Large granular lymphocytic leukemia as a cause of pancytopenia
A 79-year-old man was referred with a long-standing pancytopenia: hemoglobin concentration 107 g/L, total white cell count 2.7 × 109/L, and platelet count 71 × 109/L. On clinical examination, there was no lymphadenopathy or splenomegaly. The patient had a past medical history of sepsis in the preceding year, recurrent upper respiratory tract infections and a recent Staphylococcus aureus abscess.
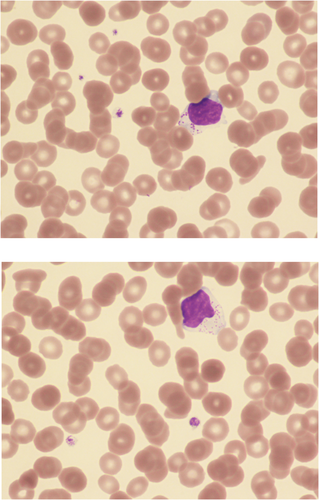
A blood film confirmed the pancytopenia but, in addition, showed an excess of large granular lymphocytes (Images); some of these had reduced chromatin condensation and a minority had cytoplasmic basophilia or an irregularly shaped nucleus. A manual differential count showed neutrophils 1.3 × 109/L and total lymphocytes 0.9 including 0.6 × 109/L large granular lymphocytes.
Clonality studies using PCR showed a broad polyclonal TRB and TRG (T-cell receptor β and γ genes) background. In addition, within the Vγ9 locus, a large peak of ×25 the background was highly suspicious for the presence of a T-cell clone. Immunophenotyping showed expression of CD2, CD7, CD8, CD56, CD57, and T-cell receptor (TCR) αβ. There was no expression of CD3, CD4, CD5, or TCR γδ. A diagnosis of T-cell large granular lymphocytic leukemia (T-LGLL) was made.
This patient had a lower total lymphocyte count than is usual in T-LGLL, but the observation of disproportionate increase in large granular lymphocytes led to the suspicion that this was the cause of the pancytopenia. The clonality studies supported this suspicion. In the six years since initial presentation the patient has been stable with no further infections, and there is not yet an indication for treatment.