Developing an electronic health record–derived health equity dashboard to improve learner access to data and metrics
Supervising Editor: Alden Landry, MD, MPH.
Funding information
CMF has received research support unrelated to this work from the National Heart, Lung, and Blood Institute (1K12HL133304).
Abstract
Objectives
It is essential to engage learners in efforts aimed at dismantling racism and other contributors to health care disparities. Barriers to their involvement include limited access to data. The objective of our study was to create a data dashboard using an existing quality improvement (QI) infrastructure and provide resident access to data to facilitate exploratory analysis on disparities in emergency department (ED) patient care.
Methods
Focusing on patient populations that have previously been shown in the literature to suffer significant disparities in the ED, we extracted outcomes across a variety of metrics already collected as part of routine ED operations. Using data visualization software, we developed an interactive dashboard for visual exploratory analyses.
Results
We designed a dashboard for our resident learners with views that are flexible and allow user selected filters to view clinical outcomes by patient age, treatment area, and chief complaint. Learners were also allowed to select grouping and outcomes of interest to investigate questions and form new hypotheses of their choosing. Available dashboard views included summary counts view to assess ED visits over time by selectable group, a rooming and triage acuity view, time-to-event survival curve view, histogram and box plot views for continuous variables, a view to assess outcome variables by time of day of ED arrival, customizable contingency table views, and correspondence analysis.
Conclusions
Utilizing an existing QI infrastructure, we developed a dashboard that provides a new perspective into commonly collected ED operations data to allow for the exploration of disparities in ED care that is accessible to learners. Future directions include using these data to refine hypotheses on ED disparities, understand root causes, develop interventions, and measure their impact.
INTRODUCTION
Learners play a critical role in patient care yet their opportunities to engage in eliminating health care disparities remains limited.1 The Accreditation Council for Graduate Medical Education (ACGME) has formed a working group, the Quality Improvement in Health Care Disparities Collaborative,2 to guide development of programs to empower learners to systematically engage in reducing health care disparities. Racism, in the form of health care disparities in emergency department (ED) care, exist in outcomes related to administration of pain medications,3 management of acute coronary syndrome,4 and access to specialists.5 These studies have drawn much needed attention to examining differences in health care delivery, but implementation of interventions based on these findings remains limited.6 The effectiveness of implicit bias training and other educational interventions to reduce systemic racism in physician behavior have mixed efficacy.7 Incorporating novel approaches to allow assessment of provider actions in real time will be essential to informing interventions to eliminate these disparities.8
While it is common for EDs to provide individual or departmental feedback regarding metrics on disposition, length of stay, patient satisfaction, and other aspects of care, these data are rarely stratified by groups that have the potential to be marginalized in their care. These patient groupings include race, ethnicity, sexual orientation, gender identity, language, religion, age, and weight. Dashboards have emerged within health care as a visual tool to monitor data for continuous quality improvement (QI) and to detect variations in care. However, these data are generally unavailable to learners and audiences are limited to hospital staff in clinical and financial operations. The COVID-19 pandemic has driven a dramatic expansion in the number of dashboards presented to health care workers outside of operations.9 We sought to adapt this philosophy of data transparency and real-time monitoring to improve the equity of care delivered in our ED. Thus, we developed a data dashboard utilizing variables selected from existing quality metrics and applied exploratory analyses to these data to identify health care disparities that are specific to our institution and patient population. The goal was to develop a learner-accessible dashboard and facilitate a collection of relevant variables that would allow for data exploration, generation of new hypotheses, and evaluation of interventions.
METHODS
Group selection
We identified groups previously shown to suffer disparities in outcomes of their care in the ED. Groups included patients of varying race, ethnicity, sexual orientation, gender identity, language, religion, age, and weight. These data were collected routinely at registration during either the ED encounter or prior encounters and stored in the electronic health record (EHR).
Outcome variable selection
Our department's data analytics group collects a variety of metrics concerning clinical operations. These quality metrics are similar to those commonly monitored other EDs and include information on wait and rooming times, provider action times, dispositions, administration of pain medications, use of laboratory testing, use of imaging, and triage information.10 A subset of these variables was selected for use in the dashboard.
Dashboard design
All selected variables were collected and stored securely in our institution's health information data warehouse. We utilized Tableau data visualization software to develop the interactive dashboard. Learners were provided the ability to select groups and outcomes to explore trends over time, by chief complaint, primary diagnosis, and a variety of other factors. Dashboard creation and data collection were deemed exempt QA activities by our hospital's institutional review board and access is via secure login similar to the EHR.
RESULTS
Selected outcome variables
Outcome variables were a subset of commonly available ED operations metrics and broadly grouped into four domains. First, we identified triage-related variables including time to events such as time to room and first provider contact, triage note text, and triage acuity level. We also identified outcomes in diagnostic testing such as utilization of specific and total laboratory tests, type and number of imaging studies, and use of specialist consultants. Pain and antiemetic medication usage was also identified as a domain of interest and variables included type, route, and timing of administration for a predefined list of pain and antiemetic medications. Finally, disposition-related metrics including ED and hospital length of stay, disposition type, time to disposition decision, ED return, and unplanned ICU transfers were collected.
Dashboard-based exploratory analyses
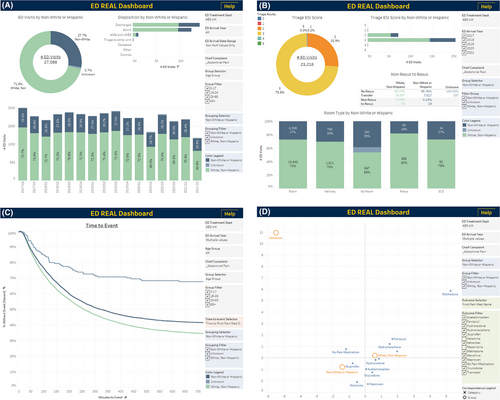
We designed the dashboard views to be flexible and allow user selection of filters to narrow analysis to a specific population of interest by date of presentation, age, treatment area (adult or pediatric ED), and chief complaint. Learners were allowed to select grouping and outcomes of interest to investigate questions of their choosing in a variety of dashboard views that included total ED visits over time by selectable group, rooming and triage acuity trends, time-to-event survival curves, histogram and box plot views for continuous variables, assessment of outcome variables by time of day of ED arrival, contingency tables, and correspondence analysis.11 Figure 1 presents an example dashboard-based, exploratory analysis of pain medication administration in patients presenting with abdominal pain stratified by race and ethnicity as White, non-Hispanic, non-White or Hispanic, and unknown race/ethnicity patients. Summary counts and percentage data indicate relatively stable ED census and percentage of patients who are non-White or Hispanic (Figure 1A). Time-to-event analysis demonstrated that within the population of abdominal pain patients, there was generally a longer time to administration of the first pain medication in non-White or Hispanic patients (Figure 1B). Final pain score was also assessed, and higher final pain scores were found in non-White or Hispanic patients (Figure 1C). Correspondence analysis demonstrated association between nonopioid medications and non-White or Hispanic patients (Figure 1D). These analyses were considered example exploratory analyses, and formal statistical testing was not performed.
DISCUSSION
We have developed a dashboard for the exploration of common ED metrics stratified by groups historically known to have disparities in care. By utilizing our own department's data, we hope to increase awareness and empower learners to pursue QI interventions that seek to reduce inequality and bias in the care of our patients. Potential interventions could include personalized and aggregate data derived from the dashboard. For example, use of individual provider data to facilitate personal coaching sessions regarding implicit bias could mitigate identity threat as a barrier to meaningful behavior change. Specifically, these data could be used to provide trainees with iterative and formative feedback congruent with the ACGME’s Milestones 2.0 under system-based practice, practice-based learning and improvement, and interpersonal and communication skills. Alternatively, dashboard monitoring could be used to support an ongoing dialogue regarding local issues of health care disparities and support active change management when resistance to continued action is encountered. Based on our experience with a resident-initiated lecture series on health care disparities, example topics amenable to such analysis include differences in care due to primary language, race and pain medication delivery, and rural heath disparities.
Our dashboard leverages the existing data infrastructure in our ED and similar techniques could be applied easily scaled both with and across at other institutions to minimize the costs to training programs or EDs that seek to implement similar dashboards. Partnership with departmental leadership facilitates a meaningful cross-disciplinary conversation with clinical operations staff. While we utilized Tableau software to create our dashboard; similar, less costly tools are available. Preconfigured reporting tools may also be available directly in the EHR. For example, Epic (Epic Systems) includes the SlicerDicer reporting tool that can be applied to the analysis of health care disparities.
Dashboard monitoring promotes continuous QI and can facilitate access to data for learners and educators. The ability to interact with departmental data, particularly one's own data, may provide learners the opportunity to further investigate their observational hypotheses. Congruent with the ACGME’s Quality Improvement in Health Care Disparities Collaborative, access to departmental health disparities data is an important foundational resource for learners to engage in projects aimed at eliminating health care disparities. We anticipate that this will help overcome one of the barriers that limit learners’ participation in QI projects. By reducing these barriers, learners can more easily identify potential interventions within their clinical environment.
LIMITATIONS
While our dashboard allows for data monitoring and exploratory visual analysis, statistical testing that adjusts for confounding variables is necessary before drawing inferences; especially prior to designing new interventions. The dashboard is limited by the completeness and accuracy of the underlying EHR data. Demographic information, from which the categorical groupings are derived, is entered at registration by department registrars and can be edited by patients online. This process may introduce errors or selection bias in the underlying data. Finally, outcome variables we selected to present to dashboard users were already collected by our quality monitoring. While this approach is pragmatic, it may introduce a reporting bias. Other outcomes that we do not collect may better reflect health care disparities of interest.
CONCLUSION
We utilized existing quality improvement infrastructure to build a dashboard that allows for the exploration of disparities in ED care that is accessible to learners. Future directions include using these data to drive novel educational interventions, refine explanatory hypotheses on ED disparities, understand root causes, and measure both the impact of educational interventions on learners and the overall program evaluation.
ACKNOWLEDGMENTS
The authors acknowledge and thank the Massey Foundation for its generous support of Emergency Critical Care research at the University of Michigan.
CONFLICTS OF INTEREST
The authors have no potential conflicts to disclose.
AUTHOR CONTRIBUTIONS
Ryan E. Tsuchida, Adrianne N. Haggins, Marcia Perry, and Christopher M. Fung were the primary writers of the manuscript. Christopher M. Fung was the primary designer of the dashboard. Chiu-Mei Chen was the primary data analyst. Ryan E. Tsuchida and Christopher M. Fung proposed the initial concept of this study and all listed authors contributed substantially to the design of this study, selection of variables, and views on the dashboard. All listed authors participated in editing the manuscript. Christopher M. Fung supervised all aspects of study design, data collection, analysis, and manuscript preparation.