Three families with mild PMM2-CDG and normal cognitive development
Abstract
Congenital disorders of glycosylation (CDG) are caused by defective glycosylation of proteins and lipids. PMM2-CDG is the most common subtype among the CDG. The severity of PMM2-CDG is variable. Patients often have a recognizable phenotype with neurological and multisystem symptoms that might cause early death. We report six patients from three families who are diagnosed with a clinically mild PMM2-CDG and have normal cognitive development. All these patients had delayed gross motor skills with mild-to-moderate neurological findings. Cerebellar hypoplasia was detected in all siblings for whom brain MRI was performed. In 5/6 children the Wechsler Intelligence Scale for Children (WISC) showed normal cognitive development with full scale IQ scores ranging from borderline to average. Four patients were diagnosed with PMM2-CDG at the age of 8 years or later as their neurological symptoms were quite mild and they had been able to participate in regular school programs. We report patients with p.Val231Met/p.Arg239Trp and p.Ile120Thr/p.Gly228Cys genotypes which may cause milder variants of PMM2-CDG.
1 INTRODUCTION
Congenital disorders of glycosylation (CDG) are a group of inherited diseases characterized by defective glycosylation of proteins and lipids. The most common subtype of CDG is PMM2-CDG, which is recessively inherited. Mutations in PMM2 cause reduced activity of phosphomannomutase (PMM), which is the enzyme that converts mannose 6-phosphate to mannose 1-phosphate. This causes disturbed dolichol-oligosaccharide synthesis and eventually leads to hypoglycosylation of glycoproteins (Van & Jaeken, 1995).
The clinical phenotype of PMM2-CDG ranges from mild to severe. It can affect many organs and usually involves the central nervous system. During infancy, PMM2-CDG often presents with inverted nipples, fat pads, strabismus, axial hypotonia, and hyporeflexia. Severely affected patients also have visceral symptoms in addition to severe intellectual disability (ID) and other neurological findings. Mortality is around 20% in the first years of life (Hagberg, Blennow, Kristiansson, & Stibler, 1993; Kjaergaard, Schwartz, & Skovby, 2001). In rare patients, a much milder clinical presentation is described, where strabismus, hypotonia, cerebellar hypoplasia, mild-to-moderate ID, and higher residual PMM2 activity in fibroblasts are seen; whereas dysmorphic features, epilepsy, and stroke-like episodes are much less frequent (Barone et al., 2015; Grunewald, Schollen, Van Schaftingen, Jaeken, & Matthijs, 2001).
Here, we report six patients of three families from Estonia, the Netherlands, and the United States, who have clinically very mild PMM2-CDG with normal cognitive development.
2 CLINICAL REPORT
2.1 Family A
In family A (Table 1), the parents of the siblings are non-consanguineous, and all children were born at term after an uncomplicated pregnancy and delivery. PMM2-CDG was first diagnosed in the youngest sibling (A1) at the age of 10 months. She presented with delayed motor skills, muscular hypotonia, truncal ataxia, and strabismus. She was not crawling and sat insecurely. However, her cognitive development and growth parameters were appropriate for her age. She started to walk independently at the age of 21 months.
| Proband A1 | Proband A2 | Proband A3 | Proband B1 | Proband B2 | Proband C1 | |
|---|---|---|---|---|---|---|
| Age at diagnosis | 10 months | 16 years | 8 years | 10 years | 8 years | 1 year |
| Current age sex | 2 years female | 18 years male | 10 years female | 16 years female | 14 years male | 7 years female |
| PMM2 mutations | p.Val231Met/ p.Arg239Trp | p.Val231Met/ p.Arg239Trp | p.Val231Met/ p.Arg239Trp | p.Cys241Ser/ p.Arg141His | p.Cys241Ser/ p.Arg141His | p.Ile120Cys/ p.Gly228Cys |
| Transferrin isoelectric focusing pattern | Type 1 | Type 1 | Type 1 | Type 1 | Type 1 | Type 1 |
| PMM activity mU/mg protein in fibroblastsa | N/A | 1.6 (4.7–9.2) | N/A | 2.1 (6.7–11.2) | N/A | N/A |
| Gross motor skills | Walked at 19 months | Walked at 19 months | Walked at 21 months | Walked at 22 months | Walked at 20 months | Walked at 5 years |
| Fine motor skills | Disturbed | Disturbed | Slightly disturbed | Slightly disturbed | Disturbed | Disturbed |
| Neurological findings | Hypotonia, body ataxia | Previously hypotonia, ataxia; presently slight ataxia, slow and dysarthric speech | Previously ataxia; presently clumsiness | Previously mild hypotonia | Previously mild hypotonia, slow and dysarthric speech | Previously hypotonia, ataxia; presently slight ataxia, dysarthric speech |
| Full scale IQb | N/A | 72 B | 81 LA | 93 A | 72 B | 83 LA |
| Verbal comprehension | N/A | 79 B | 77 B | 78 B | N/A | 77 B |
| Perceptual organization | N/A | 73 B | 90 A | 89 A | N/A | 90 A |
| Working memory index | N/A | 97 A | 83 LA | 99 A | N/A | 83 LA |
| Processing speed | N/A | 62 EL | 91 A | 80 LA | N/A | 91 A |
| Educational level at the time of diagnosis | N/A | High school | Elementary school | Elementary school | Elementary school | N/A |
| Brain MRI | N/A | Cerebellar hypoplasia with enlarged fourth ventricle | Cerebellar hypoplasia with enlarged fourth ventricle | N/A | Cerebellar hypoplasia | Cerebellar hypoplasia with vermis hypoplasia |
| Ophthalmologic findings | Strabismus | Normal | Strabismus | Normal | Strabismus | Strabismus |
| Antithrombin III (%)a | 63 (101–131) | 46 (96–126) | 80 (95–134) | Normal | Normal | Low |
| Free protein C (%)a | 68 (65–127) | 54 (66–118) | 69 (71–129) | Normal | Normal | Low |
| Free protein S (%)a | 74 (67–136) | 54 (65–140) | 64 (64–154) | Normal | Normal | Normal |
| Factor IX (%)a | 94.0 (44–127) | 114.0 (64–216) | 88.0 (48–145) | Normal | Normal | Low |
| Factor XI (%)a | 72.0 (60–140) | 58.0 (60–140) | 86.0 (60–140) | Normal | Normal | Low |
| INRa | 1.27 (0.92–1.14) | 1.31 (0.97–1.30) | 1.25 (0.87–1.20) | Normal | Normal | Low |
| PT (%)a | 60.0(>70) | 56.0(>70) | 61.0 (>70) | Normal | Normal | Normal |
| Thyroid function | Normal | Normal | Normal | High TSH, low freeT4 | Normal | Normal |
| FSH (U/L)a | 34.7 (0.5–4.5) | N/A | 18.1 (0.5–4.5) | High FSH | Normal | N/A |
| LH (U/L)a | 2.75 (<0.45) | N/A | 0.54 (<3.36) | High LH | Normal | N/A |
- N/A, no answer.
- a In parentheses age dependent/normal limits.
- b Wechsler intelligence scale for children: A, average; LA, low average; B, borderline; EL, extremely low.
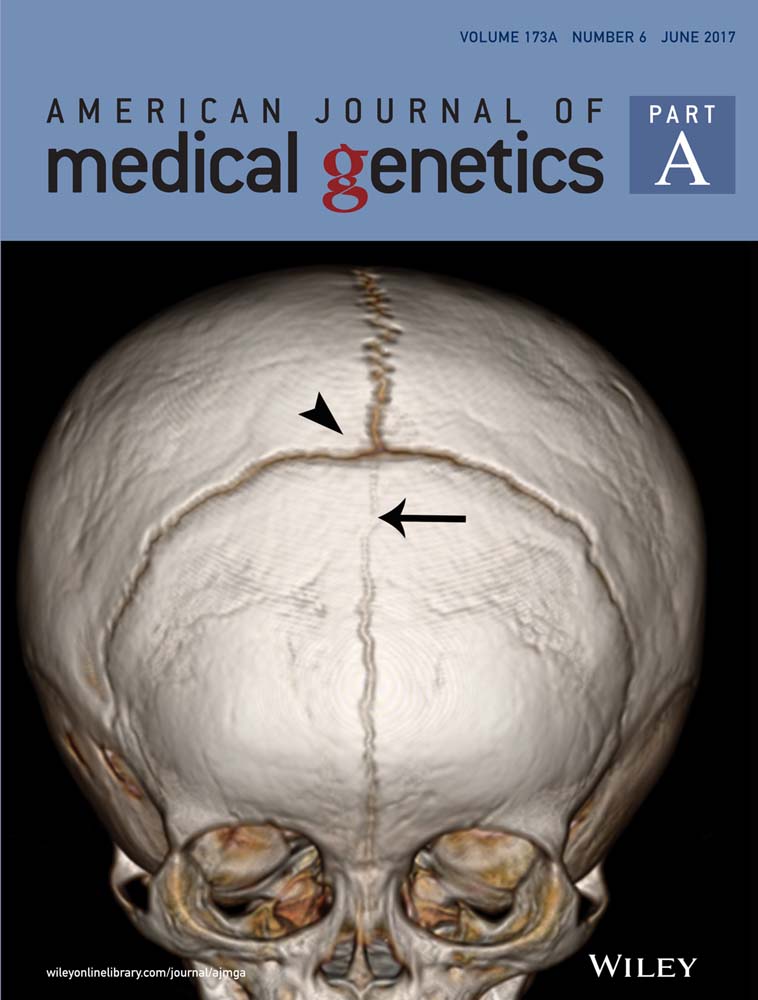
Two older siblings (proband A2 and A3 in Table 1) also had problems with gross motor development, and ataxia in infancy and early childhood. A2 started to walk at 19 months of age and his speech development was delayed, whereas A3 started to walk at 21 months of age, but had no problems with speech development. Brain MRI of probands A2 and A3 showed non-progressive cerebellar hypoplasia.
All sibs have needed orthodontic treatment, since they continued to have an infantile swallowing pattern characterized by tongue thrusting, which caused occlusion abnormalities. All probands showed some coagulation abnormalities, and females need to be followed for the risk of developing hypergonadotropic hypogonadism (details in Table 1).
According to the Wechsler Intelligence Scale for Children (WISC), the full scale IQ scores were 72 and 81 for probands A2 and A3, at the ages of 16 and 8, respectively. Proband A3 compensated for his borderline IQ with good working memory (index 97). Both older sibs presently study in normal school.
2.2 Family B
In family B (Table 1), both children were born to non-consanguineous parents at term after an uneventful pregnancy. PMM2-CDG was first diagnosed in the oldest sibling (B1) at the age of 10 years, when she presented with mildly delayed motor skills and hypothyroidism. She started to walk at the age of 20 months. At the age of 16 years she was evaluated for delayed puberty. She attended normal education and finished secondary school. She was diagnosed with anxiety and autistic features, although her communication skills were normal. Her older brother (B2) had a similar mild motor developmental delay as well as strabismus. He had delayed speech development and mild dysarthria. He attended special education for his speech impediment, which normalized at the age of 14 years. There were no coagulation abnormalities or abnormal liver function tests in patients in family B.
WISC showed that proband B1 has full scale IQ score of 93 and proband B2 an IQ score of 72.
2.3 Family C
In family C (Table 1), the patient C1 was born at term to non-consanguineous parents after an uneventful pregnancy. PMM2-CDG was diagnosed at the age of 1 year due to delayed motor skills and ataxia, strabismus and failure to thrive. The patient started to walk at the age of 5 years. She also had dysarthria, but used sentences from the age of two years. A brain MRI showed cerebellar and vermis hypoplasia. There were mild coagulation abnormalities, but no endocrine dysfunction or abnormalities of liver function. She is attending normal education and finished primary school. WISC showed an IQ score of 89.
3 METHODS AND RESULTS
All probands from families A, B, and C showed a clear type 1 pattern on serum transferrin isoelectric focusing.
All mutations in PMM2 are named according to the Human Genome Variation Society nomenclature guidelines using NM_000303.2 as the reference sequence. The first reports of the mutations identified in our patients are cited.
In patient A1, next generation sequencing of a large gene panel (TruSight One, Illumina Inc., San Diego, CA) revealed compound heterozygosity for two previously reported mutations in exon 8: c.691G>A (p.Val231Met) and c.715A>T (p.Arg239Trp) (Grunewald et al., 2001; Matthijs et al., 1997). Sanger sequencing confirmed PMM2 mutations in sibs A1, A2, A3, and their parents.
Direct Sanger sequencing of PMM2 identified the mutations c.722G>C (p.Cys241Ser) and the common c.422G>A (p.Arg141His) (Matthijs et al., 1997; Matthijs, Schollen, Heykants, & Grunewald, 1999) in family B, and c.359T>C (p.Ile120Thr), c.682G>T (p.Gly228Cys) (Matthijs et al., 2000, 1999) in Family C.
Enzymatic analysis of PMM showed a residual activity of PMM in skin fibroblasts 1.6 mU/mg protein (normal limits 4.7–9.2) in A2 and 2.8 mU/mg protein (normal limits 6.7–11.2) in B1. PMM activity was not measured in patient C1.
This study was approved by the Research Ethics Committee of the University of Tartu.
4 DISCUSSION
PMM2-CDG is the most common subtype among the growing number of different CDG. The severity of PMM2-CDG is variable. Patients usually present a recognizable phenotype with neurological/multisystem symptoms that might cause an early death. Still, patients with subtle neurological symptoms (often hypotonia and ataxia) who have mild-to moderate ID or IQ within normal limits have also been described (Giurgea, Michel, Le Merrer, Seta, & de Lonlay, 2005; Mader, Dobler-Neumann, Kuker, Stibler, & Krageloh-Mann, 2002; Vermeer et al., 2007). In our report, WISC was performed for five patients, all of whom showed normal cognitive development with full scale IQ ranging from borderline to average (score 72–93).
As in other patients with mild PMM2-CDG, delayed gross motor skills were common among the patients described in this study. Cerebellar hypoplasia was present in all patients in whom brain MRI was performed. Central nervous system involvement and cerebellar hypoplasia are characteristic even in mild PMM2-CDG (Barone et al., 2015; Grunewald et al., 2001; Scott, Gadomski, Kozicz, & Morava, 2014). Thus our patients’ clinical symptoms are on the milder end of PMM2-CDG phenotypic spectrum as was described by Grunewald et al. (2001).
We did not see any difference on serum transferrin isoelectric focusing between severe and mild PMM2-CDG patients, as all six patients showed a clear type 1 pattern despite their mild phenotype and age at the time of diagnosis.
Genotype-phenotype correlation studies in PMM2-CDG patients (Barone et al., 2015; Grunewald et al., 2001) have been published. Some mutations (e.g., H218L, L32R, C241S, T237M) cause a milder phenotype; however, the severity might also depend on the combination of particular mutations (Barone et al., 2015; Matthijs et al., 1999). In this paper, all reported families had different compound heterozygous mutations. Siblings from family A shared the genotype p.Val231Met/p.Arg239Trp. p.Val231Met is rather frequently found among patients with PMM2-CDG, and its usual combination with the most common mutation, p.Arg141His, has been shown to cause a severe clinical picture (Barone et al., 2015; Grunewald et al., 2001; Matthijs et al., 2000, 1997). p.Arg239Trp has been described only once in combination with p.Phe157Ser, in which case the patients had either a mild-moderate or a moderate phenotype (Grunewald et al., 2001).
Siblings from family B with a common combination of mutations p.Cys241Ser and p.Arg141His support the genotype-phenotype correlation described in other papers, as this genotype has been reported to cause a mild clinical expression (Barone et al., 2015; Giurgea et al., 2005; Grunewald et al., 2001). Sibling C1 had mutations p.Ile120Thr/p.Gly228Cys. p.Gly228Cys has been described in combination with p. Arg141His in a 4-year-old patient with similar neurological findings and good developmental progress, but also with a cerebral hemorrhage (Stefanits, Konstantopoulou, Kuess, Milenkovic, & Matula, 2014).
To our knowledge, patients with the genotypes p.Val231Met/p.Arg239Trp and p.Ile120Thr/p.Gly228Cys have not yet been reported, but it seems likely that these genotypes might cause a milder PMM2-CDG. Our reported patients may give useful insight into the course and the prognosis of PMM2-CDG for other patients with the same genotype.
There is no official management protocol for PMM2-CDG, and the treatment remains supportive and symptomatic. Reviews about hypothyroidism and thrombotic events due to coagulopathy among PMM2-CDG patients have been published, which give suggestions about the management of these conditions (Linssen, Mohamed, Wevers, Lefeber, & Morava, 2013; Mohamed et al., 2012). All our described patients are under regular follow-up and treated when needed.
We present six patients from three families, who are diagnosed with clinically mild PMM2-CDG and normal cognitive development. Four out of our six patients were diagnosed with PMM2-CDG at the age of 8 years or later, as their clinical course and neurological symptoms were quite mild and non-progressive, and they were able to participate in regular school programs. This suggests that some of the mild cases of PMM2-CDG might be missed, leading to underdiagnosis of PMM2-CDG. Hence, we encourage screening for CDG among patients with a subtle neurological syndrome and normal cognitive development.
ACKNOWLEDGMENTS
We thank the families for their cooperation. This work was supported by the Estonian Research Council grant PUT355 and The National Institute of General Medical Sciences of the National Institutes of Health (1 U54 GM104940), which funds the Louisiana Clinical and Translational Science Center.
CONFLICTS OF INTEREST
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.