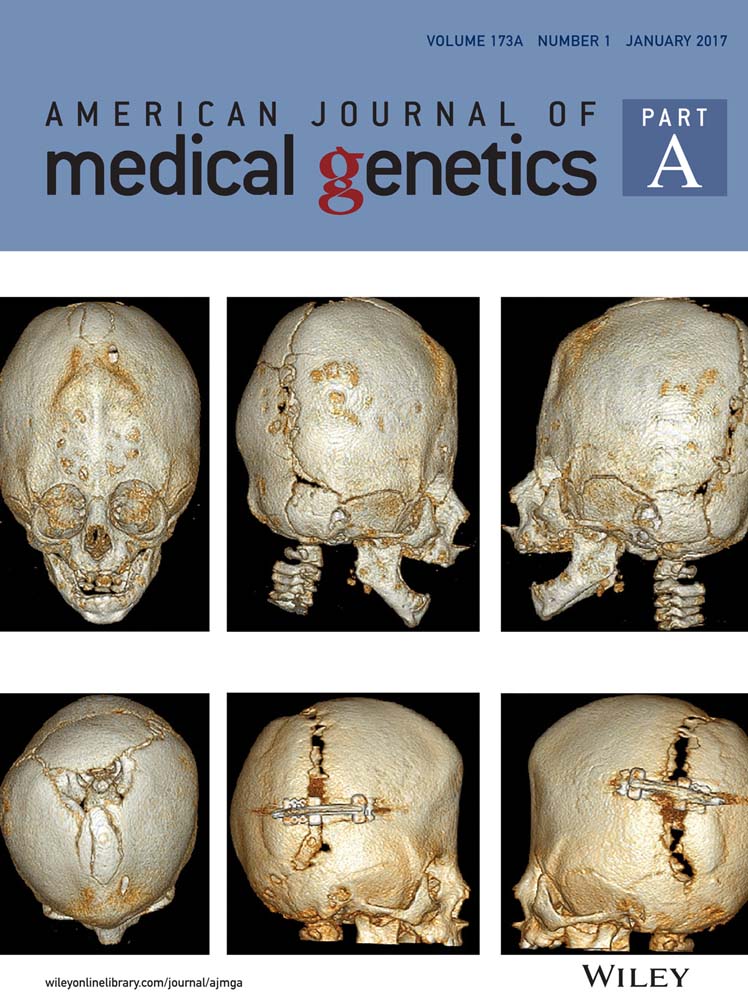
Spondyloepiphyseal dysplasia Omani type: CHST3 mutation spectrum and phenotypes in three Indian families
Abstract
We describe three consanguineous Indian families with a distinct form of spondyloepiphyseal dysplasia (SED Omani type). It is an autosomal recessive disorder due to mutation in CHST3 gene. CHST3 gene encodes the enzyme chondroitin 6-O-sulfotransferase-1 (C6ST-1) which mediates the sulfation of proteoglycans, (chondroitin sulfate), in the extracellular matrix of cartilage. CHST3 gene was sequenced in probands from three different families with SED. In two families missense mutations (c.904G>C predicting the substitution D302H) and c.491C>T (P164L) were identified. A frameshift (insertion) mutation (c.533_534ins G predicting the substitution A179Rfs*) was found in the third family. SNP micrarray in the family 2 helped to localize the common areas of homozygosity and identified the candidate gene. The confirmation by molecular diagnosis will be useful in the management and in the counseling of affected patients and their families. The presence of sclerosis of cranial sutures adds to the phenotypic spectrum of the disorder. Severe cardiac valvular disease in a case and triangular epiphyses of knees are other features which are highlighted in this report. © 2016 Wiley Periodicals, Inc.
INTRODUCTION
Understanding of molecular etiologies has helped to classify skeletal dysplasias in a better fashion. Spondyloepiphyseal dysplasia (SED) with joint laxity and CHST3-related spondyloepiphyseal dysplasia have joint dislocations, the feature showing overlap with Larsen syndrome. Due to presence of congenital joint dislocations, some of the cases had been labelled as Larsen syndrome or were described under a different name as humerospinal dysostosis. This type of SED presenting as short stature, prominent joints, camptodactyly, and joint dislocations was described in a large Omani kindred in 2004 [Rajab et al., 2004; Thiele et al., 2004]. No firm data regarding the prevalence of CHST3-related skeletal dysplasia are available. More than 30 cases (including familial recurrences) with homozygous mutations have been reported. We identified CHST3 mutations in three unrelated Indian patients. This adds to the mutational as well as phenotypic spectrum of the disorder. Because of consanguinity, we performed SNP array in one case and confirmed CHST3 gene as candidate gene and this helped to rule out the possibility of other syndromes with joint laxity.
CLINICAL REPORT
Patient 1
A 5-year-old male child presented to medical genetics outpatient department with chief complaints of short stature dislocations of right hip joint and both knee joints at birth and right talipo equinovarus. He was a product of third degree consanguineous parentage and born at term. His birth weight was 3.5 kg. Developmental milestones were normal till 7–8 months of age. However, standing and walking was delayed because of joint problems. His cognition was appropriate for age and had apparently normal hearing and vision. After multiple joint surgeries, he could stand and walk. He had broad and prominent forehead, small, and low set ears (Fig. 1). Terminal extension at elbow joints was restricted. There was no distal joint laxity. He has kyphosis and pectus excavatum. Right foot was medially deviated with spatualate great toes. Thumbs were proximally placed and spatulate. Head circumference was 52 cm (+1 SD), height was 92 cm (−3 SD), upper segment to lower segment ratio was 1.12:1, and arm span was 92 cm. Clinically the cardiac evaluation was normal but echocardiography was not done.

Radiographs showed that the right hip joint was dislocated and heads of femora were small and flattened. Femoral necks were short. Left femur showed coxa vara. There was bony overgrowth at the tendon attachment on the iliac bone near left superior iliac spine. Distal epiphyses of femora were asymmetric with triangular shape and loss of intercondylar notch. Patellae were hypoplastic and laterally deviated. Bone age was delayed and only three carpals were present. Both elbows were dislocated. Thoracolumbar spine showed irregularity of vertebral margins, mild platyspondyly, decreased intervertebral spaces. Also the antereoposterior radiograph of thoracolumbar spine showed the widening of the interpedicular distance from T12 to L1 with narrowing of this distance further down in the lumbar vertebrae which is characteristic of SED Omani type. Mild sclerosis around skull sutures was noticed.
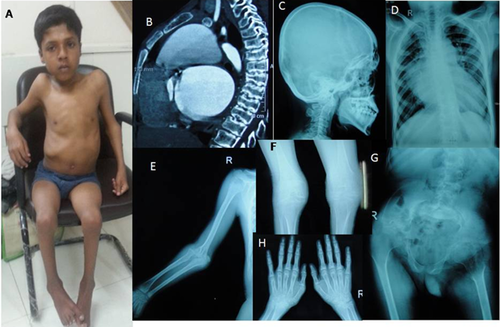
Patient 2
A 15-year-old boy born to consanguineous parents was brought to the medical genetics outpatient department with the complaint of pain in both hip- and knee joints leading to progressive worsening difficulty in standing and walking for last 6 months. Six months ago the patient was ambulatory to such an extent that he used to ride a bicycle on his own and attend school. But at the time of examination, he could not stand and was wheel chair bound. He was also having short stature which was noticed since infancy. Heart disease was also diagnosed during infancy. Development milestones were attained on time. The intelligence was age appropriate. He was sixth in birth order, other five sibs, two brothers, and three sisters are healthy with no similar complaint. His weight was 20 Kg (<3rd centile for 15 years). Head circumference was 51.5 cm (−2 SD for 15 years), height (could not be measured properly) was 114 cm (−6 SD for 15 years), upper segment to lower segment ratio was 1.03:1.
He did not have facial dysmorphism. There was pectus carinatum, restriction of movements of shoulders, elbows, knees, and hip joints (Fig. 2). Elbows and wrists were broad and enlarged. Fingers were normal. He had lordosis and scoliosis. He had cardiomegaly and echocardiogram showed severe mitral regurgitation, pulmonary stenosis, aortic stenosis, and aortic regurgitation. Radiographs showed markedly deformed pelvis with disorganized and dislocated hip joints. Elbows were dislocated and show metaphyseal widening. Wrists showed small irregular carpal bones and almost no joint spaces. Metaphyses of radius and ulna were widened. Epiphyses of metacarpals were flattened. The knees also showed reduced joint spaces, prominent intercondylar notch, and squared condyles rather than the normal rounded shapes. There was sclerosis around skull sutures. Spine showed accentuated spinal curvatures and scoliosis. CT scan of spine was more informative than the radiographs. There was platyspondyly in thoracic region only and vertebral margins were irregular and sclerosed with reduced joint spaces. The widening interpedencular distance was not obvious probably due to scoliosis. On follow up, the family informed that he died probably due to cardiac problems. Due to scoliosis interpedicular distance abnormality was not obvious and SNP microarray was done to select a candidate gene for the phenotype with multiple joint dislocations and arthropathy with cardiac involvement.
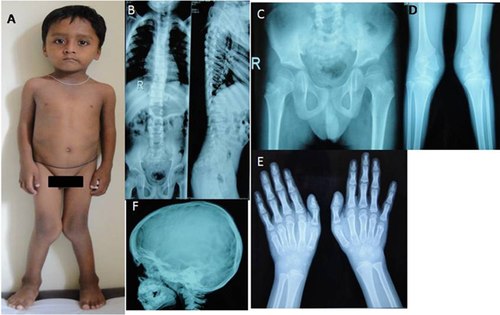
Patient 3
A 5-year-old boy presented with complaints of not gaining height since 6–7 months of age. The child was markedly short as compared to the peer group. There is also history of progressively increasing contractures with joint deformities noticed since 6–7 months of age. It involved knees, ankles, hands, and elbows. He was born to consanguineous parents at 37 weeks of gestation. Antenatal period and neonatal period were uneventful. There has been normal attainment of development milestones. Intellect is normal. His height was 88.5 cms (−4 SD) with upper segment to lower segment ratio of 1.1. His weight and head circumfenerce were 12 kgs (−2.5 SD) and 49.5 cms (30th centile), respectively. Face was normal. He had genu vulgam and lumbar lordosis (Fig. 3). All joints were prominent. Joint contractures were present at elbows, knees, wrists. The movements were restricted at ankles and hips as well. Mobile calcaneo-valgus was present. Both hands had Simian creases. There was no brachydactyly or camptodactyly. There was lumbar lordosis and sacral dimple. Radiographs of spine showed platyspondyly, irregularity and sclerosis of vertebral ends, and characteristic widening of interpendencular distance upto second lumber vertebrae. Pelvis was wide and epiphyses of head of femur were small and left hip joint was dysplastic with vertical acetabular roof and sclerosis of acetabular margins. Skull radiograph showed sclerosis around sutures. Femur necks were short and there was sclerosis of lesser trochanter. Shape of carpals was normal but bone age was 4.5 years. Elbows were dislocated. Femoral epiphyses at knees showed deep intercondylar notch with large and triangular condyles. Distal epiphyses of metacarpals were flattned. There was no clinical evidence of cardiac disease but echocardiographic evaluation was not done. Due to characteristic presentations the clinical diagnosis of SED Omani type was made and CHST3 gene was sequenced.
MATERIALS AND METHODS
Informed consents were obtained from the parents of the patient for the molecular genetic analysis of the patients. Blood samples from both affected and unaffected individuals of the family were collected in EDTA containing vacutainer sets. Genomic DNA from the blood samples was extracted using QIAamp DNA Blood extraction kit.
SNP Microarray
We genotyped DNA using Gene Chip Human Mapping NspI HD array (Affymetrix, Santa Clara, CA), as per the manufacturer's recommendations. The homozygous areas were identified by selecting the Loss of Heterozygosity (LOH) regions with a minimum cut off value of 5 MB. Genomic Oligoarray and SNP array evaluation tool, a software programme described elsewhere has been used to search the candidate gene by putting specific clinical features [Wierenga et al., 2013].
Sequencing Analysis
The two coding exons of CHST3 were amplified by PCR and cycle sequenced using the ABI Prism BigDye Terminator Cycle Sequencing Ready Reaction Kit Version 1.1 (Applied Biosystems, Darmstadt, Germany). Capillary electrophoresis was performed using an ABI 310 sequencer (Applied Biosystems, Foster City, CA).
RESULTS
SNP microarray was done for patient 2. On analyzing genes situated in these LOH regions, we found CHST3 gene related to the joint abnormalities. Sequencing of CHST3 gene identified two different novel missense mutations in homozygous state (c.904G>C predicting the substitution D302H in patient 1 (Supplementary Fig. S1A) and c.491C>T (P164L) in patient 2 (Supplementary Fig. S1B). One HGMD (Human Genome Mutation Database) reported insertion was identified in patient 3 (c.533_534 InsG) which leads to frameshift mutation (p.A179R fs* 141) (Supplementary Fig. S1C). Parents were found to be carriers for the mutations. c.904G>C and c.491C>T were novel mutations, not reported in 1000 genomes, HGMD, and HGV (Human Genome Variation).
DISCUSSION
Here, we present three Indian patients with mutation proved cases of SED Omani type. All of them were from consanguineous families. Patients 1 and 3 had characteristics changes in the radiographs of the thoraco lumbar spine in the form of the widening of the interpedicular distance from T12 to L1/L2 with narrowing of this distance further down in the lumbar vertebrae. The characteristic radiographic changes can provide the clinical diagnosis. In the case 2, because of deformed spine and pelvis an appropriate view of the spine to demonstrate increasing interpedicular distance in lumbar spine was not obtained and hence case 2 was subjected to SNP microarray to identity the candidate gene and differentiate from other recessive disorders with joint dislocations. Presence of normal face distinguishes this disorder from Larsen syndrome which is a common cause of congenital joint dislocations.
SED Omani type was mapped to chromosome 10q23, and subsequently, missense mutations (P164L, D302H) were identified in CHST3 gene. CHST3 codes for C6ST-1, an enzyme involved in the transfer of sulfate specifically to position six of the GalNAc in chondroitin sulfate. All the three mutations identified in our cases, namely; homozygous missense mutation c.904G>C (D302H) and c.491C>T (P164L) and one frameshift insertion mutation (c.533_534ins G predicting the substitution A179Rfs*) are localized in the highly conserved PAPS-binding site, the 3′-phospho-binding (3′-PB) motif, which is known to be essential for the transfer of sulfate. Eighty percent of the mutations reported so far that are located within the highly conserved PAPS binding site. van Roij et al. [2008] found a missense mutation (857T>C predicting the substitution L286P) in CHTS3 in two Turkish siblings with a severe skeletal dysplasia resembling SED Omani type. In addition to characteristic features of congenital dislocations, platyspondyly and decrease in the interpeduncular distance in lumbar vertebrae, these two siblings has ventricular septal defect (VSD), deafness, metacarpal shortening, and accessory carpal ossification centers, adding new clinical features to the condition. CHST3 mutations have also been described in a subset of patients with initially labelled as recessive Larsen syndrome and humero-spinal dysostosis [Hermanns et al., 2008]. The reported mutations consist of four frameshift and four missense mutations. The latter are all located within the sulfotransferase domain of C6ST-1 and are predicted to interfere with the normal function of the protein.
The phenotypic descriptions are limited. Unger et al. [2010] have described phenotypes of 24 cases of mutation proved cases including some cases from India. Joint dislocations with spinal involvement are characteristic. The commonest joints involved are knees followed by elbows and hips. Clubfeet was seen as the list common of the joints involved. All affected individuals possess the characteristic vertebral anomalies of platyspondyly, end plate irregularities, and increasing interpedicular distance from T12 to L1/L2. However, this was not appreciable in one of our cases due to abnormality of spinal curvature. In the case series of 24 cases, nine had kyphosis and five had scoliosis [Unger et al., 2010]. Epiphyseal involvement is seen in the form of small epiphyses. The epiphyses of knees in all three cases in this report are grossly abnormal in shape and do not appear to be small. The epiphyses of lower ends of femora were asymmetric and pointed in case one and triangular with deep intercondylar notch in case 3. Case 2 also lad pointed square shaped epiphysis of lower ends of femora and the notch was prominent. Similar changes are described in a case by Unger et al. [2010] and have attributed them to abnormalities of weight bearing. However, most of the radiographs of the children with SED Omani type are of ages around 2–3 years. Epiphyses of metacarpals in our cases were large and square. There was some degree of sclerosis around cranial sutures in all cases. There is limited data about cardiac involvement as all cases were not clinically evaluated. Two original cases reported by Kozlowaski et al. [1974] and 5 of 24 cases of the only series [Unger et al., 2010] had evidence of cardiac valvular involvement with thickening and dysplasia. In case 2 of our report, there was severe cardiac valvular disease noted since infancy and probably the cause of early death. The patient had marked cardiomegaly, severe mitral regurgitation, pulmonary stenosis, aortic stenosis, and aortic regurgitation. Cardiac involvement has also been reported by Tuysuz et al. [2009]. In view of cardiac involvement in some patients with SED Omani type, we believe that there is a need for cardiac evaluation and close follow up during surveillance of such patients. In addition to vertebral changes and joint dislocations, sclerosis around cranial sutures may be the characteristic features unreported till date. Abnormalities of epiphyses of lower ends of knees especially in older children also may be a diagnostic clue. Though, we do not have close and long-term follow up of these cases, the severity of joint involvement appears to vary greatly from case to case. Case 2 was mobile till second decade, while case 1 needed multiple surgeries during childhood. The accurate diagnosis of this rare variety of SED presenting as joint dislocations is important as being inherited in autosomal recessive fashion the risk of recurrence is 25% as against most common varieties of Larsen syndrome which are dominantly inherited. The possibility of severe cardiac problems stresses the need for cardiac evaluation in all cases. The disorder though reported as a rare disorder, may be not uncommon especially in populations with high prevalence of consanguinity.
ACKNOWLEDGMENTS
We sincerely thank the cooperation of patient families and acknowledge Indian Council of Medical Research, New Delhi for funding (BMS-63/8/2010).