Iron deficiency across chronic inflammatory conditions: International expert opinion on definition, diagnosis, and management
Funding information: Vifor Pharma
Abstract
Iron deficiency, even in the absence of anemia, can be debilitating, and exacerbate any underlying chronic disease, leading to increased morbidity and mortality. Iron deficiency is frequently concomitant with chronic inflammatory disease; however, iron deficiency treatment is often overlooked, partially due to the heterogeneity among clinical practice guidelines. In the absence of consistent guidance across chronic heart failure, chronic kidney disease and inflammatory bowel disease, we provide practical recommendations for iron deficiency to treating physicians: definition, diagnosis, and disease-specific diagnostic algorithms. These recommendations should facilitate appropriate diagnosis and treatment of iron deficiency to improve quality of life and clinical outcomes.
“Iron deficiency is very common but often overlooked, especially in people with chronic conditions. Iron deficiency is a health-related condition in which iron availability is insufficient to meet the body's needs and, therefore, its timely detection and treatment is important, because iron is essential to the functioning of all organs”1
1 INTRODUCTION
Managing patients with chronic diseases, particularly those with complex inflammatory disorders, can be challenging. In these patients, a considered multidisciplinary approach needs to be adopted to maintain quality of life (QoL) and improve outcomes.2, 3 One condition that is frequently associated with chronic disease, but often overlooked, is iron deficiency. Iron deficiency is estimated to affect 37–61% of patients with chronic heart failure (CHF), 24–85% of patients with chronic kidney disease (CKD) and 13–90% of patients with inflammatory bowel disease (IBD).4-9 Iron is essential to every cell and, while its fundamental role in oxygen transport through erythropoiesis is well recognized, it is equally critical for energy production and efficient functioning of all of the body's organs.10, 11 In patients with chronic inflammatory conditions, its impact can be particularly severe and may exacerbate the underlying disease state, leading to accelerated clinical deterioration.5, 12
Anemia is the ultimate consequence of iron deficiency in many patients with chronic inflammatory conditions.2, 3, 13, 14 However, the medical field should recognize iron deficiency as a clinical condition distinct from anemia. Recognition is improving owing to our better understanding of the pathophysiological role of iron deficiency (independent of chronic anemia) in symptomatology and clinical outcomes.10, 15, 16 This is further supported by recent clinical observations of an association between the alleviation of morbidity or mortality and the treatment of iron deficiency, even outside the context of anemia.6, 17, 18 However, there is uncertainty among physicians on how to diagnose iron deficiency in patients with chronic inflammatory conditions. This is partially because of symptom overlap with the underlying disease and unclear laboratory diagnostic thresholds. Several publications have also highlighted the problems of recognizing iron deficiency in the context of anemia of inflammation.13, 19-21 This has led to under-diagnosis of an easily treatable condition, leading to anemia, at which point physicians feel more confident about using iron therapy.22
In part, this uncertainty also stems from the heterogeneity of guideline recommendations for the diagnosis and management of iron deficiency in chronic inflammatory diseases. In the absence of any overarching guidance, a series of roundtable discussions were convened to try and bridge this gap. Our objectives were to: (1) provide a definition of iron deficiency; (2) examine the current evidence on (and identify knowledge gaps in the clinical impact of iron deficiency in chronic inflammatory conditions, specifically CHF, CKD, and IBD; and (3) provide practical guidance for the diagnosis of iron deficiency in these patient populations.
1.1 Mechanisms of iron deficiency in chronic inflammation
Iron plays an important role in many physiological processes.15 All aspects of iron homeostasis are tightly controlled and regulation of iron transport is central to this process.10, 23 The hepatic peptide hormone hepcidin and its transmembrane receptor, ferroportin, control the principal routes of iron transport and availability in the body.15 Hepcidin levels are feedback regulated by plasma iron concentration and the amount of iron stores.15 Levels are also negatively regulated by the activity of erythrocyte precursors, the main consumers of iron.15 Hepcidin controls the internalization and degradation of ferroportin, which transfers cellular iron into the plasma and is predominantly expressed in key iron exporters (eg, enterocytes and iron-recycling macrophages).10, 16
Hepcidin, and therefore the regulation of ferroportin, is affected by inflammation (Figure 1).15, 24, 25 In inflammatory conditions, hepcidin production and release is induced by circulating proinflammatory cytokines, especially interleukin-6. This results in increased internalization and degradation of ferroportin and subsequent cellular iron retention. This ultimately leads to decreased levels of circulating iron, which may result in insufficient iron availability to meet the body's needs.10, 15, 16
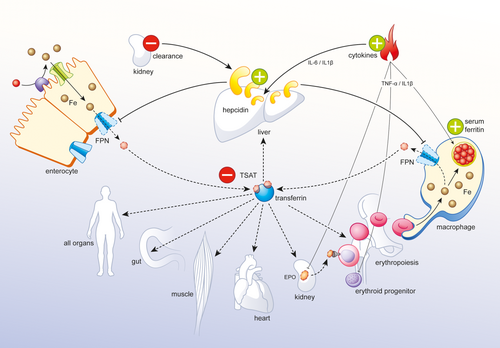
The pathophysiology of iron deficiency in chronic inflammation. Increased cytokine levels in all conditions, and decreased renal clearance in CKD and CHF, result in enhanced hepcidin levels. High hepcidin levels bind, internalize and degrade ferroportin on the lateral membrane of duodenal enterocytes and spleen macrophages. Iron remains trapped in enterocytes, which are then shed in the gut. Iron is also sequestered into macrophages, which are responsible for destroying senescent red blood cells and recycling their iron. Serum ferritin levels are regulated by the iron content of macrophages and increase in inflammation (apoferritin as an acute-phase protein). A decrease in circulating iron leads to lower amounts of iron bound to the iron carrier protein, transferrin, and subsequently to a decline in transferrin saturation and low iron supply to all organs. Furthermore, cytokines may also have negative effects on erythropoietin production in the kidney and erythroid cell maturation, while also increasing macrophage iron retention. Note that the increased iron losses that can occur in specific chronic inflammatory conditions are not illustrated here. Plus and minus signs represent increase/enhancement and decrease, respectively. EPO, erythropoietin; FPN, ferroportin; IL, interleukin; TNF, tumor necrosis factor; TSAT, transferrin saturation
It is estimated that for the healthy individual, total body iron content is ∼3–4 g, of which 1–2 mg of exogenous iron is absorbed per day and 25 mg of iron is required daily for erythropoiesis, mostly obtained from iron recycling.26 As a result of limited iron supply from macrophage-led iron retention, patients with chronic inflammatory conditions have greater daily iron requirements to increase the levels of circulating iron compared with healthy individuals.27-29 As a consequence of severely depleted iron availability, proper functioning of many organ systems is compromised in these patients.27-29 For example, iron content and transferrin receptor levels were decreased in the myocardium of patients with iron deficiency anemia and advanced heart failure compared with healthy individuals, suggesting that iron depletion was associated with adverse outcomes in these patients.30
1.2 Defining iron deficiency
Based on our literature review, it is evident that iron deficiency is not fully recognized as a disorder distinct from iron deficiency anemia, or as one that may have its own clinical consequences. Indeed, the terms “iron deficiency” and “iron deficiency anemia” are often used interchangeably.31 Where iron deficiency is discussed, it is frequently perceived as the most common nutritional disorder worldwide,31-33 but not as a medical condition in and of itself.34
It is clear that the heterogeneity in how iron deficiency is defined is a knowledge gap that is compounding physicians' lack of confidence in recognizing and diagnosing this condition. The lack of a standard simple definition for iron deficiency hinders its uncoupling from iron deficiency anemia and its acceptance as a standalone medical condition with distinct clinical implications.
1.3 Expert recommendation
Iron deficiency is a health-related condition in which iron availability is insufficient to meet the body's needs and which can be present with or without anemia
1.4 Clinical impact of iron deficiency
Iron deficiency may contribute to several symptoms that can manifest even in the absence of progression to anemia. Although there are symptoms that are likely to be caused by iron deficiency (eg, pagophagia, and RLS), many symptoms are nonspecific, such as fatigue, and exhaustion.35-38 This means that physicians and patients do not always recognize that iron deficiency is present and, as a consequence, diagnosis is not pursued and the condition is left untreated.
Physicians may need to actively ask their patients about such symptoms, especially for those patient populations where iron deficiency is highly prevalent, so that appropriate diagnostic tests can be performed and, if necessary, treatment can be given.35 In this section, we outline the iron deficiency symptoms that have been commonly reported in patients with CHF, CKD and IBD, as well as its associated clinical outcomes that further call for its prompt diagnosis and management.
1.5 Iron deficiency in chronic heart failure
Iron deficiency is estimated to affect between 37 and 61% of patients living with CHF, and its prevalence increases as CHF advances.5-7, 9 The etiology of iron deficiency in CHF is not fully understood, but it is thought to be multifactorial and arising from: a general loss of appetite and poor nutrition; decreased gastrointestinal (GI) iron absorption due to edema; increased GI blood loss that may occur partially as a result of antiplatelet and anticoagulant drugs; and, importantly, as a consequence of the chronic inflammatory state of these patients.28, 39 The diagnosis of iron deficiency in CHF is complicated by the fact that the key manifestations of CHF (fatigue, exercise intolerance) are the same as those of iron deficiency. Fatigue is frequently associated with iron deficiency in CHF patients and linked with reduced exercise and work capacity.40-43 In a recent study using the 6-min walk test (6MWT), exercise-induced symptoms were significantly more frequent in iron-deficient CHF patients (35%) compared with non-iron-deficient patients (27%; P = 0.028); the most commonly reported symptom was fatigue.44
In CHF, iron deficiency has been shown to adversely impact exercise capacity and QoL independently of anemia. Iron deficiency significantly reduces exercise tolerance as measured by the 6MWT.17, 44-46 In the FAIR-HF study, iron-deficient CHF patients who were treated for iron deficiency with intravenous (IV) iron, ferric carboxymaltose, had significant improvements in the 6MWT (P < 0.001 at weeks 4, 12, and 24) compared with those receiving placebo.45 These findings are supported in the recent EFFECT-HF study, whereby treatment with ferric carboxymaltose led to significant improvement in exercise capacity in iron-deficient CHF patients compared with other standard treatments other than IV iron.47 In a secondary analysis, the same patients experienced significantly increased QoL as measured by the Kansas City Cardiomyopathy questionnaire (P < 0.001).45 Studies demonstrated that QoL was significantly affected by iron deficiency in patients with CHF, whether assessed using the European Quality of Life-5D, Kansas City Cardiomyopathy or the Minnesota Living with Heart Failure questionnaires.17, 48, 49
Iron deficiency can also negatively impact outcomes in CHF. The increased risk of mortality from iron deficiency in studies evaluating CHF patients ranges between 40 and 60%.5-7 Iron deficiency in CHF has also been associated with increased hospitalizations, with one study showing that the risk of hospitalization doubled in patients who were not treated for iron deficiency compared with those who were (relative risk [RR] 2.23, 95% confidence interval [CI] 1.59–3.42, P < 0.01).50 This is further supported by the CONFIRM-HF study, where treatment of iron deficiency with ferric carboxymaltose was associated with a significant reduction in hospitalizations (hazard ratio [HR] 0.39, 95% CI 0.19–0.82, P = 0.009).46
Notably, the benefit of treating iron deficiency in this setting occurs whether or not patients are also anemic, thus establishing iron deficiency as an independent therapeutic target in CHF.51, 52 This has led to compulsory iron deficiency screenings in patients with CHF and treatment with IV iron (eg, ferric carboxymaltose) has been recommended.
1.6 Iron deficiency in chronic kidney disease
The prevalence of iron deficiency in patients with CKD has been reported as ranging from 24 to 85% and, as for CHF, the prevalence increases as CKD progresses.4, 8 Similar to CHF, iron deficiency in CKD can arise from decreased GI iron absorption, malnutrition and blood loss, which is worsened by chronic inflammation.29 Blood loss in CKD patients can originate from ongoing assessment tests and treatments such as dialysis. Additionally, iron utilization is promoted during the use of erythropoiesis-stimulating agents (ESAs). ESA therapy, while effective in correcting anemia, can further exacerbate iron deficiency, which in turn may result in poor response to ESAs.53-56 Unlike cardiologists, nephrologists do not recognize iron deficiency, which is easily treatable, as a distinct entity and still aim to treat iron deficiency in the context of anemia management. Thus, in contrast to CHF, where there is strong evidence that iron deficiency alone impacts the underlying disease, the evidence in CKD is almost non-existent and focuses only on anemia, of which iron deficiency is a major cause.
Anemia in CKD is frequently associated with reduced QoL,57 particularly in physical domains such as vitality and energy.58 Similar to CHF, these physical domains appear to play a major role in patient QoL. This is supported by data demonstrating that normalization of hemoglobin (Hb) levels is associated with significant improvements in physical function (SF-36 scores; P < 0.001).56
At present, the major importance of iron deficiency in CKD is its role in the development of chronic anemia, which is easily correctable. Anemia in CKD is associated with an increased risk of morbidity and mortality.59, 60 In non-dialysis CKD patients, lower time-averaged Hb levels correlated with a significantly increased risk of predialysis mortality and end-stage renal disease (HR [95% CI] of Hb <11, 11–12 and 12–13 g dL−1: 2.57 [1.85–3.58], 1.97 [1.45–2.66], and 1.19 [0.86–1.63]; all vs. Hb >13 g dL−1, Ptrend < 0.001).59 In a 5-year observational study, anemia in CKD patients was again associated with increased mortality, regardless of CKD severity.61 The change from baseline to follow-up in the prevalence of anemia was much higher in patients with CKD stage 2 and 3 who died (stage 2: 42.1%; stage 3: 42.2%) compared with those who were alive (stage 2: 24%; stage 3: 28.3%) at the end of observation.61 Notably, one study demonstrated that ESA treatment for the correction of anemia in patients with type 2 diabetes and CKD had significant safety concerns, (eg, stroke).62 Moreover, no overall cardiovascular, renal or QoL benefits were observed when targeting higher Hb levels compared with the placebo group, who received only iron.62 This further supports the point of treating iron deficiency prior to anemia development and requirement for ESAs.
Anemia in CKD patients is often associated with cardiovascular morbidities and can result in increased hospitalization (HR 2.18, CI 1.76–2.70),63 leading to cardio–renal–anemia syndrome. While this overlap between CKD and CHF populations is recognized, the nature of cardiac disease may differ between these groups. As there are differences in the nature of the heart failure, the consequences and treatment of iron deficiency may also differ.
1.7 Iron deficiency in inflammatory bowel disease
Iron deficiency affects between 13 and 90% of patients with IBD, depending on the population that is studied, eg, in- or outpatients, active or quiescent, as well as severity of the disease.4 The main causes of iron deficiency in IBD arise from impaired GI iron absorption due to chronic inflammation, bowel resection (especially in Crohn's disease), disease triggered malnutrition and (mainly chronic) blood loss.27 As with nephrologists, not all gastroenterologists fully appreciate the importance of managing iron deficiency. This may be because the role of iron deficiency anemia in IBD is not fully understood—evidence often depends on the selected patients from tertiary referral centers, including: Crohn's disease and ulcerative colitis; hospitalized patients versus outpatients; or patients with and without surgical interventions.27, 64 Iron deficiency can be easily corrected before the onset of anemia; however, the current evidence base focuses on iron deficiency anemia and its treatment.22
Iron deficiency anemia is recognized as one of the most common complications and extra-intestinal manifestations of IBD. However, over 50% of patients who are diagnosed with iron deficiency anemia are not treated.65 In a recent survey, it was shown that approximately one-third of patients diagnosed with IBD, who are unsure of their anemia status, do not discuss the possibility of developing iron deficiency anemia with healthcare professionals.22 In this same survey, patients attributed weakness and chronic fatigue to both IBD and iron deficiency anemia.22 Chronic fatigue associated with iron deficiency anemia may be debilitating and has been suggested to be the primary cause of impaired QoL in anemic IBD patients, to the same extent as other symptoms such as abdominal pain and diarrhea.22, 27, 66 Notably, improvements in iron status with IV iron treatment have led to significantly improved QoL in patients with ulcerative colitis and Crohn's disease, according to IBD QoL questionnaire scores (P < 0.001) and SF-36 physical (P < 0.001) and mental component (P = 0.024) scores.18 Furthermore, changes in Hb levels (but not the activity of the underlying disease) were associated with significant changes in SF-36 (P = 0.005) and IBD QoL questionnaire (P = 0.009) scores in IBD patients with iron deficiency anemia.67
1.8 Diagnosis of iron deficiency in chronic inflammatory conditions
Our review of international guidelines available for CHF, CKD and IBD reveals no consensus practical guidance for diagnosing iron deficiency independent of anemia (Table 1). However, only some guidelines recognize iron deficiency as a standalone condition—whether this is through lack of awareness of iron deficiency or an intentional omission is difficult to establish (Table 1). Iron deficiency can be simply diagnosed with routinely available blood tests measuring serum ferritin and transferrin saturation (TSAT).86 yet guidelines often lack agreement on test cut-off values for these parameters.4 Serum ferritin levels are sensitive to inflammation and some guidelines recommend assessment of chronic inflammation (according to inflammatory markers such as C-reactive protein [CRP] and erythrocyte sedimentation rate); however, there is little consensus for many conditions on when this should be measured, should it be standard practice for all patients or measured only when serum ferritin is >30 µg L−1 or if patients are symptomatic68, 87? Moreover, no standard CRP cut-off values are provided; although a CRP level of 5 mg L−1 is the most common threshold,64 this is not recognized in most guidelines68
| Recommended iron deficiency threshold values independent of anemia | |||||
|---|---|---|---|---|---|
| Professional association | Year | ID/IDAa | Serum ferritin (µg L−1) | TSAT (%) | Additional tests |
| Chronic heart failure | |||||
| ACCF/AHA | 2017 | ID and IDA | <100 or 100–300 | – and <20 | – |
| Canadian Cardiovascular Society | 2014 | IDA only | – | – | – |
| European Society of Cardiology | 2016 | ID and IDA | <100 or 100–299 | – and <20 | – |
| French cardiologists | 2014 | ID | AID <100; FID 100–299 | – and <20 | – |
| German commentary for European Society of Cardiology | 2013 | ID | <100 or 100–299 | – and <20 | – |
| National Heart Foundation of Australia and Cardiac Society of Australia and NZ | 2011 | ID | No threshold recommended | No threshold recommended | – |
| Spanish Society of Cardiology and Spanish Society of Internal Medicine | 2017 | ID | <100 | or <20 | If patients have SF <100 µg L−1 but TSAT >20%, test for sTfr |
| Chronic kidney diseaseb | |||||
| Canadian Society of Nephrology | 2008 | IDA only | – | – | – |
| ERBP | 2013 | ID and IDA | AID <100 | and <20 | – |
| KDIGO | 2012 | IDA only | – | – | – |
| KDOQI | 2012 | IDA only | – | – | – |
| KHA-CARIc | 2013 | ID | <100; <200–500 | <20; <20–30 | |
| NCGC | 2015 | IDA only | – | – | – |
| UK NICE | 2015 | IDA only | – | – | – |
| UK Renal Association | 2012 | IDA only | – | – | – |
| Inflammatory bowel disease | |||||
| Quiescent IBD | |||||
| ECCO | 2015 | ID and IDA | <30 | – | – |
| Portuguese Working Group on IBD | 2016 | ID and IDA | <30 | and <16 | CRP assessments |
| Active inflammatory bowel disease | |||||
| British Society of Gastroenterology | 2011 | ID and IDA | <50d | – | – |
| ECCO | 2015 | ID and IDA | <100 | – | – |
| Portuguese Working Group on IBD | 2016 | ID and IDA | 30–100 | and <16 | CRP assessments |
- a Guidelines that only report diagnosis thresholds specific to IDA have been described as ‘IDA only’.
- b Includes both haemodialysis and non-dialysis chronic kidney disease.
- c These threshold values are based on target ranges for the treatment of iron deficiency.
- d Possibly more, depending on degree of inflammation. ACCF, American College of Cardiology Foundation; AHA, American Heart Association; AID, absolute iron deficiency; CRP, C-reactive protein; ECCO, European Crohn's and Colitis Organisation; ERBP, European Renal Best Practice; FID, functional iron deficiency; IBD, inflammatory bowel disease; ID, iron deficiency; IDA, iron deficiency anemia; KDIGO, Kidney Disease Improving Global Outcomes; KDOQI, Kidney Disease Outcomes Quality Initiative; KHA-CARI, Kidney Health Australia—Caring for Australasians with Renal Impairment; NCGC, National Clinical Guideline Centre; NICE, National Institute for Health and Care Excellence; NZ, New Zealand; SF, serum ferritin; sTfr, soluble transferrin receptor; TSAT, transferrin saturation.
1.9 Expert recommendation
Serum ferritin <100 µg L−1 or TSAT <20%
If serum ferritin is between 100 and 300 µg L−1, a TSAT test will be required to confirm iron deficiency
Furthermore, we also propose the following algorithms for the diagnostic workup of iron deficiency in patients with CHF, CKD, and IBD (Figures 2-4). In all conditions, initial workup should incorporate assessment of serum ferritin and TSAT, as well as Hb levels, in order to distinguish between those with normal hematological parameters, those with some form of iron deficiency (iron deficiency: normal Hb and low iron; or iron deficiency anemia: low Hb and low iron), and those with some other form of anemia (where iron levels are normal but Hb is low). In CKD, we must also consider whether the patient is receiving dialysis (Figure 3A,B). Finally, in IBD, we must further consider whether the underlying condition is in remission or active. For IBD, we therefore also recommend measuring CRP levels or stool markers such as calprotectin or lactoferrin at the time of iron markers and hematological workup, in order to appropriately manage iron deficiency in relation to these results. We recommend a CRP threshold of 5 mg L−1 to determine the IBD disease activity. Although laboratory markers are usually sufficient with clinical disease activity markers, other indicators of intestinal inflammation, such as transabdominal ultrasound or endoscopy, may also be used to supplement these assessments.
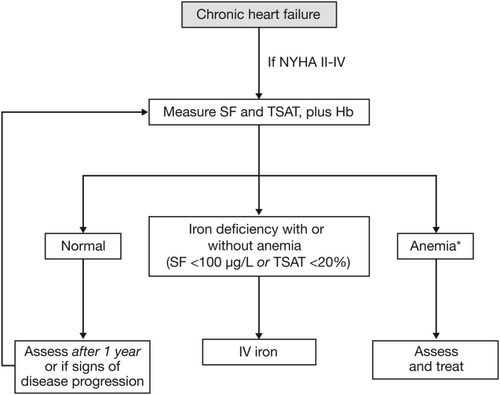
Diagnostic algorithm: iron deficiency in chronic heart failure. *Look for other causes of anemia and treat accordingly. Hb, haemoglobin; IV, intravenous; NYHA, New York Heart Association; SF, serum ferritin; TSAT, transferrin saturation
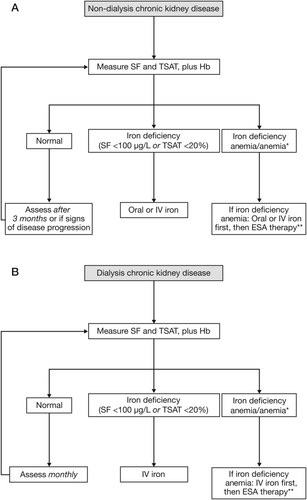
Diagnostic algorithms: iron deficiency in (A) non-dialysis and (B) dialysis chronic kidney disease. *If iron stores are normal but Hb is low, look for other causes of anemia and treat accordingly. **When prescribing ESA therapy, iron should always be administered. ESA, erythropoiesis-stimulating agent; Hb, haemoglobin; IV, intravenous; SF, serum ferritin; TSAT, transferrin saturation
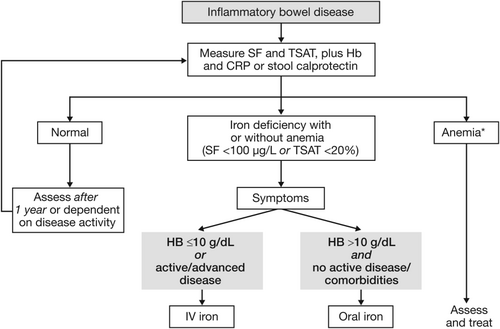
Diagnostic algorithm: iron deficiency in inflammatory bowel disease. *Look for other causes of anemia and treat accordingly. CRP, C-reactive protein; Hb, haemoglobin; IV, intravenous; SF, serum ferritin; TSAT, transferrin saturation
1.10 Iron deficiency in high-risk populations with chronic inflammatory conditions
Chronic conditions cannot be viewed in isolation and there will be circumstances where individuals may have further increased susceptibility to iron deficiency. To optimize outcomes for these patients, risks need to be pre-empted wherever possible. Three important populations to consider among your patients are: women (particularly those who are pregnant or are planning to become pregnant, and those who suffer from heavy menstrual bleeding [HMB]); the elderly; and those undergoing surgery.
Women of reproductive age are one of the most at-risk population groups for iron deficiency anemia. Between 4 and 52% of women of reproductive age are reported to suffer from HMB, with a wide range reflecting disparities between study populations and how HMB is defined88 Notably, a recent European study demonstrated that 63% of the participating HMB patients were suffering from iron deficiency or iron deficiency anemia.89 Iron deficiency in combination with HMB can have debilitating consequences on the QoL and wellbeing of the sufferer.90-93 Thus, many of these women enter pregnancy with low iron stores and are often already anemic. Approximately 42% of pregnant women worldwide have anemia, with iron deficiency anemia being the primary cause, and this may have a serious detrimental effect on the outcome for both mother and child.2, 94-96 In pregnancy, iron deficiency anemia is associated with increased maternal morbidity and mortality, possibly due to not being able to withstand the adverse effect of excessive blood loss at delivery and the increased risk of infection.96 Iron deficiency anemia also affects the child and has been linked with increased risk of preterm labor and subsequent low birthweight, and perinatal complications.97 Moreover, there is an association between maternal iron status in pregnancy with that of the infant; with infants born to anemic mothers being more likely to be anemic themselves.98 Iron deficiency also carries negative long-term impact on the mother–child relationship and the child's cognitive development, of which the latter has shown to persist for up to 10 years, even after iron repletion.95, 99, 100
Extra vigilance should also be taken when managing elderly patients. The prevalence of iron deficiency increases rapidly with age, and timely diagnosis and treatment of iron deficiency will substantially improve outcomes and QoL for a population prone to multiple comorbidities.101, 102 Where surgery is required for your IBD patients, regardless of age, the impact of iron deficiency during procedures that have the potential to result in major blood loss has to be recognized early and proactively managed. An awareness of the substantial impact of pre-operative iron deficiency with and without anemia on morbidity and mortality is increasing, with growing recognition that patient blood management procedures need to be established across all surgical specialties.103-105
1.11 Management of iron deficiency in chronic inflammatory conditions
Treatment options for iron deficiency fall into two broad categories, oral and IV iron preparations. There are advantages and limitations for each (Table 2) and physicians must decide on the most suitable option on a patient-by-patient basis. Factors that should be considered are: the inflammatory condition of the patient; the degree of iron deficit (ie, the total amount of iron to be replenished); and the time frame that is available or acceptable to achieve adequate iron stores.
| Oral iron | IV iron | |
|---|---|---|
| General benefits |
• Ease of use • Lower costs compared with IV iron |
• More efficient and faster than oral iron at increasing iron availability and Hb levels • Effective in the presence of inflammation • Fewer GI side effects than oral iron • Few administrations required to reach target serum ferritin, TSAT and Hb (compared with daily intake of oral iron) • IV administration ensures treatment adherence |
| General limitations |
• Low intestinal absorption of iron (10–20%) • Low absorption results in slow and limited efficacy • Requires daily intake of up to three equally spaced doses • Decreased iron absorption in inflammatory conditions • Unfavorable (GI) adverse-event profile • Low adherence to treatment • Accidental iron overdose with ferrous salts (eg, ferrous sulfate)a |
• Requires medical expertise for administration and facilities for cardiopulmonary resuscitation • Potential fatal hypersensitivity may occur • Side effects at injection site may occur • More expensive than oral iron • Complex stability varies between preparations; less stable complexes release larger amounts of weakly bound iron in the blood and can induce oxidative stress if given in high doses |
- a The US Food and Drug Administration has issued a black box warning.
- GI, gastrointestinal; Hb, hemoglobin; IV, intravenous; TSAT, transferrin saturation.
Oral iron treatments are the most widely used, largely because of convenience, but there are a number of limitations that impact their effectiveness in patients with chronic inflammatory conditions (Table 2). Oral iron absorption from the ingested amount is low (on average 10%) and even in iron-deficient conditions, upregulation of absorption may be limited.106 During active inflammation, absorption is further reduced as a result of hepcidin-mediated ferroportin inhibition.15 Thus, oral iron supplementation may fail to supply sufficient amounts of iron in chronic inflammatory conditions. Recent evidence from the IRONOUT study further supports the ineffectiveness of oral iron in the chronic disease setting. In this study, no improvement in exercise tolerance or iron stores was demonstrated with oral iron treatment in iron-deficient patients with CHF.112 In the CKD setting, the proportion of anemic patients achieving Hb increase of ≥1 g dL−1 at any time was significantly reduced in the oral iron group compared with the IV iron group (P < 0.001).113 Moreover, oral iron treatment has recently been associated with significant changes in the normal gut microbiota, adding to our understanding of how oral iron causes its well-known GI tolerability profile, which is particularly detrimental to IBD patients.114
The alternative solution, IV iron treatment, can deliver a larger iron supply, effectively replenishing iron stores more rapidly than oral iron and, because of the route of administration, bypassing the risk of GI side effects. Many guidelines acknowledge the benefits of IV iron preparations as a valuable option for patients with chronic inflammatory diseases who lack a response to, are non-compliant with, or are intolerant of oral iron treatment, as well as those who have severe iron deficiency and require rapid replenishment of available iron and Hb levels. However, multiple IV iron preparations are available for which the dosing, infusion times, efficacy and safety profiles can vary. While some products have very little data published demonstrating their benefit-to-risk profile, for other IV iron preparations, such as ferric carboxymaltose, there is a wealth of clinical evidence, including studies in all three chronic inflammatory conditions within the scope of this review; there is a growing evidence base supporting its effectiveness and good tolerability across patient groups.32, 115-117
2 CONCLUSIONS
Iron deficiency is a very common but often overlooked condition, especially in patients with chronic inflammatory conditions. It is a highly relevant comorbidity and accounts for poor outcomes, prolonged hospitalization and poor QoL in this patient population. Here, we have proposed several practical recommendations for the definition and diagnosis of iron deficiency in CHF, CKD and IBD. Based on this definition and diagnosis threshold, simple diagnostic algorithms and management for these conditions have been discussed. The intention of these recommendations is to provide consensus expert opinion where there is variability in the guidelines or gaps in the current evidence base.
ACKNOWLEDGMENTS
This study was sponsored by Vifor Pharma. Medical writing support was provided by Mai Kurihara, PhD, from Mudskipper Business Ltd, funded by Vifor Pharma.
CONFLICTS OF INTEREST
All IRON CORE members have received honoraria as advisors from Vifor Pharma. WD has also received a grant from Vifor Pharma.