morphogenic proteins signaling. We report on four novel patients (one female proband and her two affected children, and one male proband) with Myhre syndrome harboring the recurrent c.1486C>T (p.Arg496Cys) mutation in SMAD4. The female proband presented with a congenital heart defect, vertebral anomalies, and facial dysmorphic features. She developed severe tracheal stenosis requiring a total laryngectomy. With assisted reproductive treatment, she gave birth to two affected children. The second proband presented with visual impairment following lensectomy in childhood, short stature, brachydactyly, stiff skin, and decreased peripheral sensitivity. Transmission electron microscopy (TEM) of the dermis shows irregular elastin cores with globular deposits and almost absent surrounding microfibrils and suggests age-related increased collagen deposition. We report on the first familial case of Myhre syndrome and illustrate the variable clinical spectrum of the disorder. Despite the primarily fibrotic nature of the disease, TEM analysis mainly indicates elastic fiber anomalies.
1 INTRODUCTION
Myhre syndrome (MIM 139210) is a rare connective tissue disorder with multisystem involvement. Main clinical features are a short stature, facial dysmorphism, mild to moderate intellectual disability, cardiovascular defects, and skeletal anomalies. Progressive proliferative fibrosis can occur spontaneously or after trauma. This may cause skin stiffening limiting joint mobility and may increase the risk for life-threatening complications such as laryngotracheal stenosis. (Lin et al., 2016; Michot et al., 2014; Myhre, Ruvalcaba, & Graham, 1981; Starr, Lindor, & Lin, 2017).
Myhre syndrome is caused by de novo heterozygous gain-of-function mutations in SMAD4 (MIM 600993). SMAD4 encodes the common SMAD protein required for most transcriptional responses to transforming growth factor-beta and bone morphogenic protein signaling. So far, only four SMAD4 pathogenic variants have been observed in Myhre syndrome. These missense variants are all restricted to residues 496 and 500 situated in the Mad homology 2 domain. (Caputo et al., 2012; Caputo et al., 2014; Le Goff et al., 2012; Michot et al., 2014; Starr et al., 2017).
We report on a familial case of Myhre syndrome and a second adult proband with Myhre syndrome. All four patients harbor the less frequently reported SMAD4 c.1486C>T (p.Arg496Cys) mutation. Our data broaden the phenotypic spectrum of the disorder. Transmission electron microscopy (TEM) of skin biopsies of patients shows elastic fiber anomalies, classifying this disorder as an elastinopathy.
2 CLINICAL REPORT
2.1 Case 1
The proband presented when she was 38 years old. She was referred for a familial recurrence of congenital heart defects (CHD). She was born with either a patent ductus arteriosus or aortic coarctation, for which she was surgically treated at the age of 1 year. Her parents and sister are healthy. Two maternal cousins died from sudden infant death syndrome. One maternal aunt died at the age of 1 week due to cyanotic disease of unknown etiology. Her unrelated partner is healthy.
Because of primary infertility, she and her partner started with assisted reproductive treatment (ART) at the age of 30. After three unsuccessful cycles of intra-uterine insemination, intracytoplasmic sperm injection (ICSI) treatment was initiated. She had nine ICSI cycles, resulting in 10 embryo transfers of 23 embryos in total. Eight of these embryo transfers resulted in a pregnancy (seven singleton and one twin pregnancy). Six pregnancies ended in an early miscarriage. The twin pregnancy resulted in single intrauterine demise and the birth of her first child. The last pregnancy resulted in the birth of her second child. The first child, a girl, was born at term by means of cesarean section, because of prolonged labor due to cephalopelvic disproportion (narrow pelvis) and fetal distress. Birth weight was 2.620 kg (<3th centile), length at birth 49 cm (3th–10th centile) and head circumference 33 cm (<3th centile). The girl presented with a muscular ventricular septum defect and aortic coarctation for which coarctectomy was performed. Furthermore, a congenital thoracic scoliosis was noted. The second child, a boy, was also born at term by means of cesarean section. Birth weight was 2.660 kg (<3th centile), length at birth 45 cm (<3th centile) and head circumference 33 cm (3th centile). He presented with a tetralogy of Fallot (TOF) for which surgical correction was performed.
The proband weighed 76 kg (68th centile), was 159 cm tall (20th centile) and had a head circumference of 56.5 cm (53th centile). She had mild facial dysmorphic features including small low set ears, deeply set eyes, and prognathism. Furthermore, we noted a bilateral clinodactyly of the second toe, a mild scoliosis, and an extension deficit of both shoulders (limited to 90°). The girl was 4 years old, weighed 12.3 kg (<3th centile), measured 96 cm (3th–10th centile) and had a head circumference of 49 cm (25th–50th centile). She had small low set and posteriorly angulated ears, deeply set eyes with short palpebral fissures, a synophrys, a small nose with underdeveloped alae nasi, a narrow mouth with thin upper lip vermilion, and mild bilateral clinodactyly of the second toe. Like her mother, she also presented with a limited mobility of both shoulders and a severe thoracic scoliosis. She further showed joint hypermobility of both elbows and the finger joints. By the age of 11 years, the midfacial hypoplasia and prognathism were more apparent. The boy was 2 months old, weighed 3.9 kg (<3th centile), measured 53 cm (<3th centile) and had a head circumference of 36.7 cm (<3th centile). He had low set ears, widely spaced eyes with short and slightly downslanted palpebral fissures, a narrow mouth with thin upper lip vermilion, and bilateral clinodactyly of the second toe. At the time of clinical reevaluation, the boy was 7 years old and had a more visible midfacial hypoplasia and prognathism. Clinical photographs of the proband and her children are shown in Figure 1a.
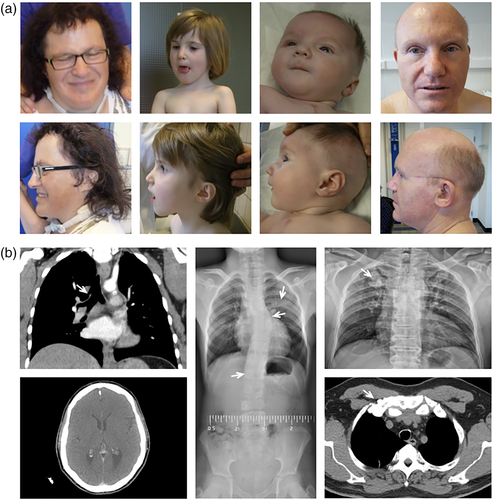
Radiographic evaluation of skeletal abnormalities showed a mild thoracic dextroconvex scoliosis and lumbar sinistroconvex scoliosis with hemisacralisation of L5 in the proband. A severe thoracic sinistroconvex scoliosis due to unilateral hypoplasia and incomplete segmentation of D5–D7, hypoplasia of the right 11th rib and absence of the right 12th rib, a partial posterior synostosis of the left fifth and sixth rib, and a lumbar dextroconvex scoliosis with a butterfly vertebra L3 were noted in the girl. The boy had a mild thoracic dextroconvex scoliosis with a butterfly vertebra D6 and a mild sinistroconvex lumbar scoliosis. Radiographs are shown in Figure 1(b). All three patients have a subjective normal hearing. However, the boy presented a mild conductive hearing loss on audiometry.
Starting from the age of 42 years, the proband developed progressive dyspnea on exertion and an inspiratory stridor due to a severe tracheal and laryngeal stenosis. Pulmonary evaluation through spirometry revealed a mildly restrictive lung function (TLC 71%, FEV1 64% and Tiffeneau-index 74%). High-resolution computed tomography of the chest was normal. A right tracheal bronchus was incidentally noted as a normal anatomic variant (see Figure 1b). The tracheolaryngeal stenosis was believed to result from previous traumatic tracheal intubation. Surgical resection of the stenosis provoked excessive growth of granulating tissue with further progression of the laryngotracheal stenosis and required a total laryngectomy. Dilatation of the trachea is performed every 2 weeks. Comparably, her son developed a fibroproliferative complication with persistent flexion contracture of the right hip after surgery for Legg-Calvé-Perthes disease at the age of 10 years.
Genetic workup showed normal karyotype in the proband and her partner. Array comparative genomic hybridization (180k arrayCGH, Agilent) revealed a 1.6 Mb duplication of chromosome band Xp22.31 (Xp22.31p22.31(6463313-8075094)x3 (hg18, NCBI Build 36.1)) in the proband and both her children. This duplication comprises the HDHD1A, STS, VCX, and PNPLA4 genes. Deletions of the STS gene region are known to result in X-linked ichthyosis in boys, but a duplication of this region is considered a normal variant. Rasopathy genes (PTPN11, SOS1, RAF1, KRAS, BRAF, MEK1, MEK2, and HRAS) were normal in the proband. JAG1 analysis revealed a likely benign paternally inherited variant c.2461G>A (p.Arg683His) (GenBank HSU73936) in both children. Eventually, exome sequencing (ES) in the proband revealed the pathogenic heterozygous c.1486C>T (p.Arg496Cys) missense variant in SMAD4 (NM_005359). The presence of this pathogenic variant was confirmed by Sanger sequencing in the proband and both her children.
2.2 Case 2
The second proband presented at the age of 46 years because of severe visual impairment since birth, autism spectrum disorder, and progressive skin stiffening with restricted joint mobility. He had decreased sensitivity in hands and feet complicated by recurrent painless deep skin fissures in his soles. His parents, three half-brothers and two half-sisters on the maternal side are all healthy. He has no offspring.
Clinical examination revealed a short stature (<3th centile), macrocephaly (>98th centile), a yellow-orange color of the skin, and a yellowish discoloration of the teeth. He had a broad nasal tip, relatively low set ears, and prognathism. Clinical photographs are shown in Figure 1a.
Ophthalmologic evaluation showed a status post bilateral lens extraction, severe hypermetropia and thickened sclerae with short axial length. He has a subjective normal hearing. Audiometry showed an age-related high frequency hearing loss. Radiography of the spine, pelvis, and extremities showed mild degenerative osteoarthrosis, broad ribs with exostoses on the first and second ribs (see Figure 1b), Achilles tendon fibrosis, and lumbar discopathy. Somatosensory evoked potentials of both lower limbs were severely decreased. Echocardiography was normal.
Initial genetic workup through arrayCGH analysis was normal. Stiff skin syndrome was excluded by Sanger sequencing of exon 37 and 38 of the FBN1 gene. Also next-generation sequencing of the Weill-Marchesani syndrome-related genes FBN1, ADAMTS10, ADAMTS17 and LTBP2 was normal. Eventually, ES revealed the pathogenic heterozygous c.1486C>T (p.Arg496Cys) missense variant in SMAD4 (NM_005359). Coincidentally, we also detected a pathogenic c.509C>T (p.Thr170Met) BCO1 variant (NM_017429) compatible with hypercarotenemia and mild hypovitaminosis A. This might explain the yellow-orange discoloration of the skin and teeth. Both variants were confirmed by Sanger sequencing.
3 TRANSMISSION ELECTRON MICROSCOPY
TEM of a skin biopsy of all four patients was performed. Samples were fixed in a 4% formaldehyde, 2.5% glutaraldehyde, 0.1 M cacodylate buffer solution. After washing in buffer solution, samples were post-fixed in 1% OsO4 with K3Fe(CN)6 in 0.1 M sodium cacodylate buffer (pH 7.2) and subsequently dehydrated through a graded ethanol series, including a bulk staining with 2% uranyl acetate at the 50% ethanol step followed by embedding in Spurr's resin. Ultrathin sections of a gold interference color were cut using a Leica EM UC6 ultra microtome (Leica Microsystems), followed by consecutive post-staining in uranyl acetate and lead stain in a Leica EM AC20 (Leica Microsystems). Sections collected on formvar-coated copper slot grids were viewed with a JEOL JEM 1400plus transmission electron microscope (TEM) (JEOL, Tokyo, Japan) operating at 80 kV.
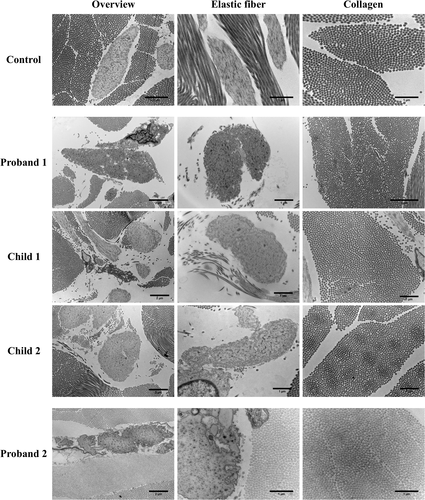
TEM images are displayed in Figure 2. In control skin biopsies, elastic fibers demonstrate a solid, dense core of elastin surrounded by a sparse mantle of microfibrils. Collagen fibers in control skin biopsies are composed of regular sized collagen fibrils and are homogenously spread between the elastic fibers. In all four patients with Myhre syndrome, TEM of the dermis shows ultrastructural abnormalities of the extracellular matrix. The elastic fibers show irregular elastin cores with globular deposits, fragmentation of the periphery of the fiber resulting in disintegration of the elastin core and almost absent surrounding microfibrils. The collagen appears structurally normal, though more densely packed.
4 DISCUSSION
Myhre syndrome is a sporadic condition characterized by a short stature and stocky muscular build, recognizable facial dysmorphism, mild to moderate intellectual disability, skeletal, cardiovascular, and respiratory anomalies. Patients have an increased risk for cardiopulmonary complications due to progressive and proliferative fibrosis. (Lin et al., 2016; Michot et al., 2014; Myhre et al., 1981; Starr et al., 2017) The first proband and her both children presented with a mainly cardiovascular, skeletal, and facial dysmorphic phenotype. They all presented with a CHD and vertebral abnormalities. TOF has only been described once before in Myhre syndrome. (Alagia et al., 2018) Both the mother and her son present posttraumatic progressive proliferative fibrotic complications, respectively laryngotracheal stenosis and a persistent flexion contracture of the hip. The second proband presented with visual impairment following lensectomy in childhood, short stature, and stiff skin. The exact reason for the lensectomy in childhood could not be retrieved. As bilateral ectopia lentis was assumed, a clinical diagnosis of Weill-Marchesani syndrome was made. Based on previously reported ophthalmological findings in Myhre syndrome, we assume that the patient might instead have suffered from bilateral congenital cataract instead. (Alagia et al., 2018)
In both probands, the diagnosis was delayed beyond the fourth life decade and eventually revealed with ES. This illustrates the difficulty of correctly and timely diagnosing patients with Myhre syndrome. Myhre syndrome is still widely unrecognized, even in classic cases. The phenotype is variable, both in severity and organ system involvement. The craniofacial, skin and joint features become more prominent with age and can be missed in younger children. (Garavelli et al., 2016) In addition, the familial presentation in Case 1 and the presumed lens ectopy in Case 2 were misleading. These cases illustrate that ES is useful to resolve a long-lasting diagnostic odyssey and might enable a more timely diagnosis in such patients. A timely diagnosis is of utmost importance because of the risk for potential life-threatening (iatrogenic) fibroproliferative complications, including laryngotracheal stenosis and pericardial effusion. (Garavelli et al., 2016; Oldenburg et al., 2015; Starr et al., 2017) This justifies regular cardiological and otorhinolaryngological follow-up in Myhre syndrome patients, and warrants a careful planning of surgery with adjusted pre-, per- and postoperative airway management to prevent laryngotracheal stenosis. (Garavelli et al., 2016; Oldenburg et al., 2015)
Thus far, patients were not known to reproduce and fertility has never been assessed. (Lin et al., 2016; Starr et al., 2017) The first case in this report illustrates that reproduction in Myhre syndrome is possible, especially in an era of ART and at least for affected females. Although coincidental occurrence was not ruled out, the need for ICSI treatment with a high number of unsuccessful embryo transfers and early spontaneous abortions suggest reduced fertility. Preimplantation genetic testing may become a considerable option for patients with Myhre syndrome.
Myhre syndrome is caused by recurrent missense mutations in SMAD4. All four patients reported here, harbor the pathogenic heterozygous p.Arg496Cys variant in SMAD4, which has thus far been reported less frequently than the three missense mutations affecting p.Ile500.(Caputo et al., 2012; Caputo et al., 2014; Le Goff et al., 2012; Lin et al., 2016; Michot et al., 2014) Clear genotype–phenotype correlations have not been reported so far. Cardiovascular features were not yet reported in patients harboring the p.Arg496Cys mutation. (Starr et al., 2017) However, our cases do indicate the possible occurrence of cardiovascular problems in patients with this genotype.
Our TEM evaluations of skin biopsies provide clues for the ultrastructural basis underlying the progressive connective tissue fibrosis in Myhre syndrome. The prominent elastic fiber abnormalities on TEM (including peripheral fragmentation, globular deposits and almost absent surrounding microfibrils) are in line with the previously observed impaired microfibril deposition in Fibrillin-1 staining of fibroblast cultures of Myhre syndrome patients. (Piccolo et al., 2014) The collagen fibers appear structurally normal but more densely packed in both adult patients, but not in the children. Taken as a whole, elastic fiber abnormalities appearing before increased collagen deposition may reflect the clinically observed progressive stiffness of the skin in Myhre syndrome patients. It is therefore tempting to speculate that aberrant growth factor signaling links elastic fiber abnormalities to secondary fibrotic changes. This hypothesis, if confirmed, may be relevant to understand the pathogenesis of common fibrotic conditions such as systemic sclerosis.
In conclusion, Myhre syndrome patients may reproduce, though reduced primary fertility is highly probable. Offering preimplantation genetic testing could be considered. Despite the wide clinical variability, the need for an early diagnosis is imposed by the risk for possible iatrogenic fibrotic complications from tracheal intubation and surgery. TEM of the skin of Myhre syndrome patients points primarily to an elastinopathy that may relate to later onset collagen deposition and the fibrotic nature of the disease.
ACKNOWLEDGMENTS
B. C. is a senior clinical investigator funded by the Fund for Scientific Research Flanders (FWO). This project was funded by the Special Research foundation of Ghent University (starting grant BOFSTA2016002401 to B. C.), the Fund for Scientific Research Flanders (grant G028415N to B. C.), and the Fund for Cardiac Surgery (grant 2015 to B. C.). We are thankful to the patients for their interest and participation. Ghent University Hospital is a member of the following European reference networks (ERN) relevant for this work: ERN-skin and ERN ReCONNET.
AUTHOR CONTRIBUTIONS
I. M. and B. C. designed and coordinated the study, drafted the manuscript and revised it critically for important intellectual content. I. M., B. C., K. B., T. D. B., S. J., J. P., F. P., and D. D. W. contributed to the acquisition of the clinical patient data. I. M., W. S., and B. C. contributed to the acquisition of the molecular patient data. A. B. and R. D. R. performed TEM imaging on skin biopsies of the patients. All authors revised the manuscript critically for important intellectual content and gave final approval of the version to be published. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.