Osteogenesis imperfecta type V: Clinical and radiographic manifestations in mutation confirmed patients
Abstract
Osteogenesis imperfecta (OI) type V is a specific OI phenotype with interosseous membrane calcification of the forearm and hyperplastic callus formation as typical features. The causative gene mutation for OI type V has been recently discovered. The purpose of this report is to review the clinical and radiographic characteristics of mutation confirmed OI type V in detail. Sixteen (nine familial and seven sporadic) patients were enrolled in the study. Blue sclera and dentinogenesis imperfecta were not evident in any patient. However, hypodontia in the permanent teeth, ectopic eruption, and short roots in molars were additionally observed in 11 patients. Of the radiographic abnormalities, cortical thickening and bony excrescence of interosseous margin of the ulna was the most common finding, followed by overgrowth of the olecranon and/or coronoid process of the ulna. Slender ribs and sloping of the posterior ribs with or without fractures were also a consistent finding. Hyperplastic callus was detected in 75% of patients and was commonly encountered at the femur. Heterotopic ossification in the muscles and tendon insertion sites were noted in four patients, which resulted in bony ankylosis or contracture of joints. The current study confirms common clinical and radiographic findings of OI type V and reports additional phenotypic information. These observations provide clues to recognize OI type V more promptly and guide to direct targeted molecular study. © 2013 Wiley Periodicals, Inc.
INTRODUCTION
Osteogenesis imperfecta (OI) is a heterogeneous group of genetic disorders characterized by fragile bones with multiple fractures and ensuing skeletal deformities. The majority of OI cases are caused by heterozygous mutation of either COL1A1 or COL1A2 encoding the α1 or α2 chains of type 1 collagen, respectively, and are inherited in an autosomal dominant pattern [Roughley et al., 2003; Rauch and Glorieux, 2004]. Some OI cases were found to be autosomal recessive, and six more genes responsible for these recessive OI have been discovered [Rohrbach and Giunta, 2012]. However, the proposed classification of OI into types I–IV [Sillence et al., 1979] remains the mainstay of the clinical classification system. Glorieux et al. [2000] proposed a new type of autosomal dominant OI similar to type IV, but with specific clinical, radiological, and/or histological features including limitations in the range of pronation/supination in forearms with apparent calcification of the interosseous membrane, anterior dislocation of the radial heads, radiodense metapyseal bands, a definite histomorphology with a mesh-like pattern of lamellation in bone biopsy, and absence of pathogenic mutation in COL1A1 or COL1A2. Thus, these patients were distinguished from type IV and categorized as OI type V.
The causative gene and its specific pathogenic mutation responsible for OI type V have been recently discovered. The heterozygous mutation c.-14C > T in the 5′-untranslated region (UTR) of a gene encoding interferon-induced transmembrane protein 5 (IFITM5) was consistently identified in all reported patients [Cho et al., 2012; Semler et al., 2012; Rauch et al., 2013].
The objective of the present study was to review the characteristics of the clinical and radiographic features in OI type V. Although a limited set of series and a few case reports have described this type [Fleming et al., 2005; Vieira et al., 2006; Cheung et al., 2007, 2008], no attempt has been made to stress the radiographic variability in a group of mutation confirmed patients. Thus, we provide phenotypic information on OI type V in more detail.
MATERIALS AND METHODS
The study design was approved by the institutional review board of the participating institutions. This study comprised 16 patients (14 Korean and 2 Japanese) with full skeletal survey available and all were confirmed to have the IFITM5 mutation, c.-14C > T in the 5′-UTR. Nine cases were familial (from four families) and seven cases were sporadic. Of these, brief clinical and limited radiographic findings were described previously [Lee et al., 2006; Cho et al., 2012]. Clinical information regarding number of fractures, disability of the bone and joints, mobility in daily life, color of sclera, and hearing deficit were obtained from the medical records. Measured height was transformed to age and sex-matched z-scores using standard growth chart and data from anthropometric survey of ethnic origins.
All radiographs at the time of first visit were assessed. Follow-up radiographs were available for 13 patients and the length of the follow-up ranged from 16 months to 10 years. Baseline radiographic criteria of OI type V including calcified interosseous membrane, radial head dislocation, dense metaphyseal bands, and hyperplastic callus were assessed. In addition, radiographic abnormal bone shape of the forearm and elbow joint were compared with age-matched normal elbow. Radiographs of the skull, chest, spine, and lower extremity were reviewed and overall percentage of frequency in radiographic abnormalities was estimated. Panoramic radiographs of the jaw were reviewed, which were taken to investigate pulpal pathology related to dentinogenesis imperfecta such as pulpal obliteration and pulp stones. Computed tomography (CT) scan of the forearm was performed in six patients and reviewed focusing on the relation between interosseous membrane and the shafts of the radius and ulna.
RESULTS
Demographic data and clinical findings are summarized in Table I. The first fracture episode experienced at <1 year of age was noted in six patients and the earliest age of the first fracture was at 2 months. Most patients recorded as having 5–10 fractures at the time of study; however, four patients had more than 15 fractures. Height z-scores ranged between −3.84 and 1.88 (median −1.35). None of the patients presented blue sclera. None of the patients had dentinogenesis imperfecta; however, scrutiny of dental examinations revealed congenital dental anomalies such as single or multiple premolar missing in eight patients, ectopic eruption of the molar in two, and short roots of the molar in two. Hearing deficit was recognized in one patient (patient 16) who had sensorineural hearing loss. The range of forearm motion in pronation/supination was limited in all patients. Flexion and extension of the elbow joint was limited in four patients. As to mobility, one patient required a wheel chair due to generalized painful and limited motion. The remaining patients had no ambulatory limitation in daily motility but were limited in ability to run and walked with the assistance of a cane.
| Patient | Gender | Age at first X-raya | Age at last follow-up (years) | Height (z-score) | Familial/sporadic | No. of fractures | Mobility in daily lifeb | Dental examination |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 9 months | 8 | 0.8 | Family 1 | ∼5 | Not limited | Maxillary premolar congenital missing |
| 2 | M | 4 years 3 months | 11 | 1.88 | Family 1 | ∼10 | Limited running | No abnormality |
| 3 | F | 7 months | 6 | 0.02 | Family 2 | ∼20 | Limited ambulation | Premolar congenital missing |
| 4 | F | 10 years | 20 | −2.43 | Family 3 | 15 | Not limited | Mandibular premolar congenital missing |
| 5 | M | — | 29 | −0.44 | Family 4 | 20 ∼ 30 | Limited ambulation (walk with a cane) | Mandibular premolar congenital missing premolar impaction |
| 6 | M | 45 years | 52 | −0.94 | Family 1 | 4 | Not limited | Malocculusion |
| 7 | F | — | 27 | −2.05 | Family 2 | ∼30 | Not limited | No abnormality |
| 8 | M | 40 years | 50 | −3.21 | Family 3 | 7 ∼ 9 | Limited ambulation (walk with a cane) | No abnormality |
| 9 | F | — | 53 | −2.6 | Family 4 | ∼10 | Not limited | No abnormality |
| 10 | F | 8 months | 2 | −1.76 | Sporadic | 8 | Start independent ambulation | No abnormality |
| 11 | F | 2 months | 4 | 0.03 | Sporadic | ∼10 | Not limited | Multiple teeth congenital missing |
| 12 | M | 4 months | 7 | −2.52 | Sporadic | ∼5 | Not limited | Molars ectopic eruption |
| 13 | F | 11 months | 9 | -1.96 | Sporadic | ∼20 | Not limited | Molar ectopic eruption short roots in molars |
| 14 | M | 2 years 6 months | 15 | −0.89 | Sporadic | ∼10 | Limited running | Premolar congenital missing |
| 15 | M | 7 years | 14 | −0.77 | Sporadic | ∼10 | Wheel chair bound | Multiple teeth congenital missing short roots in molars |
| 16 | M | 5 years 6 months | 16 | −3.84 | Sporadic | ∼10 | Limited running | Premolar congenital missing |
- a Age at first X-ray means the earliest radiographs available.
- b Mobility limitation was estimated around age at last follow-up.
Skeletal abnormalities were observed; their frequencies are summarized in Table II. Of the known diagnostic radiographic criteria, discernible interosseous membrane calcification of the forearm was not evident before 10 years of age. Instead, focal cortical thickening and/or bony excrescence was evident initially (Fig. 1). Thus, we described this finding as cortical thickening or bony excrescence of interosseous margin on radius/ulna diaphyses, rather than simply interosseous membrane calcification. CT scan in six patients showed bony excrescences that were continuous with the cortices of radius/ulna interosseous margin (Fig. 2). In two adults and one adolescent patient, there was obliteration of the radius/ulna interosseous space by bony bridge (Fig. 3). Tibia and fibula interosseous calcification was detected in six patients (Fig. 4).
| Radiographic findingsa | Frequency of findings (%) |
|---|---|
| Skull | |
| Wormian bone | 15/16 (94) |
| Chest | |
| Thin ribs | 14/16 (87) |
| Acute sloping of posterior ribs | 14/16 (87) |
| Elbow/forearm | |
| Interosseous membrane calcificationb | 16/16 (100) |
| Large olecranon/coronoid process | 15/16 (94) |
| Radial head hypoplasia | 5/16 (31) |
| Radial head dislocation | 13/16 (81) |
| Large radial head/tuberosity | 6/16 (37) |
| Radioulna bowing | 16/16 (100) |
| Extremity | |
| Metaphyseal sclerotic band | 9/16 (56) |
| Hyperplastic callus | 12/16 (75) |
| Interosseous calcification of tibia/fibula | 6/16 (37) |
| Tibiofibula bowing | 14/16 (87) |
| Spine | |
| Compression fracture | 14/16 (87) |
| Scoliosis | 9/16 (56) |
| Heterotopic ossificationc | 4/16 (25) |
- a Evaluated at the last X-ray.
- b Including cortical thickening/excrescence of interosseous margin on the radius-ulna diaphyses.
- c Heterotopic ossification seen in the muscle and tendon attachment site.
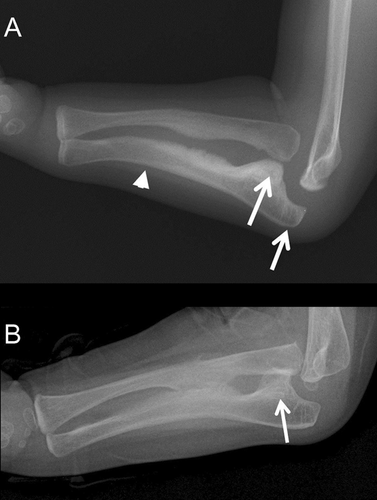



Of the newly recognized dysmorphic signs of the forearm, overgrowth of the olecranon and/or coronoid process of the ulna was the earliest abnormality and was evident in 15 patients (94%; Fig. 1). Anterior dislocation of the radial head was seen in 13 (81%) patients, which appeared as early as 11 months of age. Ulna bowing was consistently seen in all patients and in some was accompanied by extent radial bowing.
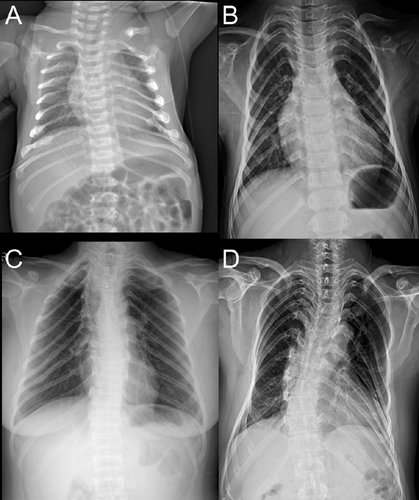
Slender ribs with or without rib fractures and sloping of the posterior ribs, which resulted in the pyramidal shape of the thorax, were seen in 14 patients (87%; Fig. 5). Metaphyseal sclerotic bands tended to be age-related, with younger patients presenting denser bands (Fig. 1). This band was evident at the knees and wrists. It became thin and less distinct with age on follow-up images.
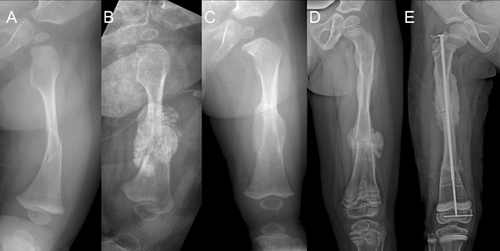
Hyperplastic callus (HC) of the extremities was noted in 12 (75%) patients, with the femur being the most prevalent site for HC formation (Fig. 6). The evolution of HC was variable, but there was regression of size within a month in the majority of patients. Complete resolution of HC was not noted in all affected patients, and remained for years as calcified protuberances merging with or without adjacent cortices.
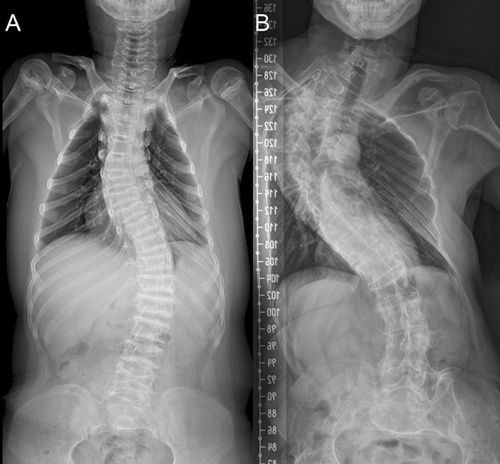
Wormian bones of the skull and compression fractures in the spine are common findings in OI, regardless of type. In the present study, 15(94%) patients showed wormian bones in the lambdoidal sutures. Spinal compression fractures identified by either radiographs or medical records were noted in 14 (87%) patients. Scoliosis was detected in half of the study cohort. There was a tendency of progressive severity of curvature with increasing age (Fig. 7).
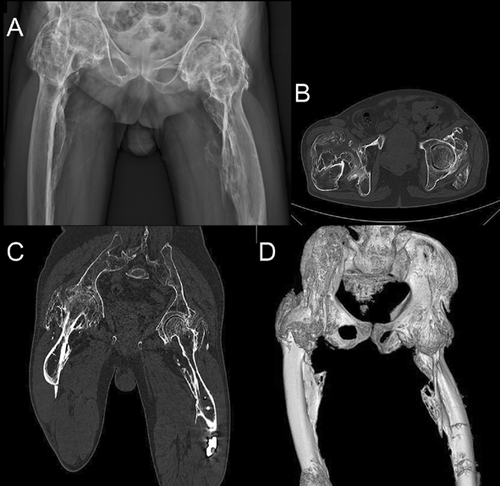
A unique finding recognized in four patients was the heterotopic ossification at the femur shaft, acetabulum, and iliac crest, similar to those seen in patients with myositis ossificans or fibrodysplasia ossificans progressiva (Fig. 8). CT scan confirmed the heterotopic ossifications in the muscles and tendons attached to the pelvic bone and femur.
DISCUSSION
Aside from general characteristics of OI such as bone fragility, frequent fractures, spine and limb deformities, the clinical manifestations specific to OI type V such as HC, limitation of forearm rotation, absence of blue sclera and dentinogenesis imperfecta were consistently observed in this study. In most cases, clinical and radiological diagnosis of OI type V becomes conspicuous before school age. However, in very young children in whom the characteristic clinical and radiographic manifestations have not yet presented, one should pay attention to subtle radiographic changes.
A novel finding of the current study was high incidence of dental anomalies including congenital missing in the permanent dentition, ectopic eruption, and short roots of the molar teeth. It is not yet known whether IFITM5 plays a role in the tooth development. However, considering the prevalence of hypodontia in general population, ranging from 2.6% to 11.3% [Larmour et al., 2005], the dental anomalies observed in our cohort might be a part of OI type V phenotype. Further studies of other mutations confirmed in the OI type V cohort would be instructive.
Interosseous membrane calcification of the forearm is one of the strong pieces of evidence suggesting the diagnosis of OI type V on radiographs. However, it is hard to discern whether it represents calcification of proper interosseous membrane or is due to proliferating and irregular thickening of cortices and periosteum along the interosseous margins of the radius and ulna. Hence, we prefer the descriptive term “cortical thickening/excrescence of interosseous margin” on the radius-ulna diaphyses to classic description of “interosseous membrane calcification.” Exosteal protuberance and cortical thickening were consistently evident along the interosseous margin of the ulna, which was one of the earliest radiographic findings, being observed as early as 4 months of age. In a few patients, the cortical excrescence appeared as a feathery-like pattern on plain radiographs, which seemed to be genuine calcification/ossification in the interosseous membrane itself. Considering follow-up radiographs in some patients, interosseous cortical thickening appeared to progress in extent and width, and seemed to be an ongoing process with age. Interosseous calcification can also be seen along the interosseous margins of the tibia and fibula. This finding was presently observed in patients over 20 years of age and was predominantly involved at the distal tibia and fibula near the ankle joint.
A novel finding in this study was the large coronoid process and olecranon of the ulna, which was the earliest radiographic finding observed. Together with ulna deformity, there seemed to be an accompanying abnormal shape of the radial head. We hypothesize that a large olecranon/coronoid process may affect the development of the radial head, and may induce its dislocation ultimately. It is unknown whether the deformity of the proximal ulna and radial head is a component of skeletal dysplasia that is specifically found in OI type V, or it is an unrecognized simple maldevelopment. A more critical analysis through cases accumulation is warranted in future studies.
A pyramidal shaped chest owing to the downward angulation of the posterior ribs from the costovertebral junction was another common finding observed in our cohort. While the conspicuous feature of the forearm has been emphasized on the radiographic evaluation of OI type V, the sloping of slender ribs has drawn less attention. Only one case report mentioned unusually shaped ribs [Fleming et al., 2005]. All but two patients in our cohort showed downward slanting of the posterior ribs, which was persistently seen in adults over 50 years of age (Fig. 5). The pathomechanism for angulated ribs in OI type V is unclear. One plausible explanation is that ribs may bow due to bone fragility. However, whether an abnormal configuration of ribs was observed more frequently in OI type V or was an unrecognized common finding observed the same as in other types of OI could not be resolved.
HC formation of the long bone is one of the widely used criteria in the literature for the radiographic diagnosis of OI type V [Nakamura et al., 1997; Rieker et al., 1998; Dobrocky et al., 1999; Smith, 2001; Ramirez et al., 2003; Cheung et al., 2007]. In our cohort, HC was found in 12 of 16 patients (75%), a higher frequency than reported previously [Cheung et al., 2007]. HC is most commonly noted in the femur and other long bones are involved infrequently. HC itself is a self-limiting condition and its usual course involves progressive decrease in size over time. However, follow-up radiographs in our cohort showed residual calcified mass and/or exuberant cortical thickening without a total regression of the callus.
A unique finding observed in this study was the heterotopic ossification in the muscle and along the tendon insertion site around the hip joint and femoral shaft. Two patients showed quite extensive ectopic ossification in the hip and knee joints. The heterotopic ossification patterning resembled that of myosits ossificans or fibrodysplasia ossificans progressiva (Fig. 8). This lesion is the most serious complication in the course of OI type V. There must be an unidentified osteogenic potential of extraskeletal tissue in OI type V that produces heterotopic ossification, HC formation, and calcification of interosseous membrane in baseline osteoporotic and fragile bone phenotype of OI. Presumably, the putative dysfunction of the mutant IFITM5 may play some role with different mechanism of skeletal bone deposition in the molecular level than that of a generalized connective tissue abnormality owing to collagen related OI types. Cho et al. hypothesized that the contradictory manifestations of OI type V may be caused by dysregulated process of bone formation effect of the IFITM5 mutation to the tissues where it is expressed [Cho et al., 2012]. The IFITM5 mutation seemed to suppress normal bone formation process in the cortical and trabecular bones, whereas in some places acted as developing ectopic ossification and HC formation. However, verification of this hypothesis and explanation of the pathogenic mechanism would be elucidated through further functional study of the gene. All patients in growing age of this cohort underwent bisphosphonate treatment during varying period of time according to the disease severity, and it seems beneficial for type V OI patients by improving mobility and reducing fracture frequency as previously reported [Fleming et al., 2005; Zeitlin et al., 2006]. However, its efficacy was not analyzed as it is beyond the scope of this study.
In conclusion, the current study confirms commonly recognized clinical and radiographic manifestations of OI type V and extends phenotypic variability by adding new findings. These clinical and radiographic observations will provide clues to recognize this specific subtype of OI more promptly. Correct subtyping in OI can avoid unnecessary expensive and time consuming gene tests by targeted molecular study.




