The case of an 85-year-old woman with subacute onset of bilateral chorea
interACTN Case #39: Available: https://interactn.org/2024/03/25/case-39-case-of-an-85-year-old-woman-with-subacute-onset-of-bilateral-chorea/.
Summary of Case (HPI, Relevant Examination Findings, and Relevant Data)
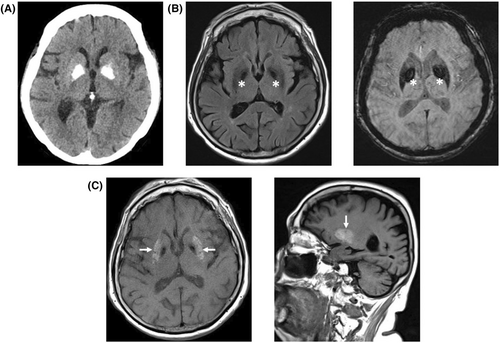
An elderly woman presented with subacute onset of chorea following a hospitalization for severe, uncontrolled diabetes, a urinary tract infection, and 6 months of depression. Her neurological examination demonstrated bilateral chorea involving the arms, legs, and jaw. MRI of the brain demonstrated bilateral T1 hyperintensity. She was diagnosed with diabetic striatopathy, also known as nonketotic hyperglycemic chorea, a rare complication of diabetes mellitus that classically causes hemichorea in the setting of very high blood glucose without ketosis. This case demonstrates typical imaging findings of diabetic striatopathy despite several atypical clinical features, including bilateral chorea, development of symptoms weeks after improvement in blood glucose, and demographics of the patient.
Diagnosis
Take-Home Points
- Diabetic striatopathy, or nonketotic hyperglycemia induced chorea, occurs in the setting of markedly elevated blood glucose.
- The mainstay of treatment is lowering of blood glucose, though, as our case indicates, chorea can start after this occurs.
- If normalization of glucose does not resolve symptoms, additional treatments include neuroleptics and benzodiazepines.
- The typical imaging finding of diabetic striatopathy is T1 hyperintensity in the putamen (Fig. 1).