Iatrogenic lymphoproliferative disorder
Conflict of interest: Nothing to report
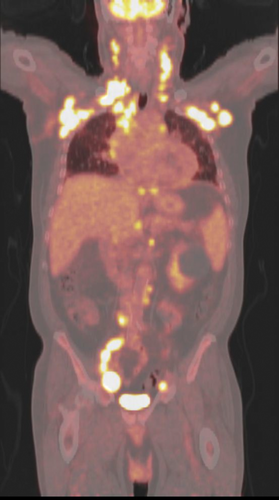
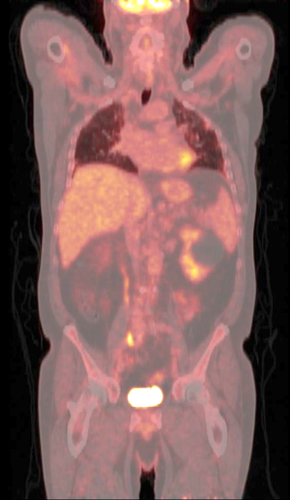
A 69-year-old male with rheumatoid arthritis, on methotrexate and plaquenil, presented with palpable right axillary lymphadenopathy. This was associated with progressive dyspnea, weight loss, and night-sweats for one-month duration. On examination, there was a 2 × 2 cm nontender lymph node on the right axillary. Positron emission tomography-computed tomography (PET-CT) illustrated diffuse hypermetabolic lymphadenopathy with moderate pericardial effusion (Image 1). Patient had a right axillary excisional biopsy that confirmed Diffuse Large B-Cell Lymphoma, which positively stained for Epstein–Barr virus encoded RNA (EBER) on in-situ-hybridization. Bone marrow biopsy was normal. A diagnosis of IIIB other iatrogenic immunodeficiency associated lymphoproliferative disorder (OIIA-LPD) was given and decided to hold methotrexate. After 6 weeks of withdrawal, the symptoms resolved along with his lymphadenopathy on PET-CT (Image 2). Patients with rheumatoid arthritis have a risk of developing LPDs with or without methotrexate. However, further immunosuppression with methotrexate and reactivation of Epstein–Barr virus is postulated to be a possible culprit in lymphomagenesis, given that withdrawal of methotrexate correlates with regression of disease in many cases 1-7. Patient currently remains in complete remission.