Femoral–facial syndrome: Prenatal diagnosis and clinical features. Report of three cases†
How to Cite this Article: Nowaczyk MJM, Huggins MJ, Fleming A, Mohide PT. 2010. Femoral–facial syndrome: Prenatal diagnosis and clinical features. Report of three cases. Am J Med Genet Part A 152A:2029–2033.
Abstract
The objective of our article is to illustrate the earliest prenatal sonographic diagnosis of femoral–facial syndrome (FFS) and to illustrate the spectrum of clinical manifestations of this condition. We present serial sonographic evaluation with 3D evaluation in two fetuses diagnosed prenatally with FFS and the postnatal findings in three patients (one fetus following pregnancy interruption and two newborns one of whom was diagnosed prenatally) with FFS. The two patients with prenatally diagnosed FFS were found to have femoral shortening and characteristic facial features, one 12 weeks of gestation, and one at 15 weeks of gestation. The sonographic findings in the two prenatally diagnosed patients were confirmed after delivery. We also present a third patient who was diagnosed at delivery in whom the diagnosis was missed at a routine prenatal sonogram at 19 weeks of gestation. The patients reported herein expand the clinical spectrum of FFS. The utility of sonographic evaluation in diagnosis of the facial appearance and of the bony abnormalities in this condition is emphasized. © 2010 Wiley-Liss, Inc.
INTRODUCTION
Femoral–facial syndrome (FFS) (OMIM 134780) (also known as femoral hypoplasia-unusual facies syndrome or proximal femoral deficiency), is a rare and sporadic multiple anomaly syndrome of unknown etiology, although it is known to be associated with maternal type 1 diabetes mellitus (DM). It comprises bilateral femoral hypoplasia and characteristic facial features which include long philtrum, thin upper lip, micrognathia with or without cleft palate, upward-slanting palpebral fissures, and a short nose with broad tip [Burn et al., 1984]. The ears may be dysplastic or low set. Additional birth defects that may be observed in FFS include sacral dysgenesis, humeroradial synostosis, renal anomalies such as renal agenesis or dysplasia, multicystic kidneys or abnormal collecting urinary system and genital anomalies including cryptorchidism, hypoplastic labia, and microphallus. To date, all reported cases were sporadic and no sib recurrences have been reported suggesting non-genetics causes such as teratogenic exposure although a new dominant mutation and reduced penetrance are also possible.
Prenatal findings in facial femoral syndrome have been reported in 12 patients [Tadmor et al., 1993; Robinow et al., 1995; Hinson et al., 1996; Campbell and Vujanic, 1997; Gillerot et al., 1997; Urban et al., 1997; Filly et al., 2004; Paladini et al., 2007; Ho et al., 2008; Figureoa et al., 2009] in whom femoral hypoplasia varied from minimal shortening with minimal bowing to complete femoral agenesis. Characteristic facial findings were observed after delivery. The prenatal diagnosis the femoral anomalies varied from 19 to 32 weeks gestation.
We report on two patients with severe FFS diagnosed prenatally—one at 12 weeks gestational age (GA) and one at 15 weeks gestation. To our knowledge these are the earliest prenatally diagnosed cases of FFS. We also report one patient with classic FFS missed on detailed fetal sonogram at 19 weeks gestation.
CLINICAL REPORTS
Patient 1
Patient 1 was a girl born to a 27-year-old gravida 2 para 1 live 1 with a 2-year history of poorly controlled type 1 DM. A fetal ultrasound at 12 weeks gestation detected short femora and micrognathia (Fig. 1). The nuchal translucency (NT) was 2.5 mm. The mother decided to continue the pregnancy and monthly sonographs documented severe shortening of the femora, tibiae, fibulas, sacral segmental dysgenesis, and left humeroradial synostosis. A 3D evaluation at 25 weeks gestation showed severe micrognathia, upturned nose, and prominent cheeks characteristic of FFS (Fig. 2A,B).
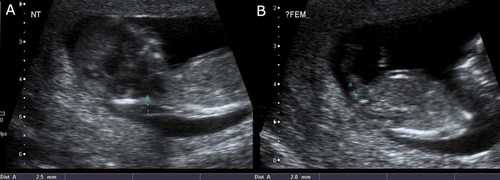
Patient 1. Sonogram at 12 weeks gestation (crown-rump measurement 54 mm) showing: A: NT of 2.4 mm and severe micrognathia; and (B) shortening of the legs with femoral length of 2 mm.

Patient 1. Sonogram at 25 weeks gestation and photographs at birth (day 2 of life). 3D sonogram showing the characteristic frontal view with recessed chin with horizontal crease, large cheeks, and small nose with anteverted nares (panel A); typical overlapping upper lip with beaked nose and protuberant cheek (panel B); and short legs consisting of fibula and tibia bilaterally and clubbed ankles (panel C). [Color figure can be viewed in the online issue, which is available at www.interscience.wiley.com.]
Delivery was at term and induced. The newborn sustained a fracture of the right radius. She had micrognathia with a horizontal chin crease, a narrow mouth and full cheeks, a short nose with anterverted nares and a broad tip, and a long and deep philtrum (Fig. 2A,B). She had glossoptosis, with an U-shaped cleft soft palate. She had a normal chest and a short neck. The proximal segments of both arms were short with severely reduced pronation and supination of the elbows; there was no flexion or extension possible. The thighs were essentially absent (Fig. 2C). External genitalia were normal and female. She had bilateral clubfeet, overriding toes, and fork-like 2–3 toe syndactyly, symphalangism of both thumbs and abnormally overlapping fingers. Radiographs showed absent right femur, severe shortening of left femur, bilateral humeroradial synostosis, a fracture of the proximal right radius, 11 pairs of ribs, and a sacrum convex to the right with only 3 vertebra (Fig. 3). The karyotype was normal female, 46,XX.

Patient 1. Postnatal radiographs showing: A: absent femur on the right and femoral shortening on the left; and (B) bilateral humeroradial synostosis.
Patient 2
The mother was a 31-year-old gravida 1 para 0 live 0 with type 1 DM and plasma HbA1c of 8.9% at the time of conception. NT measurement at 12 weeks gestation was 1.0 mm. She was referred at 15 weeks gestation because of sonographic findings of absent or short femora, asymmetry of leg bones and abnormal facial profile with microretrognathia (Fig. 3). The fetal BPD was 39 mm, head circumference was 143 mm, and abdominal circumference was 113 mm; all compatible with 17.3 weeks gestation. The femora were not measurable, the tibiae were asymmetric and measured 16.5 and 18 mm (normal for 17 weeks gestation 22 mm) on the right and left, respectively, and the fibulae 15 and 18.5 mm, respectively (normal for 17 weeks gestation 19 mm) and the sacral vertebrae were disorganized. There was also bilateral cerebral ventriculomegaly. The pregnancy was interrupted at 20 weeks gestation. At autopsy, the fetus had a small mouth with marked retrognathia and hypoplastic mandible, long philtrum, thin upper vermilion border, and bilateral low-set dysplastic ears (Fig. 3A). There was a cleft soft palate and glossoptosis. The upper limbs showed contractures at the shoulders with pterygia across the axillae, and both wrists in flexion position. The legs consisted primarily of tibia and fibula with bilateral club feet. The fetus had renal hypoplasia (combined renal weight was 0.87 g, expected mean weight 2.7 g), disc-shaped adrenals, absent uterus and vagina with normal ovaries, bilobed lungs, and hydrocephalus. A radiograph of the fetus showed bilateral humeroradial synostosis, bilateral severe hypoplasia of the femora and disorganized sacrum (Fig. 4). The karyotype was normal female, 46,XX.
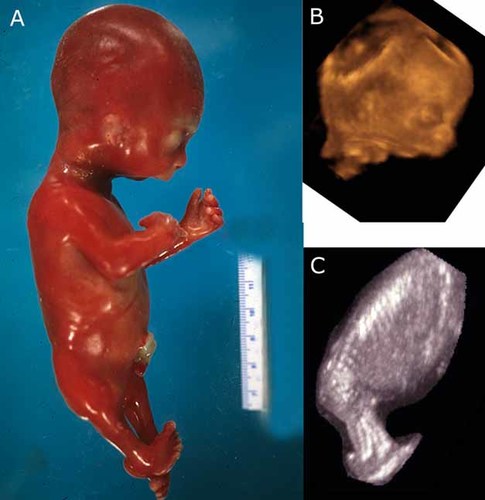
Patient 2. 3D sonogram at 18–19 weeks gestation showing absent femora (panel C), severe micrognathia (panel B), and the appearance of the fetus after therapeutic termination of pregnancy at 20 weeks gestation (panel A). [Color figure can be viewed in the online issue, which is available at www.interscience.wiley.com.]
Patient 3
This was a boy born following an uncomplicated pregnancy and delivery at 36 weeks gestation. A fetal sonogram at 19 weeks gestation performed in a community clinic was reported as normal with a documented “femoral” length of 28 mm, compatible with 18 weeks gestation, with BPD, abdominal circumference and head circumference compatible with 19 weeks gestation. The cerebellum, cerebral ventricles, bladder and kidneys, spine, stomach, and limbs, hands and feet were reported as normal. Facial profile views were not obtained and no follow up was arranged. At birth he had a cleft palate, microretrognathia, bilateral femoral deficiency; his facial features included narrow mouth, small chin, prominent cheeks, bilateral epicanthal folds, short and upslanting palpebral fissures. The sonographic images were reviewed by a panel of radiologists after the delivery of the child and no diagnostic features were noted. As per parents' wishes karyotype was not done.
DISCUSSION
FFS is a rare sporadic multiple anomaly syndrome of unknown etiology; it comprises bilateral femoral hypoplasia, characteristic facial features (long philtrum, thin upper lip, micrognathia, cleft palate, upslanting palpebral fissures, short nose with broad tip) and other malformations which may affect the skeleton and genitourinary system. The finding of fetal micrognathia and short bowed femora on prenatal sonogram should lead to the consideration of FFS in the differential diagnosis, especially in the setting of maternal DM.
Two of the three patients presented herein lie at the severe extreme of the clinical spectrum of FFS. Patient 1 presented with the most severe shortening of the extremities that was clearly demonstrated at 12 weeks gestation. Patient 2, in addition to the facial dysmorphism, femoral shortening, and sacral agenesis, had absence of internal genitalia which has not been previously reported, and cerebral ventriculomegaly, reported previously by Ho et al. 2008. The third patient, who had classic phenotype of FFS, had a reported “normal” femoral length at 19 weeks gestation.
MEDLINE search identified 10 articles, reporting a total of 13 patients of FFS that included prenatal data (Table I). Eight report femoral hypoplasia at 18–21 weeks gestation, which was the first sonographic evaluation; Urban et al. 1997 report a normal sonographic evaluation “limited” by maternal body habitus at 18 weeks gestation. One article [Paladini et al., 2007], reports a diagnosis of FFS at 13 weeks gestation with identification of symmetrically hypoplastic femora and severe micrognathia confirmed clinically after a termination of pregnancy. In four other patients prenatal US was not performed until late in the second trimester: 25, 26, and 32 weeks gestation, at which point femoral hypoplasia was detected [Tadmor et al., 1993; Robinow et al., 1995; Hinson et al., 1996; Gillerot et al., 1997]. Tadmor et al. 1993 reported a measurement of the femora at 19 and 21 weeks gestation which were within normal limits, followed by the detection of femoral hypoplasia at 32 weeks gestation, which they interpreted as “growth arrest” occurring sometime in the third trimester. However, neither other reports nor our observations support this theory: in Patient 1 we documented a normal rate of growth of an otherwise shortened and malformed bone.
| Refs. | Gestational age (weeks) | Prenatal finding | DM | Outcome | Postnatal findings |
|---|---|---|---|---|---|
|
Tadmor et al. 1993 |
32, previous normal US at 19 and 23 | Cleft palate, short femora (42 mm 50th centile for 24 weeks) short humeri (45 mm 50th centile for 27 weeks) | No | Term delivery | Cleft lip and palate, short thigh, short proximal arms, sloping shoulders, hypoplastic left scapula, cryptorchidism, shawl scrotum, single palmar creases |
|
Robinow et al. 1995 |
25, 30 | Micrognathia, short bowed femora femoral length 33 mm (c/w 20 weeks), humerus length 46 mm (c/w 27 weeks) | No | Term delivery | Characteristic face, cleft palate, short thighs |
|
Hinson et al. 1996 |
Right femur 22 mm, left femur 17 mm (<3rd centile), other bones at or <5th centile, abnormal hands, polyhydramnios | Yes | Term delivery, death due to sepsis | Cleft lip and palate, low-set ears, micrognathia, upslanting palpebral fissures, 1–2 hand syndactyly, 5th finger clinodactyly, sacral and gluteal dimples, 11 ribs on the left, thoracic hemivertebra, small kidneys | |
|
Campbell and Vujanic, 1997 |
18+ | Absent femora | Yes | TOP at 19 weeks | Absent femora, bilobed lungs, interrupted vena cava below diaphragm, right pelvic kidney with duplex collecting system, left hydroureter |
|
Urban et al. 1997 |
21, normal “limited” US at 18 | Short femora, short humeri, short forearms | GDM | In utero demise at 40 weeks | Characteristic face, U-shaped cleft, palate absent femora, short humeri, short tibiae and fibulae, hypoplastic scapulae, sacral dysgenesis, 11 pairs of ribs digitalization of thumbs hypoplastic nails, club feet, unilateral renal agenesis, bilateral cryptorchidism, anterior tracheal defect, lung hypoplasia |
|
Gillerot et al. 1997 |
26 | Short femora c/w 21 weeks | No | Premature delivery at 31 weeks, death | Characteristic face, cleft palate, short and bowed thighs, distal arthrogryphosis, 3rd and 4th camptodactyly, sacral hemivertebrae, corpus callosum—partial agenesis, neuronal heterotopias, bilobed right lung, intestinal malrotation |
|
Filly et al. 2004, Patient 2 |
19.1 | Proximal focal femoral hypoplasia, bilateral club feet normal face | No | TOP | Micrognathia, depressed nasal bridge, no other details |
|
Paladini et al. 2007 Patient 1 |
21.0 | Absent left femur, right femur “few” mm, right cleft lip and palate, right renal agenesis | No | TOP | Cleft lip and palate, long philtrum, thin upper lip, moderate micrognathia, low-set ears, short neck, absent left femur, right femur hypoplasia, vertically oriented iliac blades, right renal agenesis |
| Patient 2 | 21.0 | Severe hypoplasia left femur, normal right femur, severe micrognathia, low set ears | Yes | TOP | Cleft palate, sever micrognathia, low-set ears, short nose with broad tip, thin upper lip, hypoplastic left femur, normal right femur |
| Patient 3 | 13.0 | Hypoplastic femora, moderate micrognathia, normal NT | No | TOP | No details |
|
Ho et al. 2008 |
20 | Cerebral ventriculomegaly, hypoplastic femora, club feet | Yes | Delivery at term | Characteristic face, Robin sequence, long featureless philtrum, short legs, club feet, hydrocephaly, agenesis of posterior corpus callosum |
|
Figureoa et al. 2009 |
21.1, normal US at 13 weeks gestation | Femora 15 mm, microretrognathia | No | TOP | “Marked” micrognathia, low-set ears, femoral hypoplasia |
- DM, diabetes mellitus; GDM, gestational diabetes mellitus; TOP, termination of pregnancy; NT, nuchal translucency; c/w, compatible with.
We detected femoral shortening in two patients in either late first or early second trimester. However, we noted difficulties in identifying the absence of a femur on a 2D sonogram: at times other bones were mistakenly identified and measured for a femur; these could be either tibiae or the lower elements of the pelvis. This is what occurred on two occasions in our Patient 1, where a “femur” was being measured between 15 and 21 weeks gestation. The severe shortening of the femur—noted at 13 weeks gestation—was confirmed by a 3D sonogram at 25 weeks gestation and on the postnatal radiographs. In Patient 3, it is likely that another bone was measured at 19 weeks gestation delaying the diagnosis of FFS until after term delivery.
In contrast to the difficulties with 2D imaging of the severely shortened or absent femora, the views of the face showed unmistakable features of FFS—severe microretrognathia, long convex philtrum, and full cheeks both on 2D and 3D views. The micrognathia was obvious at the 13-week gestation 2D profile view, and the overall facial gestalt was very well visualized with 3D views at 25 weeks gestation.
NT measurement was normal in the two FFS patients with NT measurement reported in the literature [Patient 3, Paladini et al., 2007; Figureoa et al., 2009]. Our three patients had normal NT measurements at 12–13 weeks gestation suggesting that, unlike many other skeletal syndromes, FFS is not associated with increased NT.
Our report illustrates the utility of 3D imaging in the delineation of femoral hypoplasia in general and in the diagnosis of FFS in particular.




