Clinical and molecular cytogenetic characterization of four unrelated patients carrying 2p14 microdeletions
Abstract
We report the clinical and molecular cytogenetic characterization of four unrelated patients from France and Spain, carrying 2p14 microdeletions and presenting with intellectual disability and dysmorphisms. 2p14 microdeletions are very rare. Seven patients have been reported so far harboring deletions including 2p14p15 and encompassing OTX1, whose haploinsufficiency is frequently associated with genitourinary defects. To date, only one patient has been reported carrying a more proximal 2p14 microdeletion which does not include OTX1. Here, we report three further patients carrying proximal 2p14 microdeletions not including OTX1 and one patient carrying a more distal 2p14p15 microdeletion including this gene, providing new insights into the associated phenotypic spectrum. First, our study and a review of the literature showed that 3/4 patients carrying proximal 2p14 microdeletions had sensorineural hearing loss, suggesting the presence of a previously unreported deafness-causing gene in this chromosomal region. Second, one patient developed a progressive cardiomyopathy, suggesting that a cardiac follow-up should be systematically warranted even in the absence of congenital heart disease. We speculate that ACTR2 and MEIS1 might respectively play a role in the pathogenesis of the observed deafness and cardiomyopathy. Third, we observed other previously unreported features such as glaucoma, retinopathy, and mild midline abnormalities including short corpus callosum, hypospadias and anteriorly placed anus. Finally, the patient carrying a 2p14p15 deletion including OTX1 had normal kidneys and genitalia, thus confirming that OTX1 haploinsufficiency is not invariably associated with genitourinary defects. In conclusion, our study contributes significantly to delineate the phenotypic spectrum of 2p14 microdeletions.
1 INTRODUCTION
Chromosomal Microarray (CMA) has allowed the characterization of an increasing number of syndromes, named after the underlying chromosomal unbalance, whose clinical phenotype, natural history, and prognosis are often poorly characterized. Even if microdeletions caused by non-allelic homologous recombination (NAHR) of repeated duplicons in flanking regions generally have a relatively homogeneous size, their clinical phenotype is often characterized by a variable expressivity, making the prognosis prediction difficult. It is even more challenging, for clinical geneticists, to evaluate the prognosis of patients carrying “unique” non-recurrent deletions: information available in the literature is often very poor, mostly concerning only partially overlapping microdeletions.
Microdeletion 2p14 represents a typical example of the latter group of diseases. Seven patients have been reported to date harboring 2p14 deletions with distal breakpoints localized between 2p15 and 2p16 and including the OTX1 gene (OMIM: *600036), whose haploinsufficiency is frequently associated with genitourinary defects (Hancarova et al., 2013; Jorgez et al., 2014; Wohlleber et al., 2011). Nevertheless, only one patient has been reported so far carrying a more proximal 2p14 microdeletion not including OTX1 (Wohlleber et al., 2011).
We report the clinical and molecular cytogenetic characterization of four unrelated patients, among whom three carried proximal 2p14 microdeletions not including OTX1 and one carried a more distal 2p14p15 microdeletion including this gene, thus providing new insights into the associated phenotypic spectrum.
2 CLINICAL REPORT
Patients were recruited through the AChroPuce French national network, including 12 cytogenetic laboratories performing CMA.
2.1 Patient 1
This boy is the second child of non-consanguineous healthy parents. The mother previously had three miscarriages and an older brother was in a good health. During the pregnancy, amniocentesis was performed because of increased nuchal translucency, and standard karyotype was normal.
He was born at term; birth weight was 2730 g (10th centile); length was 48 cm (−1 SD) and occipital frontal circumference (OFC) was 32.5 cm (−2 SD). Bilateral inguinal hernia was surgically treated at the age of 3.5 months.
He had laryngo-tracheomalacia, requiring laser treatment as well as nocturnal non-invasive ventilation (continuous positive airway pressure) from 2.5 to 13 months of age. He also had bronchial hyperreactivity and multiple respiratory infections. An immunological assessment performed at 4 months of age, including full blood count, lymphocytes subpopulations, and immunoglobulin subclasses, did not show significant anomalies. Chest computer tomography, performed at the age of 2.5 months, showed tracheal anterior compression by brachiocephalic artery, left superior vena cava and the absence of left brachiocephalic vein.
The boy had severe feeding problems, recurrent vomiting, and failure to thrive. Cow milk protein allergy, gastroesophageal reflux, and a gastric plication were diagnosed and he underwent gastrostomy and anti-reflux surgery at 14 months of age. Nocturnal enteral feeding was required from 6 months to 6 years of age. Abdominal ultrasound scan (USS) was normal.
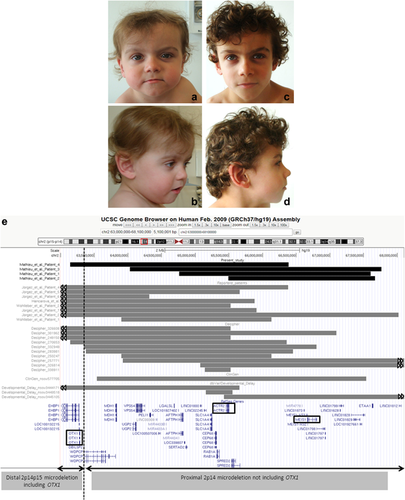
Stature was initially normal. At the age of 2 years, OFC was 47.8 cm (−1 SD); height was 82.5 cm (−1 SD) and weight was 10.880 kg (10th centile). Clinical examination showed mild dysmorphic features, such as large and squared forehead, synophrys, apparent widely spaced eyes, hooded eyelids, left intermittent exotropia, thin lips, large ears, and short neck (Figure 1a,b). He progressively developed short stature and, at the age of 3 years and 9 months, his height was 91.5 cm (−2.5 SD). At the age of 5 years, growth hormone (GH) deficiency was diagnosed on the basis of clonidine and insulin stimulation tests and GH treatment led to significant improvement. At 6 years and 10 months of age (Figure 1c,d), height was 114 cm (−1 SD), weight was 20 kg (25th centile), and OFC was 51 cm (−1 SD). Magnetic resonance imaging (MRI) showed normal hypothalamus and pituitary gland.
Developmental delay became progressively evident: the boy started sitting at 15 months, crawling at 22 months, and walking independently at 30 months of age. He pronounced his first words at the age of 3 years. Hearing test was normal. Brain MRI, performed at 1 year of age, showed mild frontal ventricular dilatation. Electroencephalogram at 2 years of age was normal. He attended a school for children with special needs, and he had speech and occupational therapy. A formal neuropsychological assessment by Psychoeducational Profile-third edition (PEP-3), performed at 4 years and 4 months of age, confirmed a global developmental delay (Table in supplemental information); the Vineland Adaptive Behavior Scales confirmed expressive language difficulties, mild motor difficulties, good socialization, and good daily living skills (except toilet training which was still not achieved). Conners test did not show any major behavioral problem. A new neuropsychological assessment by Wechsler Preschool and Primary Scale of Intelligence III performed at the age of 7 years and 2 months confirmed ID (Table in supplemental information).
Repeated echocardiographies (at the age of 11 days and 23 months) were normal. A heart murmur was firstly noted at the age of 30 months during a respiratory infection and a further echocardiography revealed the occurrence of hypertrophic cardiomyopathy with sub-aortic muscular hypertrophy. Treatment by Verapamil was required from the age of 5 years and 6 months.
Standard karyotype, fluorescent in situ hybridization (FISH) for chromosome 22q11 microdeletion, thyroid function tests, plasma amino acids, urine organic acids, urine mucopolysaccharides, and oligosaccharides were normal.
CMA, performed using an oligo 180k quatuor Agilent® array according to the manufacturer's instruction (Agilent Technologies, Santa Clara, CA) and DNA Analytics 4.0 for data analysis, showed a 2p14 microdeletion not including OTX1: arr[GRCh37] 2p14(64,745,676 × 2,64,761,134-67,602,027 × 1,67,619,813 × 2) (Figure 1e; Table 1). FISH analysis, performed in the child and both parents using the RP11-547F18 probe, confirmed the de novo occurrence of this chromosomal unbalance.
| Proximal 2p14 deletions not including OTX1 | Distal 2p14p15 deletions including OTX1 | |||||
|---|---|---|---|---|---|---|
| Main features | Pt 1 (present study) | Pt 2 (present study) | Pt 3 (present study) | Previously reported Pta | Pt 4 (present study) | Previously reported Ptsb |
| Deletion size (Mb) | 2.8 | 2.17 | 3.7 | 2.23 | 3.3 | 2.75–6.31 |
| Breakpoints (Hg19) | 64,761,134–67,602,027 | 65,490,660–67,666,133 | 64,029,271–67,760,781 | 63,903,236–66,130,003 | 63,140,968–66,353,450 | na |
| Gender | M | M | M | M | M | 6 M/1 F |
| Age | 7 y | 1 y 7 m | 6 m | 8 y 3 m | 2 y 2 m | 21 m–16 y |
| Dysmorphic features | + | + | + | + | + | 7/7 |
| OFC ≤ −2 SD | − | − | NA | + | + | 3/7 |
| Large/high forehead | + | + | + | + | − | 0/7 |
| Hooded eyelids | + | + | − | + | − | 2/7 |
| Large/prominent ears | + | − | + | − | − | 3/7 |
| Low set years | − | − | + | + | + | 1/7 |
| Bulbous nasal tip | − | + | − | + | + | 2/7 |
| Thin upper lip | + | − | + | + | − | 4/7 |
| Developmental delay | + | + | + | + | + | 7/7 |
| Brain anomalies | Mild ventricular dilatation | Short corpus callosum | − | − | − | 2/3 |
| Seizures | − | − | − | + | − | 1/7 |
| Heart involvement | Hypertrophic cardiomyopathy | PFO at 6m | − | − | − | 1/7 (PDA) |
| Hearing loss | − | + | + | + | − | 0/2 |
| Eye involvement | Intermittent exotropia | Bilateral glaucoma | Rod degeneration | Mild hyperopia | − | 3/7 |
| Feeding problems | + (FT; EF) | + (FT; PF/EF) | + | + | − | 3/7 |
| Short stature | + (GH deficiency) | − | − | − | − | 1/7 |
| Genitourinary defects | − | Balanic hypospadias | − | − | − | 5/7 |
- Pt, patient; M, male; F, female; +, reported; −, not reported; MRI, magnetic resonance imaging; PFO, persistent foramen ovale; PDA, persistent ductus arteriosus; y, years; m, months; OFC, occipital frontal circumference; FT, failure to thrive; EF, enteral feeding; PF, parenteral feeding; NA, not available; na, not applicable.
- a Pt 1 of Wohlleber et al. (2011).
- b Pt 2 of Wohlleber et al. (2011), Pt of Hancarova et al. (2013), and Pts 2, 4, 5, 6, 7 of Jorgez et al. (2014).
2.2 Patient 2
This boy was the first child of non-consanguineous healthy parents. A maternal half-sister and two paternal half-sisters were in good health.
He was born at term after an uneventful pregnancy. At birth, an anteriorly placed anus and balanic hypospadias were noted. At 4 months of age, he developed a severe eczema and failure to thrive with a significant weight loss, requiring parenteral feeding for 1 month and, subsequently, enteral feeding. A severe cow milk protein allergy was diagnosed.
Bilateral glaucoma was diagnosed at 6 months of age, requiring urgent surgery; auditory evoked potentials showed profound deafness requiring hearing aids.
On clinical examination, at 6 months of age, his weight was 5.610 kg (<3th centile), and OFC was 42 cm (−1 SD). Dysmorphic features included dolichocephaly with high forehead, prominent ears with mildly uplifted lobules, a small mouth with down-turned corners, high arched palate, a small upturned nose with depressed nasal bridge and anteverted nares, dry skin, and deep-set toe nails. No limb abnormalities were noted. He was able to hold his head and had axial hypotonia. At 1 year of age, length was 71.5 cm (−1 SD); weight was 7.500 kg (3th centile); and head circumference was 45 cm (−1 SD). Developmental delay was noted: he could not sit independently and did not say any word. He was reviewed at 19 months of age: he walked nearly independently, he expressed himself by screaming but he could not babble. Loose joints, mild lower limb hypertonia, and brisk reflexes were noted as well as stereotypic movements. He had speech and occupational therapy. Enteral nutrition was still needed during the night; the child was able to eat mixed food and had constipation.
Echocardiography performed at 6 months of age showed only persistent foramen ovale. Abdominal USS and skeletal survey were normal. Brain MRI showed short corpus callosum. Standard karyotype, FISH analysis for 22q11 microdeletion, molecular analysis of CX26 and SALL1 were all normal.
Genome wide copy number analysis was performed using Illumina® HumanCytoSNP12 BeadChip (Illumina, San Diego, CA) which contain 300,000 markers including 200,000 SNPs. Samples were processed using Infinium assay as previously described (Steemers et al., 2006) and data were analyzed by examining signal intensity (Log R ratio, i.e., ln: sample copy number/reference copy number) and allelic composition (B allele frequency/BAF with GenomeStudio V1.1 and CNV PartitionV2.4.4.0 software). Results were confirmed by FISH, using the RP11-263L17 probe. These analyses showed a de novo 2p14 microdeletion, not including OTX1: arr[GRCh37] 2p14(65,481,008 × 2,65,490,660-67,666,133 × 1,67,674,538 × 2) (Figure 1e; Table 1).
2.3 Patient 3
This boy is the first child of non-consanguineous healthy parents. The mother underwent amniocentesis during her pregnancy because of abnormal first trimester markers, and standard karyotype was normal. He was born at term: birth weight was 2.960 kg (10–25th centile) and length was 49 cm (−1 SD) (OFC not available).
He had gastroesophageal reflux. Bilateral hearing loss was diagnosed at 6 months of age, requiring right cochlear implantation. He had lower limb spasticity, requiring left foot Achilles tenotomy, and mild to moderate ID. He also showed mild facial dysmorphisms, including high and squared forehead, large and low set ears, thin upper lip and down-turned corners of the mouth.
Ophthalmological assessment revealed arteriolar sclerosis and granular aspect of the macula and electroretinogram was consistent with rod degeneration; clinically, the child had no visual impairment. At the age of 13 years, weight was 30 kg (<3rd centile), and height was 148 cm (−0.5 SD). Brain MRI and abdominal USS were normal, and he did not have heart murmur.
Molecular cytogenetic analyses, performed using the same techniques as patient 2, showed the presence of a 2p14 microdeletion not including OTX1: arr[GRCh37] 2p14(64,022,996 × 2,64,029,271-67,760,781 × 1,67,766,949 × 2) (Figure 1e; Table 1). Unfortunately, parental samples were not available.
2.4 Patient 4
This boy was born at term, to non-consanguineous healthy parents, after an uneventful pregnancy. Amniocentesis was performed for maternal age and standard karyotype was normal.
At birth, weight was 3340 g (25th centile); length was 47 cm (−2 SD); and OFC was 34 cm (−1 SD). Umbilical hernia was noted.
He presented with developmental delay: he started sitting at 7 months, and walking independently at 22 months; at 2 years he was able to pronounce 3 words and, at the age of 4 years and 8 months, there was still no structured language. He had no significant feeding problem.
The patient was referred to the genetic department at 22 months of age. Height was 85 cm (+0.5 SD); weight was 11.380 kg (−0.5 SD), and OFC was 46.5 cm (−2 SD). His facial features included a bulbous nasal tip, a long columella, a long philtrum, wide spaced teeth, low set ears, and down-turned corners of the mouth. Clinical examination was otherwise normal and there was no heart murmur. Hearing and vision were normal as was brain MRI performed at 2 years and 2 months. Renal USS was normal.
Molecular cytogenetic analysis was performed using an oligo 60k Agilent® array according to the manufacturer's instructions. Data were analyzed with ADM2 algorithm and CMA results were confirmed by quantitative polymerase chain reaction.
These analyses revealed a de novo 2p14p15 deletion, including OTX1: arr[GRCh37] 2p14(63,101,463 × 2,63,140,968-66,353,450 × 1,66,484,262 × 2) (Figure 1e; Table 1).
3 DISCUSSION
We report four unrelated patients carrying microdeletions including 2p14. Currently, there is limited information available in the literature concerning the clinical phenotype associated with this rare chromosomal unbalance. Two patients have been reported carrying a 2p14 microdeletion associated with a 5q23.2 duplication which were the result of a familial complex rearrangement involving chromosomes 2p, 22q, and 5q (Fonseca et al., 2015); as compared with other family members carrying variable chromosomal rearrangements, these two patients showed more severe learning disabilities. The authors speculated that the presence of the 2p14 microdeletion might explain the observed difference in the severity of the neurological involvement. Nevertheless, given the coexistence of the 5q duplication, it is difficult to formally ascertain the contribution of 2p14 microdeletion to the observed clinical phenotype.
“Pure” 2p14 microdeletions are very rare: only one patient has been reported in the literature carrying proximal 2p14 microdeletion not including the OTX1 gene and seven patients have been described harboring larger 2p14 deletions including this gene (Figure 1e) (Hancarova et al., 2013; Jorgez et al., 2014; Wohlleber et al., 2011). Fourteen further microdeletions have been included in the databases DECIPHER (https://decipher.sanger.ac.uk/), ClinGen (https://www.clinicalgenome.org/), and dbVar/Developmental delay (www.ncbi.nlm.nih.gov/dbvar/variants/) (Figure 1e), but the available information concerning the associated clinical phenotypes is very poor.
Table 1 summarizes the main clinical features observed in the four patients here described and in those previously reported in the literature. A few patients appear to share some facial features such as large forehead, hooded eyelids, large and low set ears, a bulbous nasal tip, and thin upper lip. Nevertheless, it is difficult to define a recognizable “2p14 microdeletion facies,” given the heterogeneity of the size of the reported microdeletions and the variable expressivity. All patients showed variable degree of ID. On the basis of the observed overlap between the reported 2p14 microdeletions, it has been speculated that a few genes might contribute to the pathogenesis of ID, including RAB1A (OMIM: *179508), involved in vesicle traffic from the endoplasmic reticulum to the Golgi, and ACTR2 (OMIM: *604221), coding for an actin-related protein involved in multiple cytoskeleton functions (Fonseca et al., 2015).
The present study and the review of the literature show that three out of four patients carrying proximal 2p14 microdeletions (not including OTX1) have sensorineural hearing loss. To the best of our knowledge, no deafness-causing gene has been reported to date in this chromosomal region. It is interesting to notice that mutations in either ACTG1 (OMIM: *102560), coding for cytoplasmic gamma-actin, or in other genes interacting with actin are known to cause syndromic and nonsyndromic deafness (Zhu et al., 2003): we speculate that haploinsufficiency of ACTR2 might play a role in the pathogenesis of the observed hearing loss, given also its high probability of loss of function intolerance (PLI) (1.00) (http://exac.broadinstitute.org/).
We report here some developmental abnormalities which had not been previously described in association with 2p14 microdeletions. Patient 1 developed a non-congenital progressive hypertrophic cardiomyopathy, thus suggesting that repeated cardiac evaluations should be systematically warranted for patients carrying 2p14 microdeletions, even in the absence of congenital heart disease. It is interesting to notice that the gene MEIS1 (OMIM: *601739) is a critical regulator of the cardiomyocyte cell cycle: it has been demonstrated that deletion of Meis1 in mouse was sufficient to induce reactivation of cardiomyocytes mitosis in the adult heart (Mahmoud et al., 2013). We speculate that the haploinsufficiency of this gene, showing a high PLI (0.99) (http://exac.broadinstitute.org/), might play a role in the development of the observed progressive hypertrophic cardiomyopathy.
Our report also expands the spectrum of eye abnormalities associated with 2p14 microdeletion, which include glaucoma (patient 2), and retinopathy (patient 3). Other previously unreported features include mild midline abnormalities, such as short corpus callosum, hypospadias and anteriorly placed anus (patient 2), and lower limb spasticity (patients 2 and 3).
Feeding problems of various origins (gastroesophageal reflux, severe cow milk protein intolerance), possibly leading to parenteral or enteral nutrition, seem to be frequent findings in patients with 2p14 microdeletions (Table 1), even in the absence of severe neurological involvement.
Overall, the 2p14 microdeletion phenotype appears to be different from that associated with more distal microdeletions. Patients carrying 2p15p16 microdeletions generally show intrauterine growth retardation, short stature, dysmorphic features including microcephaly, moderate to severe developmental delay, autistic spectrum disorder, and genitourinary malformations (Fannemel et al., 2014). It has been suggested that haploinsufficiency of OTX1 (OMIM: *600036) might play an important role in the pathogenesis of the genitourinary malformations frequently observed in microdeletions involving 2p15 (Jorgez et al., 2014). Among the four patients here reported, the only patient carrying a microdeletion including OTX1 (patient 4) did not show genitourinary defect, while patient 2 carrying a more proximal deletion not including this gene did show hypospadias. This confirms that haploinsufficiency of OTX1 is not sufficient to cause genitourinary malformations, as previously reported (Jorgez et al., 2014), and suggests that other genes localized in 2p14 are involved in genitourinary development.
The discrepancies between the observed clinical pictures and the phenotype expected on the basis of the genes included in 2p14 microdeletions, might be tentatively explained by variable disruptions of Topologically Associating Domains (TADs) resulting in ectopic enhancer-promoter interactions affecting gene expression (Lupiáñez, Spielmann, & Mundlos, 2016).
In conclusion, we report the clinical and molecular cytogenetic characterization of four unrelated patients carrying 2p14 microdeletions, thus providing new insights into the phenotypic spectrum associated with this very rare chromosomal unbalance.
ACKNOWLEDGMENTS
We would like to thank Dr. Christelle Rodier Bonifas, Service d'ophtalmologie, Hôpital Edouard Herriot, Hospices Civils de Lyon, France, for her clinical opinion and expertise.
CONFLICT OF INTEREST
All authors do not have any conflict of interest.