Metachromatic leukodystrophy in the Navajo: Fallout of the American-Indian wars of the Nineteenth Century†‡
The opinions in this article are those of the authors and are not those of the United States Public Health Service.
This article was prepared by a group consisting of both United States Government employees and non–United States Government employees, and as such is subject to 17 U.S.C. Sec. 105.
Abstract
Our aim was to determine if the high frequency of metachromatic leukodystrophy (MLD) in Navajo Indians of the Southwestern United States is the result of a “genetic bottleneck” that occurred in the mid 19th century. Navajo Nation, Indian Health Service, and other national databases were queried for Native American patients with MLD. Pedigrees, including birth location, were established by interviewing relatives. We found that cases of MLD and their ancestors are clustered in a portion of the western Navajo Nation to which a small number of Navajo fled after armed conflict with the United States Army in the 1860s. The observed incidence of MLD on the western Navajo Nation is 1/2,520 live births, with an estimated carrier frequency of 1/25 to 1/50. No cases were observed in the eastern part of the Navajo Nation over a period of 18 years (60,000 births). The high incidence of MLD in the western Navajo Nation appears to be the result of a genetic bottleneck and probable founder effect from the mid 19th century: This mechanism may also explain the high incidence of a number of other unique, heritable disorders among the Navajo. The history of the Navajo may also be relevant to other American Indian and Alaskan Native groups that have undergone severe population reduction since the arrival of Europeans in North America. © 2001 Wiley-Liss, Inc.
INTRODUCTION
The arrival of Europeans into North America set in motion a precipitous decline in the Native American population. Experts argue over the proportional contribution of disease, famine, warfare, and outright genocide to this demographic catastrophe, but it is thought that the indigenous population declined from roughly 6,000,000 at the end of the 15th century to less than 250,000 at the close of the 19th century [Denevan, 1976].
Such drastic reduction in population size, in association with random genetic drift, can cause a so-called “genetic bottleneck.” After such a “bottleneck,” the new population will likely reach a new Hardy-Weinberg equilibrium, leading to an increased frequency of previously rare recessive alleles and previously uncommon autosomal recessive disorders [Roberts, 1968].
Metachromatic leukodystrophy (MLD) is an autosomal recessive disorder of sphingolipid metabolism in which deficiency of the lysosomal enzyme arylsulfatase A (ARSA) leads to progressive demyelination of the white matter [Kolodny and Fluharty, 1995; Polten et al., 1991]. In the most common form, late infantile MLD, patients present between the first and second year of life with incoordination progressing to spastic quadriparesis. Death usually occurs by age five years. MLD is a panethnic disease with an estimated incidence ranging from 1/40,000 to 1/130,000 births [Scriver et al., 1995].
Between 1990 and 1992, four Navajo Indian children were diagnosed with late infantile metachromatic leukodystrophy at a small, rural hospital on the western Navajo Nation. In 1994, further investigation showed that all four Navajo patients were homozygous for a unique splice site mutation in intron IV of the ARSA gene [Paster-Soler et al., 1994]. It is known that the Navajo underwent a severe population reduction in the mid 19th century as a result of armed conflict with the United States. We hypothesized that the observed cluster of Navajo Indians with MLD might be the result of a genetic bottleneck in the previous century. We undertook a study to identify all known Navajo patients with MLD and the geographic pattern of disease.
BACKGROUND
The Navajo are the second largest tribe in North America with 219,000 enrolled members as of the 1990 census, of which 151,000 reside on the Navajo Reservation in the Southwestern United States. The Navajo are considered Athabascan Indians with genetic and linguistic links to the small population of Nadene tribes in Alaska and Northwest Canada as well as the Apache in the Southwest. Navajo creation stories tell of their people emerging from the underworld to the surface of the earth in what is now Northwest New Mexico [Underhill, 1956]. Anthropologists suggest that the Athabascan tribes, including the Navajo, arose in central Asia and migrated across the Bering Strait to Alaska approximately 10,000 years ago [Cavalli-Sforza et al., 1988; Szathmary, 1984]. The Navajo gradually migrated southwards, and earliest evidence of their presence in Arizona and New Mexico dates back to the 15th century [Kluckhorn, 1946].
The arrival of American settlers to the Southwest in the mid 19th century led to increasing conflict over grazing land. In 1864 nearly the entire tribe of 8,000 Navajo were forced by the United States Army from their homeland on the Arizona/New Mexico border to exile at Fort Sumner in eastern New Mexico, an event known in Navajo history as “The Long Walk.” During “The Long Walk” and subsequent four years of captivity at Fort Sumner, roughly 40% of the population died [Link, 1971]. In 1868 the surviving tribal members were placed on reservation land where the vast majority live today. In spite of these hardships, the Navajo people have thrived. Over the past 130 years the fertility rate of the Navajo Nation has been double that of the United States, such that the Navajo population has increased from 6,000 members after “The Long Walk” to over 219,000 today [Howard, 1993].
Of particular interest is a group of less than 1,000 Navajo [Link, 1971; Johnston, 1966] who avoided incarceration at the time of “The Long Walk” in 1864 by fleeing to the rugged and inaccessible areas around Navajo Mountain and the Little Colorado River in what is now the western portion of the Navajo Nation (Fig. 1) [Navajo Tribal Council, 1987]. Oral history of local elders suggests that the western portion of the Navajo Nation has been geographically and genetically isolated until the past few decades. Paved roads were not built until the early 1960s, and to this day Navajo Mountain remains accessible only at the end of a 40 mile dirt road.
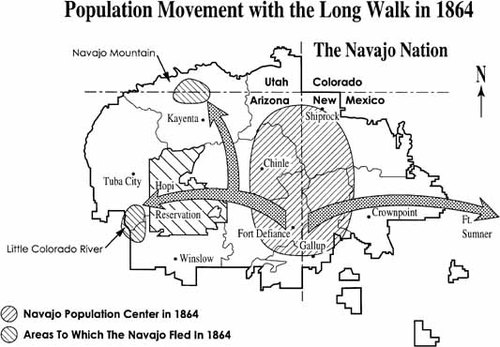
Population movement with “The Long Walk” in 1864.
METHODS
The Indian Health Service (IHS) offers medical care to all enrolled members of Native American tribes. All Navajo who reside on the Navajo Nation, as well as many who do not, receive some or all of their care through this system. The Navajo Nation is divided into eight administrative service units through which all medical data are collected. The service units of Tuba City, Kayenta, and Winslow encompass the western portion of the Navajo Nation.
We reviewed pediatric chronic disease registries and queried Navajo Area computerized databases to identify patients with MLD. To identify Navajo MLD patients not living on the reservation, as well as other Native Americans with MLD, the National IHS database was searched. The laboratory that performs the bulk of lysosomal enzyme testing for the IHS was asked to review their registry and identify any additional Native Americans with MLD.
Pedigrees and birthplace data were obtained by interview of family members. There is no traditional written form of Navajo and little historical record before the census of 1928, but oral tradition was deemed reliable as far back as four generations [Kelly, 1964]. Permission to obtain data was approved by the Navajo Nation Institutional Review Board.
RESULTS
We initially identified four patients in Tuba City with MLD who shared a specific ARSA mutation. Review of records from 1977 to 1995 identified an additional six patients, giving a total of 10 patients from nine families with a confirmed diagnosis of MLD. One of these additional patients was still living and was found to share the same ARSA intron IV mutation as the original four Navajo patients tested. The other five patients were deceased, and no tissue or blood samples were available.
No consanguinity was identified as far back as four generations. However, the geographic distribution of probands and ancestors was most striking. Patients and ancestors were not from areas of original Navajo settlement on the Arizona/New Mexico border. Instead, 8/10 were from the service units of Tuba City, Kayenta, and Winslow on the western Navajo Nation (Fig. 2a). The other two patients were born off-reservation in Phoenix and Salt Lake City, reflecting the tendency in recent years of many younger Navajo to leave the reservation to find employment. As birthplaces of each previous generation were mapped, there was increased geographic clustering (Fig. 2b and 2c): a plotting of the birthplace of all known great grandparents (Fig. 2d) shows nearly exclusive concentration in the areas around Navajo Mountain and the Little Colorado River. The birthplaces of these ancestors is congruent with the areas (shown in shading) to which the Navajo fled to avoid capture by the U.S. Army in 1864.
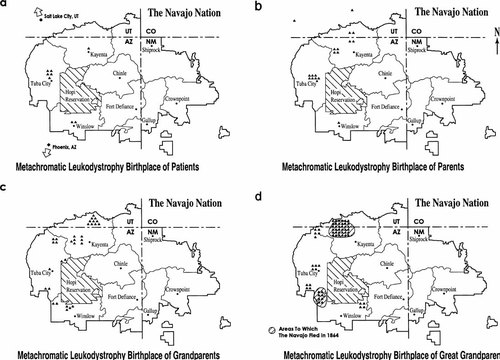
a: Birthplace of MLD patients. b: Birthplace of parents of MLD patients. c: Birthplace of grandparents of MLD patients. d: Birthplace of great grandparents of MLD patients.
The western Navajo Nation encompassing the service areas of Tuba City, Kayenta, and Winslow had a combined population of 49,000 as of the 1990 census. On average, this area had 1,400 births per year over the past 18 years, including the approximately 20% of Navajo births that occur off reservation [Navajo Area Indian Health Service, 1997]. Based on these data, we calculated the incidence of MLD for the western Navajo Nation at 1/2,520 live births. Over the same period (1977–1995), there was a total of approximately 60,000 births in the other five service units of the Eastern Navajo Nation with no identified cases of MLD.
The coefficient of inbreeding for this isolated population is not known. A variety of cultural taboos are in place through the traditional clan system to prevent consanguinity. Pedigree analysis for the families demonstrated no documented consanguinity as far back as four generations. However, coefficient of inbreeding for the Navajo has been estimated at approximately 0.008 [Spuhler and Kluckhorn, 1953]
| Observed incidence (R) | Carrier frequency (2pq) | Coefficient of inbreeding (α) | Expected incidence in a randomly mating population (q2) | Normal allele frequency (p) | Mutant allele frequency (q) |
|---|---|---|---|---|---|
| 0.0004 | 0.01 (1/100) | 0.075 | 0 (1/40,000) | 0.995 | 0.005 |
| 0.0004 | 0.014 (1/75) | 0.05 | 0 (1/20,500) | 0.993 | 0.007 |
| 0.0004 | 0.02 (1/50) | 0.03 | 0.0001 (1/10,000) | 0.99 | 0.01 |
| 0.0004 | 0.03 (1/32) | 0.009 | 0.0003 (1/3333) | 0.984 | 0.016 |
| 0.0004 | 0.04 (1/25) | 0.00 | 0.0004 (1/2500) | 0.98 | 0.02 |
A ten-year search of the national IHS database and the registry of the reference laboratory uncovered no other Navajo with MLD. One other Athabascan Indian, a Yavapai Apache from central Arizona, was identified with a diagnosis of MLD. This patient was deceased, and no tissue was available for genetic testing. As of the 1990 census there were approximately 35,000 non-Navajo Athabascan Indians (the Nadene and Dogrib in the Northwest and the San Carlos, White Mountain, Yavapai, Tonto, Mohave, Jicarilla, and Mescalero Apache in the Southwest). During this time these Athabascan bands had on average a total of 900 births per year, suggesting that the incidence of MLD in these groups is at most 1/9,000, and likely much less.
DISCUSSION
Genetic bottlenecks are known to put isolated populations at risk for unusual heritable illnesses. In many of these groups genealogical studies using written records have identified a common ancestor hundreds of years in the past, suggesting a founder effect as the cause for the high frequency of disease. [Laberge, 1969; O'Brien et al., 1994]
An identifiable founder for Navajo MLD is currently unknown, and probably unknowable, given the lack of written records prior to the 1928 census [Johnston, 1966]. Our data show that the ancestors of all of the Navajo MLD patients are from the same isolated region of the Navajo Nation. We think the Navajo ARSA mutation was established at a new, higher frequency in the western Navajo people as a result of genetic drift and a significant population bottleneck in the mid-19th century. Unfortunately, we are not able to evaluate the haplotypes of the families to document identity by descent from a single, or small number, of common ancestors. While mutation analysis is available for only five of the 10 patients, it is likely that all 10 share the same mutation based on the isolated geographic origin of the ancestors. This hypothesis is supported by the recent demonstration of strong linkage disequilibrium for an ancestral haplotype in Navajo patients with severe combined immunodeficiency (SCID) Athabascan type (OMIM 602450) [Li et al., 1998].
The splice site mutation of intron IV of the ARSA gene found in the Navajo was initially thought to be unique. However, recent work shows that the Yupik Eskimos in western Alaska also have a high incidence of late infantile MLD and share the same genotype as the Navajo [Paster-Soler et al., 1995]. The Yupik and the Navajo are not thought to be close genetically as they are alleged to have entered North America from central Asia in two separate migrations up to 5,000 years apart [Wallace and Torroni, 1992]. This would imply that the ARSA mutation is much older, and arose from a common ancestor of the Navajo and Yupik in central Asia. An alternative explanation is that this mutation arose in either the Yupik or ancestral Navajo, and there was genetic admixture prior to the migration of the Navajo into the southwest.
If the ARSA mutation predates Navajo migration to the Southwest, it may be present in other Athabascan populations. The finding that the only other non-Navajo, non-Eskimo Native American with MLD was Athabascan is intriguing in this regard. The apparently low frequency of this mutation in other, non-Navajo, Athabascans supports our hypothesis that there has been establishment of a new equilibrium for the mutant allele in the western part of the Navajo Nation. As there is no purported reproductive or heterozygote benefit to this ARSA mutation, we postulate that the high frequency of this mutation is the result of genetic bottleneck and possibly a founder effect, at the time of “The Long Walk” in 1864.
This model may explain the high incidence of a number of other unusual heritable disorders found among the Navajo in the western portion of the Navajo Nation. SCID Athabascan type [Li et al., 1998], Navajo neuropathy (OMIM 256810) [Appenzeller et al., 1976; Singleton et al., 1990], Athabascan brainstem dysgenesis (OMIM 601536) [Friedman et al., 1996], and microvillus inclusion disease (OMIM 251850) [Pohl et al., 1999] are found in the western Navajo at extraordinarily high rates (Table II). Each disease appears to be autosomal recessive, without apparent heterozygote advantage, and fatal before reproductive years. Given what we know about Navajo history and population growth, we hypothesize that each illness has become more frequent in the Navajo as a result of a genetic bottleneck at the time of “The Long Walk” in 1864. Presuming each arose from a single “founder” or “founders,” each disease is likely to have a single mutation and ancestral genotype in this population, as has been shown for SCID.
As specific genotypes for heritable diseases among the Navajo are identified, a DNA mutation based screening program could be developed. Screening for Navajo neuropathy, microvillous inclusion disease, or brainstem dysgenesis would not be clinically warranted at this time as no suitable treatment exists. However, a screening program for SCID would be beneficial, as this disease is curable with early bone marrow transplantation. A screening program for MLD may be useful, as bone marrow transplant has shown modest success in ameliorating the progression of MLD if done before clinical signs and symptoms develop [Krivit et al., 1990]. Any such screening program will need to consider traditional Navajo beliefs, and be developed in consultation with tribal leaders.
Finally, this example of heritable illness in the Navajo may be pertinent to other American Indians and Alaskan Natives. It is estimated that at the time of arrival of Europeans to North America the indigenous population was approximately six million [Denevan, 1976]. Three hundred years later, at the end of the 19th century, that number was reduced to 250,000. Many tribal groups were completely eliminated; those remaining suffered population reductions of catastrophic proportions. These population bottlenecks likely created an increased risk for heritable illnesses among current American Indians and Native Alaskans.
Until recently, the risk for heritable illnesses in Native Americans was obscured by geographic isolation and a high burden of infant mortality from infectious diseases. As health conditions improve, it is likely that heritable illnesses will emerge from the shadow of high infant mortality to become more noticeable and more problematic for American Indians and Alaskan Natives. To date, only a handful of heritable illnesses have been identified in Native American tribes other than the Navajo: cystic fibrosis in the Zuni [Kessler et al., 1996]; congenital adrenal hyperplasia in the Eskimo [Speiser et al., 1992]; pyruvate carboxylase deficiency, glutaric aciduria type I, and primary hyperoxaluria type II in the Cree [Haworth et al., 1991]; and scleroderma in the Oklahoma Choctaw [Tan et al., 1998]. It is likely that other heritable illnesses are present but remain undiagnosed in Native Americans. Physicians, and especially geneticists, need to be aware of this risk in American Indians and Alaskan Natives and share information as it develops with tribal leaders and health professionals.
Acknowledgements
The authors acknowledge Andrey Lynn and H. Neil Kirkman for their helpful comments.




