The Case of a 67-Year-Old Man With Memory Difficulties and Altered Sleep
InterACTN Case #45: Available: https://interactn.org/2025/03/04/case-45-the-case-of-a-67-year-old-man-with-memory-difficulties-and-altered-sleep/.
Funding: The authors received no specific funding for this work.
1 Summary of Case
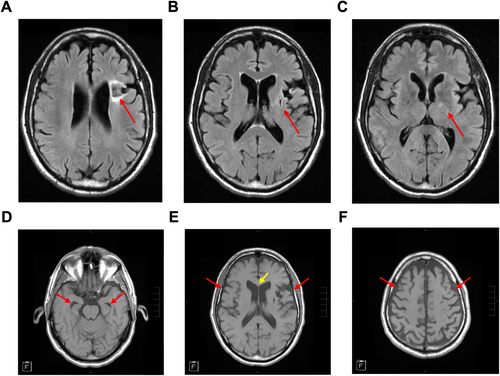
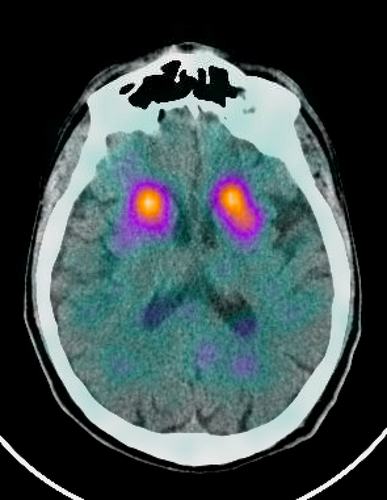
A 67-year-old man presents for evaluation of several years of memory and word-finding difficulties. During this time, he has also had issues with inattentiveness and mood changes including increased anxiety and apathy. Additional history includes 2 years of sleeping problems involving knocking over items and “fighting with his wife” as well as constipation and erectile dysfunction. His past medical history was significant for traumatic brain injury as a result of playing football in high school and college. On neurological exam, the patient was noted to have mildly increased tone in both arms and mild cogwheel rigidity. Neuropsychological testing was consistent with an amnestic disorder with multidomain difficulties. MRI brain demonstrated an old infarct and associated myelomalacia in the left basal ganglia and adjacent anterior parietal white matter as well as a cavum septum pellucidum. Additional neuroimaging included a DaT scan, which showed normal basal ganglia uptake, and a PET/CT brain that demonstrated decreased cortical glucose metabolism in the bilateral parietotemporal lobes. CSF studies demonstrated low Aβ42 and normal phospho-tau levels. In this case study, we discuss the clinical diagnosis as well as the approach to evaluating the underlying causes and management of this patient's neurocognitive disorder.
2 Diagnosis
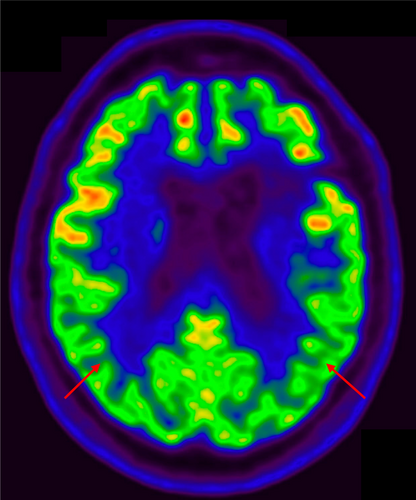
Mild major neurocognitive disorder due to mixed neurodegenerative (Figure 1) and cerebrovascular disease (Figure 2). Negative DaT scan ruled out Lewy body disease (Figure 3).
3 Take-Home Points
- Clinical diagnosis of Alzheimer's disease is currently based on the AT(N) system in which each letter represents a different AD biomarker (A = amyloid β, T = tau, (N) = neurodegeneration or neuronal injury) [1].
- An individual with a positive amyloid β biomarker, either through low CSF Aβ42 levels or a positive amyloid PET, is categorized as having a biomarker profile on the Alzheimer's disease continuum [2].
- The main pharmacologic therapies for Alzheimer's disease include cholinesterase inhibitors and anti-NMDA receptor modulators, although neither affects long-term disease progression [3]. Amyloid β-targeting monoclonal antibody therapies, such as lecanemab, have recently shown promise in slowing cognitive decline in patients with mild AD and amyloid pathology [4].
- The basal ganglia is a subcortical region that is an important mediator of motor control and nonmotor functions, including motivated behaviors. Lesions in the basal ganglia can have variable presentations, from personality changes such as apathy to parkinsonism and REM behavior disorder [5].
Author Contributions
The authors take full responsibility for this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data for this study are available upon official request.




