A broad range of ophthalmologic anomalies is part of the holoprosencephaly spectrum†
How to Cite this Article: Pineda-Alvarez DE, Solomon BD, Roessler E, Balog JZ, Hadley DW, Zein WM, Hadsall CK, Brooks BP, Muenke M. 2011. A broad range of ophthalmologic anomalies is part of the holoprosencephaly spectrum. Am J Med Genet Part A 155: 2713–2720.
Abstract
Holoprosencephaly (HPE) is the most common disorder of the developing forebrain in humans, and is characterized by failed or incomplete cleavage of the cerebral hemispheres and deep brain structures. HPE includes wide phenotypic variability, with a continuum of both brain and craniofacial anomalies. While “classic” eye findings, including the spectrum of midline anomalies ranging from cyclopia to hypotelorism, as well as chorioretinal coloboma and microphthalmia, have been frequently described in patients with HPE, other subtle eye anomalies may also occur. In our study we prospectively analyzed a small cohort of 10 patients in whom we identified mutations in SHH, SIX3, ZIC2, or FGF8, the latter of which is a very recently described HPE-associated gene. We found that 9 of 10 patients had at least two ophthalmologic anomalies, including refractive errors, microcornea, microphthalmia, blepharoptosis, exotropia, and uveal coloboma. These findings contribute to the understanding of the phenotypic variability of the HPE spectrum, and highlight findings in one medically important but often incompletely investigated system. Published 2011. This article is a U.S. Government work and is in the public domain in the USA.
INTRODUCTION
Holoprosencephaly (HPE) is the most common disorder of the developing forebrain in humans, with a frequency up to 1 in 250 conceptuses and approximately 1 in 10,000 live births [Matsunaga and Shiota, 1977; Orioli and Castilla, 2007]. HPE is known to be due to chromosomal anomalies (50% of patients), may occur in the context of syndromes such as Smith–Lemli–Opitz syndrome (SLOS), be due to mutations in Sonic Hedgehog (SHH) [Roessler et al., 1996] and other genes that interact with or are a direct part of the SHH-signaling pathway including SIX3 [Wallis et al., 1999], ZIC2 [Brown et al., 1998], TGIF [Gripp et al., 2000], GLI2 [Roessler et al., 2003], PTCH [Ming et al., 2002], NODAL [Roessler et al., 2009c], and others [Arauz et al., 2010; Ribeiro et al., 2010], involve alterations in cholesterol biosynthesis [Haas et al., 2007], or result from exposure to environmental factors (such as ethanol and retinoic acid during embryonic organogenesis) [Lipinski et al., 2010; Roessler and Muenke, 2010].
HPE is characterized by distinct and complex phenotypic variability. The HPE neuroanatomical spectrum, which includes a progressive gradation of structural brain anomalies, consists of failed or incomplete cerebral hemisphere separation. Classically defined types of HPE range from the alobar form of HPE at the most severe end of the spectrum, to the lobar form of HPE, agenesis of the corpus callosum (ACC), and septo-optic or septo-preoptic dysplasia at the less severe end of the spectrum of patients with structural brain anomalies [Hahn and Barnes, 2010; Hahn et al., 2010].
This spectrum of brain malformations is typically accompanied by a craniofacial phenotypic spectrum of characteristic midline deficits, which includes facial features such as cyclopia, hypotelorism, proboscis, absent nose, absent nasal bone, single nostril, pyriform aperture stenosis, choanal stenosis, and cleft lip/palate. These facial features often correlate with the severity of brain anomalies [Demyer et al., 1964], with some exceptions, such as the case of patients with mutations in ZIC2 [Solomon et al., 2010a].
Some types of ophthalmologic anomalies in patients with HPE are relatively easily ascertained on routine physical examination. These include cyclopia, synophthalmia, hypotelorism, and uveal coloboma. However, more subtle ophthalmologic anomalies may also occur [Schimmenti et al., 2003]. For example, Schimmenti et al. [2003] described a family without any structural brain anomalies in whom a mutation (c.1210_1233del, p.Gly404_Gly411del) in the autocatalytic C-terminus of protein encoded by the SHH gene (NM_000193) was associated with chorioretinal coloboma and iris thinning. This provides an example of how alterations of the SHH-signaling pathway can result in abnormal morphogenesis causing subtle eye anomalies in patients with HPE or microforms of HPE (a diagnosis of “microform” HPE is often given to mildly affected individuals with craniofacial malformations consistent with the HPE spectrum, but who do not have characteristic structural brain anomalies).
The evaluation of patients and their families affected by HPE may include the following: dysmorphology examination, brain imaging, cytogenetic studies, and molecular genetics analyses [Hahn and Plawner, 2004; Levey et al., 2010; Pineda-Alvarez et al., 2010]. However, a careful ophthalmologic assessment is not routinely performed after the initial diagnostic period, especially by specialists highly familiar with the condition. As a consequence, subtle ophthalmological anomalies are, in our experience, often overlooked. As these anomalies may have health consequences, we describe a series of patients with the goal of detailing specific ophthalmologic findings.
METHODS
We analyzed 10 patients with previously identified intragenic mutations or deletions affecting HPE-associated genes (SHH, ZIC2, SIX3, or FGF8, the last of which is a newly identified HPE-associated gene) (Table I). These patients were evaluated at the National Institutes of Health Clinical Center (NIH-CC) in a 2-year period by a multi-disciplinary team including an ophthalmologist geneticist (BPB) highly familiar with the disorder.
| Affected gene | Inheritance | Sequence variant | Domain | Predicted effect | Refs. | Comments | |
|---|---|---|---|---|---|---|---|
| Patients 1 and 2 | SHH | Familial | c.588_602del (p.Gly197_Gly201del) | C-terminus | In-frame deletion including autocleavage site (Cys 198), resulting in possible alteration of protein processing | Patient 2 is the mother of Patient 1 | |
| Patient 3 | SIX3 | De novo | c.769C > T (p.Arg257Trp) | Homeodomain | Intermediate loss-of-function | Domené et al. 2008 | — |
| Patient 4 | SHH | De novo | 46,XX,del(7)(q36). arr cgh 7q36.1q36.3(149,597,103-158,739,800)x1 including SHH | Whole gene | Whole gene deletions have previously been described to cause severe holoprosencephaly; however, incomplete penetrance and variable expressivity are high for this particular locus | Solomon et al. 2010b | — |
| Patients 5 and 6 | SHH | Familial | c.1051C > T (p.Gln351*) | C-terminus | Truncation of C-terminus, resulting in possible alteration of protein processing. | Roessler et al. 2009a | Patient 6 is the mother of Patient 5 |
| Patient 7 | FGF8 | Familial | c.686C > T (p.Thr229Met) | C-terminus | Hypomorphic mutation related with midline defects, including HPE, and idiopathic hypogonadotropic hypogonadism | Arauz et al. 2010, Falardeau et al. 2008 | — |
| Patients 8 and 9 | SIX3 | Familial | c.743_745del (p.Thr248_Gln249delinsLys) | Homeodomain | Possible loss-of-function | Lacbawan et al. 2009 | Patient 9 is the mother of Patient 8 |
| Patient 10 | ZIC2 | De novo | c.612del (p.Tyr205ThrFS*13) | 5′ to Homeodomain | Predicted null due to absence of the homeodomain | Roessler et al. 2009b | — |
Due to logistic considerations, most of the patients invited to the NIH-CC to participate in our study had relatively less severe phenotypes and were stable enough to be evaluated in the outpatient clinics.
RESULTS
General Characteristics
Eight of the 10 patients were female, and 2 were male. Six patients presented with microforms of HPE, two patients had semilobar HPE, and one had lobar HPE. Additionally all patients had documented pathogenic mutations in genes associated with HPE, including SHH in five patients; SIX3 in three patients; and ZIC2 and FGF8, in one patient each, respectively (Table I).
Dysmorphological Findings
All the patients evaluated had craniofacial anomalies consistent with HPE. Among these anomalies were: mild hypotelorism (10/10 patients); depressed midface with depressed nasal bridge (6/10), and single central maxillary incisor (2/10). However, additional structural ophthalmological anomalies were not detected in any of the patients with the initial physical examination prior to examination by an ophthalmologic geneticist. The in-depth ophthalmological evaluation detected a spectrum of ocular and extraocular anomalies in 9/10 patients (Table II). The only patient without such findings was a patient with microform HPE due to a mutation in FGF8 [Arauz et al., 2010].
| Patient (age and gender) | Gene (sequence variant) | Physical exam findings | Other clinical characteristics | HPE brain phenotype | Summary of ophthalmologic anomalies |
|---|---|---|---|---|---|
| Patient 1 (34-year-old female) | SHH: (c.588_602del; p.Gly197_Gly201del) | Single central incisor | None | Microform of HPE | Horizontal corneal diameters 10.5 mm OU. RI: −0.75 OD, −1.75 OS, not requiring correction |
| Patient 2 (12-year-old male) | SHH: (c.588_602del; p.Gly197_Gly201del) | Mild microcephaly, hypotelorism, mildly depressed nasal bridge, single central incisor | Attention deficit/hyperactivity disorder, hypopituitarism, corrected hypospadias | Microform of HPE | Large scleral crescent in OS reminiscent of uveal coloboma, nanophthalmus (axial length of the eye, 21.69 and 22.48 mm in OD and OS, respectively), foveal hypoplasia in OD, horizontal corneal diameters 11.5 mm OU, unilateral blepharoptosis. RI: +1.75 OD and +2.50 OS, not requiring correction |
| Patient 3 (9-year-old female) | SIX3: (c.769C > T; p.Arg257Trp) | Microcephaly, hypotelorism, depressed nasal bridge, single central incisor | Non-verbal, seizure disorder, diabetes insipidus, small kidneys | Lobar HPE, absent septum pellucidum, azygous anterior cerebral artery | Myopia and astigmatism, horizontal corneal diameters: 11 mm OU. RI: −4.5 OU, requiring correction |
| Patient 4 (6-year-old female) | SHH: (46,XX,del(7)(q36). arr cgh 7q36.1q36.3(149,597,103-158,739,800)x1) | Mild microcephaly, hypotelorism, upslanting palpebral fissures | Austism spectrum disorder, non-verbal | Hypoplasia of the left frontal lobe | Hyperopia, astigmatism, 30–40 prism diopters esotropia, horizontal corneal diameters: 11 mm OU. RI: +3.5 OU, requiring correction |
| Patient 5 (2.5-year-old male) | SHH: (c.1051C > T; p.Gln351*) | Hypotelorism, choanal stenosis, depressed nasal bridge, single central incisor, ear tags | Corrected umbilical hernia | Microform of HPE | Myopia, iris and chorioretinal coloboma OD, microcornea OD, horizontal corneal diameters 10 mm OD, 12 mm OS, 40 prism diopter right exotropia and, unilateral (left) blepharoptosis. RI: −4.5 OD, −4.25 OI, requiring correction |
| Patient 6 (25-year-old female) | SHH: (c.1051C > T; p.Gln351*) | Hypotelorism and apparent proptosis, depressed nasal bridge | None | Microform of HPE | Myopia, horizontal corneal diameters, 11.6 mm and 11.5 OD and OI, respectively, asymmetric cupping of the optic nerve (0.5 mm OD vs. 0.3 mm OS), and thinning of the optic nerves nasally OU, more in OS. RI: −3.25 OD, −3.5 OS, requiring correction |
| Patient 7 (8-year-old female) | FGF8: (c.686C > T (p.Thr229Met)) | Hypotelorism, narrow nasal bridge, single central incisor | Light pigmentary pattern | Microform of HPE | Blonde fundus consistent with cutaneous pigmentation. RI: +0.75 and +1.00, not requiring correction |
| Patient 8 (8-year-old female) | SIX3: (c.743_745del; p.Thr248_Gln249delinsLys) | Microcephaly, hypotelorism, depressed nasal bridge, post-surgically corrected midline cleft lip/palate | Hypopituitarism, diabetes insipidus | Semilobar HPE | Myopia, central visual impairment, horizontal corneal length 11 mm OU, mildly dysplastic optic nerve on OD (cup-to-disk ratio: 0.3), fine multivectorial nystagmus, and 30 prism diopters exotropia. RI: −2.5 OU, requiring correction |
| Patient 9 (40-year-old female) | SIX3: (c.743_745del; p.Thr248_Gln249delinsLys) | Hypotelorism, and single central incisor | Hypothyroidism | Microform of HPE | Myopia, bilateral punctate cortical cataracts (+1), myopic crescent in OS, 14 prism diopter hypertropia on OS, and apparent bilateral inferior oblique underaction. RI: −8.25 OD, −6.75 OS, requiring correction |
| Patient 10 (5-year-old female) | ZIC2: (c.612del; p.Tyr205ThrFS*13) | Microcephaly, hypotelorism, and depressed nasal bridge | Diabetes insipidus | Semilobar HPE, absence of the corpus callosum | Hyperopia, hyperopic astigmatism microcornea with horizontal corneal diameters of 10 mm OU. RI: +1.50 OU |
Ocular anomalies
Among the ocular anomalies identified, the most common anomalies were refractive errors. Nine of 10 patients had refractive errors of varying severity, 6 of which necessitated corrective lenses; 1 of the 6 also suffered cortical visual impairment. Six of 10 patients presented with smaller than average horizontal corneal diameters (Fig. 1A). Of the six patients with small corneal diameters, two had borderline microcornea, with horizontal corneal diameters of 10 mm [Rufer et al., 2005]. In one of these patients (Patient 5), a borderline horizontal corneal diameter was accompanied by a chorioretinal coloboma. Although, the horizontal corneal diameters appeared to be smaller than average, the number of patients in this cohort is too small to attempt further statistical analyses regarding this finding.
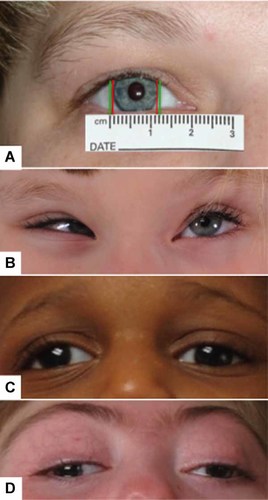
A: Illustration of the horizontal corneal diameter of Patient 1, an adult female patient with a microform of HPE due to a SHH mutation in the C-terminus of the gene; corneal diameters measured ∼10 mm (distance between red bars), while the average is ∼12 mm for adult women (distance between green bars). B: Patient 4, a child with a 7q36 deletion including SHH, presented with hypotelorism, upslanting palpebral fissures, and esotropia. C: Patient 5, a child with a microform of HPE due to a SHH mutation in the C-terminus of the gene, presented with hypotelorism, right exotropia, and left blepharoptosis. D: Patient 8, a child with semilobar HPE due to a SIX3 mutation, presented with hypotelorism, and right exotropia.
Other ocular anomalies presented with lower frequency. These included: chorioretinal coloboma (1/10, same patient mentioned above), subtle retinal and optic nerve anomalies (3/10), simple microphthalmia, and narrow anterior chamber resulting in an increased risk for the development of closed-angle glaucoma (1/10). One patient with a SIX3 mutation had “pre-senile” cortical cataracts, which while perhaps not medically significant, may indicate a developmental alteration related to the HPE-associated mutation.
Extraocular anomalies
Besides anomalies that involve eye spacing (in our cohort, evident as hypotelorism), other extraocular anomalies were identified. These included strabismus (4/10) (Fig. 1): exotropia (2/10), esotropia (1/10), and inferior oblique muscle underaction, in addition, to hypertropia (1/10). The other extraocular manifestation noted was unilateral blepharoptosis, which was present in two unrelated patients in our cohort, who had two different mutations in the C-terminus of SHH.
DISCUSSION
From a developmental standpoint, eye morphogenesis is a complex process, and proper patterning requires extremely well-coordinated temporo-spatial and dosage-dependent interactions between molecules, including PAX6, SHH, PAX2, FGF8, BMP4, and TBX5. Alterations in the signaling of any of these molecules, all of which are also involved in forebrain patterning, have been postulated to produce defects in the antero-posterior and ventral-dorsal development of the eye, resulting in intraocular anomalies [Kobayashi et al., 2010].
PAX6, for instance, is the main inducer of the optic vesicle and is expressed in either side of the diencephalon of the developing embryo. PAX6 expression is repressed by the prechordal plate (presumably due to SHH expression in the ventral midline), maintaining eye-field separation. Variable degrees of loss-of-function within the SHH pathway may explain mild to severe presentation of eye non-separation (ranging from mild hypotelorism to synthophthalmia and cyclopia) [England et al., 2006].
On the other hand, PAX2 expression is induced by SHH activity in the ventral aspect of the optic vesicle, and PAX2 [Kobayashi et al., 2010] has an important role in the closure of the optic fissure along the ventral optic cup and stalk [Carlson, 2009]. Failure of optic fissure closure results in a uveal coloboma, compromising one or multiple structures of the eye, which can include the iris, ciliary body, choroid, retina, and/or optic nerve [Guercio and Martyn, 2007]. This supports the role of SHH in the pathogenesis of this defect in patients reported in this and other studies [Schimmenti et al., 2003; Bakrania et al., 2010], although, coloboma in patients with mutations in PAX2 occurs at a rather low frequency.
Correlating with the concepts above, four of the patients with mutations in the C-terminus of SHH presented with craniofacial microforms of HPE and ocular anomalies, but without structural brain anomalies. Two additional studies have demonstrated the occurrence of mutations in the C-terminus of SHH in patients with isolated ocular anomalies [Bakrania et al., 2010]. Although the functional consequences of mutations in the C-terminus of SHH were initially unknown, a recent study demonstrated that mutations in this region of the gene affect autocatalytic cleavage, altering normal processing to mature SHH (SHH-Np). In this scenario, although the full-length (i.e., non-cleaved) SHH has activity, its ability to generate further signaling is impaired [Traiffort et al., 2004; Tokhunts et al., 2010]. These findings may help explain part of the phenotypic variability observed in patients with mutations in SHH [Solomon et al., 2010b], and highlights the role of SHH and the molecules related to its signaling pathway in eye development.
Attempting to correlate the “extraocular anomalies” with the molecular defects in this patient cohort is challenging for a number of reasons, including the small number of patients studied. For instance, strabismus may be seen in patients with structural brain anomalies regardless of the underlying condition, although only one of the four patients in our cohort who had strabismus had a brain malformation. We observed two unrelated proposita with blepharoptosis who had mutations in the C-terminus of SHH; carrier siblings of both patients (not included in this cohort) were observed to have blepharoptosis as well. It is difficult to extrapolate further from this observation, except that patients with SHH mutations bear scrutiny for this and other ophthalmologic disturbances. Nevertheless, from a developmental standpoint, this observation is interesting, as SHH has been described to regulate the patterning of nuclei in the midbrain in mice [Perez-Balaguer et al., 2009]. Some of these nuclei are involved in the control of ocular and palpebral motility.
From the clinical standpoint, many of these ocular anomalies cause complications that may be anticipated and managed through follow-up by a specialized ophthalmologist familiar with HPE. For instance, besides the visual defects, a severe coloboma compromising the retina or optic nerve increases the risk of retinal detachment and choroidal neovascularization. Moreover, patients with microphthalmia are at risk of closed-angle glaucoma due to a smaller anterior chamber [Guercio and Martyn, 2007]. Although patients in this cohort did not present with high degree myopia (defined as a refraction index less than −5D), the natural history of myopia in individuals with HPE-associated mutations is not well characterized, and comparisons with “unaffected” individuals are difficult, hence the incidence of complications are not known. Certain patients, especially those with brain anomalies, present with cortical visual impairment; for these patients, vision does not improve despite adequate correction of the refraction error.
Strabismus appears to be relatively frequent in patients within the HPE phenotypic spectrum; it is of extreme importance to detect heterotropias, since, even slight deviations may result in amblyopia and loss of stereopsis. Patients presenting with documented ocular deviations (and presumably without major brain anomalies) should be treated appropriately, with the goal of establishing binocular vision and orthophoria (proper eye alignment) [Olisky et al., 2007]. In summary, we show that subtle intraocular anomalies such as refraction errors, borderline microcornea, retinal thinning or positioning of the optic nerve, uveal and chorioretinal coloboma, microphthalmia (including nanophthalmia), and extraocular anomalies such as strabismus and blepharoptosis are common in patients within the HPE phenotypic spectrum and with mutations in SHH or genes related to its signaling pathway. Therefore, routine and careful ophthalmologic evaluation of these patients is indicated, as some of these subtle anomalies require intervention and follow-up. Further, these findings may provide insights into potential genotype–phenotype correlations and our understanding of the broad and emerging clinical spectrum of HPE.
Acknowledgements
We would like to thank the patients, and families for their continued support of research investigations into the genetic basis of HPE and its clinical manifestations. This work was supported by the Division of Intramural Research (DIR) of the National Human Genome Research Institute.




