Atypical lymphocytosis due to CD8-positive T-cell expansion in unsuspected HIV infection
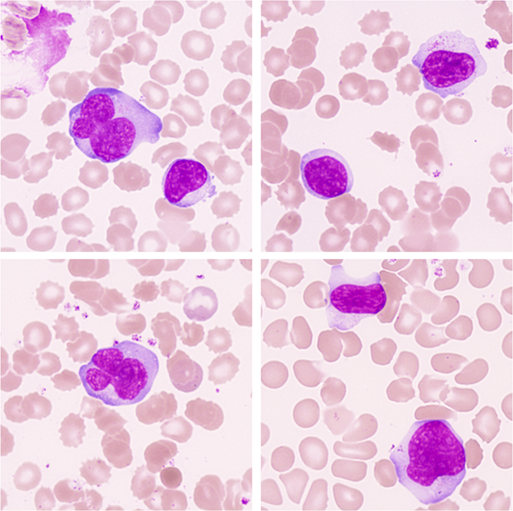
A man in his sixth decade presented to his General Practitioner with a several week history of myalgia and generalized malaise. His blood count was notable for a leukocytosis with a lymphocyte count of 24 × 109/L but was otherwise normal. A peripheral blood film demonstrated smear cells and numerous atypical lymphocytes including medium to large lymphocytes with bilobed or convoluted nuclei, and large granular lymphocytes, some of which were unusually large and also had irregular nuclei; the atypical lymphocytes showed a varying degree of cytoplasmic basophilia, sometimes peripheral (images ×100 objective). Flow cytometric immunophenotyping showed the lymphocytosis to be due to CD8-positive HLA-DR-positive activated T cells, showing partial loss of CD7. On the basis of these findings a virology screen was recommended and was positive for human immunodeficiency virus (HIV) antibody/antigen by a chemiluminescent microparticle immunoassay. The HIV avidity index was less than 40%, which would be consistent with HIV infection acquired within the previous 3–4 months. The HIV RNA viral load at log 6 copies/ml was identified. In addition, IgM and IgG antibodies to cytomegalovirus (CMV) were also detected, indicating recent infection.
It is not possible to be certain in this patient if the atypical lymphocytes were the result of CMV or HIV infection, though co-infection might be synergistic. Advanced HIV infection is characterized by lymphopenia but in the early stages there can be lymphocytosis with an increase in activated CD8-positive T cells. The detection of atypical lymphocytes is an indication for a broad viral screen including not only Epstein–Barr virus but also HIV and CMV and, in some clinical settings, dengue virus. Toxoplasmosis and, in children, pertussis should also be remembered. A detailed clinical history is often not available to laboratory staff, who must remain alert to a wide range of diagnostic possibilities. The detection of HIV infection is of particular importance given the therapeutic and other implications of this diagnosis.
CONFLICT OF INTEREST
The authors declare no conflict of interest.