A myeloid neoplasm with FIP1L1-PDGFRA presenting as acute myeloid leukemia
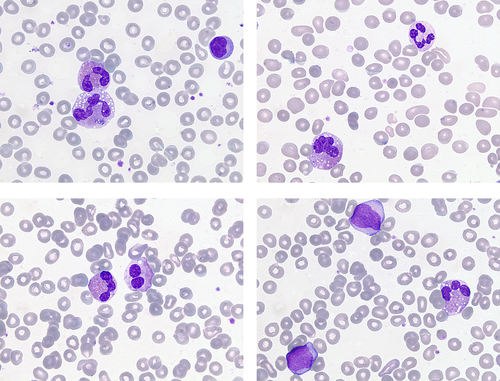
A 30-year-old Spanish woman presented with recurrent respiratory tract infections over several months, together with asthenia, and swelling of the abdomen and legs. On examination, she had hepatosplenomegaly, ascites and edema of both legs. Computed tomography confirmed these observations and, in addition, showed bilateral pleural effusions. Her blood count showed: white cell count 17.45 × 109/L, hemoglobin concentration 96 g/L, mean cell volume 93 fL, and platelet count 99 × 109/L. There was marked eosinophilia (5.2 × 109/L) and mild monocytosis (1.05 × 109/L) with small numbers of granulocyte precursors and 6% blast cells. Eosinophils showed cytological abnormalities including vacuolation, hypogranularity, hypolobation, hyperlobation and basophilic granules in mature eosinophils (images, ×100 objective). Blast cells were medium-sized with a high nucleocytoplasmic ratio and fine azurophilic granules. A bone marrow aspirate showed 25%–30% blast cells and more than 20% eosinophils, these showing similar cytological abnormalities to those in the peripheral blood. Cytogenetic analysis was normal but fluorescence in situ hybridization showed the presence of FIP1L1-PDGFRA. A diagnosis of myeloid neoplasm with PDGFRA rearrangement presenting as acute myeloid leukemia (AML) was made. Subsequent next generation sequencing showed two subclonal mutations in BCORL1 (variant allele frequency 8.4%) and PTPN11 (variant allele frequency 7.4%).
The patient was treated with imatinib in an initial does of 400 mg daily for 2 weeks and then 200 mg daily, without chemotherapy, and entered rapid remission. After 4 months on 200 mg daily of imatinib she is well with a normal blood count.
Because of their sensitivity to tyrosine kinase inhibitors, the identification of neoplasms with rearrangement of PDGFRA or PDGFRB is of considerable importance. Even patients presenting in blast phase can have a complete hematologic and molecular remission that is sustained.1
1 CONFLICT OF INTEREST
Nothing to report.