Where hematology meets rheumatology—VEXAS syndrome
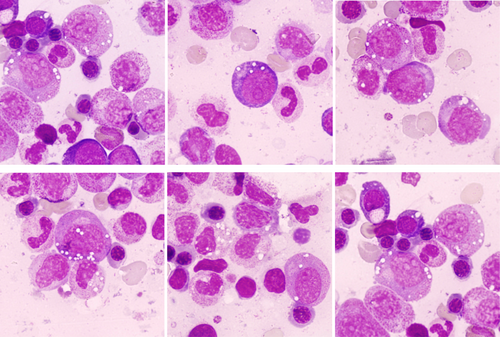
The bone marrow aspirate was cellular with no abnormal infiltration. The myeloid series was prominent and a proportion of promyelocytes and myelocytes showed prominent cytoplasmic (and some apparently intranuclear) vacuolation (all images ×100 objective). There was maturation to neutrophils, with some showing abnormal nuclear segmentation. The erythroid series showed cytoplasmic vacuolation in the earlier stages (top center, top right), with some cells having giant vacuoles (bottom right). These morphological findings in the context of the clinical presentation raised the suspicion of the VEXAS syndrome. Next-generation molecular sequencing confirmed a p.Met41Thr missense mutation in UBA1 (c.122T>C) confirming VEXAS syndrome. A DNMT3A gene splice variant mutation c1429+1G>A was also present. The patient continues on oral prednisolone, and the JAK1/JAK2 inhibitor, barcitinib, and has been referred for consideration for an allogeneic bone marrow transplant.
VEXAS (Vacuoles, E1 enzyme, X-linked, Autoinflammatory Somatic) syndrome is a recently described auto-inflammatory condition driven by a somatic mutation in UBA1 in a hematopoietic progenitor cell.1 Hematological manifestations include cytopenias with clonal evolution, sometimes leading to the development of a myelodysplastic syndrome. There may be macrocytosis and the incidence of venous thromboembolism is increased. The vacuoles are present in both early myeloid and early erythroid precursors in most (but not all) patients with a UBA1 mutation, and may also be present in plasma cells and lymphocytes. A threshold of vacuolization of more than 10% of promyelocytes and myelocytes has been proposed as a sensitive and fairly specific indicator of the condition.2 Vacuolization of bone marrow progenitors is not, however, exclusive to the VEXAS syndrome, and can be seen in other inflammatory disorders, alcoholism, copper deficiency, and malnutrition. Having been only recently defined, the prevalence of the disease is likely underestimated, but the morphological and molecular features should be sought in male patients presenting with both cytopenias and systemic inflammatory disease.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.