Scoliosis in Friedreich's ataxia: longitudinal characterization in a large heterogeneous cohort
Funding Information
This work was funded by the Friedreich’s Ataxia Research Alliance (FARA).
Abstract
Objective
The objective of this study was to characterize the incidence and progression of scoliosis in the natural history of Friedreich’s ataxia (FRDA) and document the factors leading to the requirement for corrective surgery.
Methods
Data on the prevalence of scoliosis and scoliosis surgery from up to 17 years of follow-up collected during a large natural history study in FRDA (1116 patients at 4928 visits) were summarized descriptively and subjected to time to event analyses.
Results
Well over 90% of early or typical FRDA patients (as determined by age of onset) developed intermediate to severe scoliosis, while patients with a later onset (>14 years) had no or much lower prevalence of scoliosis. Diagnosis of scoliosis occurs during the onset of ataxia and in rare cases even prior to that. Major progression follows throughout the growth phase and puberty, leading to the need for surgical intervention in more than 50% of individuals in the most severe subgroup. The youngest patients appear to delay surgery until the end of the growth period, leading to further progression before surgical intervention. Age of onset of FRDA before or after reaching 15 years sharply separated severe and relatively mild incidence and progression of scoliosis.
Interpretation
Scoliosis is an important comorbidity of FRDA. Our comprehensive documentation of scoliosis progression in this natural history study provides a baseline for comparison as novel treatments become available.
Introduction
Friedreich's ataxia (FRDA) is an autosomal recessive disorder associated with progressive ataxia, cardiomyopathy, scoliosis, diabetes, vision, and hearing difficulties.1 In 96% of individuals, FRDA is caused by homozygous expanded guanine–adenine–adenine (GAA) repeats in the FXN gene, resulting in decreased transcription of FXN and lower expression of the protein frataxin. The length of the shorter GAA repeat correlates with measures of disease severity, including age of onset, speed of progression, and level of frataxin. Decreased mature frataxin levels inhibit the functioning of mitochondrial iron–sulfur cluster-containing enzymes and the ability of cells to produce ATP2, 3; thus, mitochondrial dysfunction is a pathophysiologic mechanism in FRDA. This leads to loss of specific neuronal systems, including the large dorsal root ganglion neurons, the dorsal spinocerebellar tracts, the dentate nuclei, and later the corticospinal tracts.
While all patients with FRDA have neurological dysfunction and cardiomyopathy is the leading cause of death, scoliosis is the most common non-neurological first symptom of the disease and by evolving opinion likely precedes neurological onset in many cases.4 In general, management of scoliosis in FRDA is similar to other neuromuscular etiologies despite its unique neuroanatomical features, and it is unclear that the exact mechanism is the same in FRDA and other neurological disorders. In case series, the prevalence of scoliosis in FRDA varies but is frequently greater than 50% and commonly requires surgical intervention.5-7 These observations vary among series and usually reflect single sites with a moderate number of patients (20–100).8-11 As in other neuromuscular diseases, in early and typical onset FA progressive deformity can lead to unacceptable truncal shift affecting standing balance and sitting positioning, including in wheelchair users (for a specific review, see Murphy12). Corrective surgery is offered to improve upright posture and quality of sitting, as well as to decrease back pain. Surgical intervention can also ameliorate potential long-term cardiopulmonary dysfunction. A relationship between spinal surgery and loss of ambulation has been discussed,11 including the type and extend of the surgery,10 but a chronological analysis based on a large data set has not been reported.
In the present work, we have used data from the Friedreich Ataxia Clinical Outcome Measure Study (FACOMS, NCT03090789), a continuously recruiting natural history study with >1100 patients across 15 sites to describe the presence and progression of scoliosis, as well as the incidence of surgical intervention. Specifically, we also document the relationship of scoliosis with disease features (age, sex, and GAA repeat length) and the major disease milestone in FRDA, loss of ambulation (LoA), and how such disease related features predict likelihood of the need for surgery in FRDA.
Patients and Methods
Patients and variables
The FACOMS study has been approved by the appropriate ethics committees and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. FACOMS has minimal inclusion criteria (age 4–80 years, genetically confirmed diagnosis of FRDA), and results have been widely published.13-15 In this work, we included all patients who reported at least age of disease onset and had information available on Functional Disability Score, FDS,16 and documented presence or absence of scoliosis. Data were included through 7 July 2020, comprising 1114 patients at 4922 visits (94% of all FACOMS visits) from 15 sites. Patients are generally seen yearly, with scoliosis assessed at every visit; variables included presence or absence of scoliosis, curvature angles (measured from X-ray or estimated), corrective surgery, and the year of surgeries (including prior to enrollment). Typical FRDA-related descriptors were used: the shorter of both GAA repeat lengths (GAA1), age of onset (assessed at the baseline visit), and the single selected item as first symptom of onset leading to diagnosis of FRDA. Loss of ambulation (LoA) was defined by the first attainment of a score of 5 in the FDS (ranging from 1 to 6), indicating full time wheelchair use. Age of LoA was defined as the midpoint between the last ambulatory and the first nonambulatory visit. We also used the modified Friedreich's Ataxia Rating Scale (mFARS) Score17 for a more detailed description of the patient’s neurological status. This included the seminal FARS E7 item that quantifies gait (possible scores 1–5, with 5 being nonambulatory).
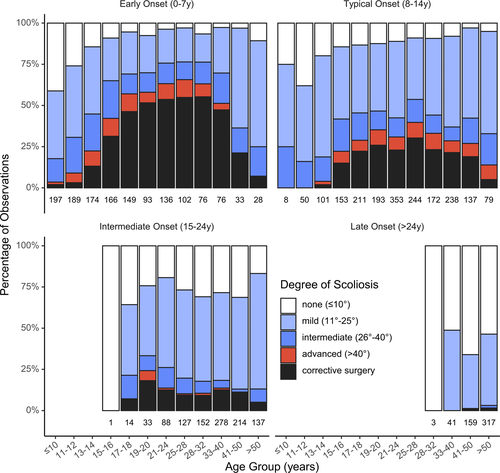
Statistical methods
Based on previously used classifications,9, 18, 19 we stratified patients into four groups based on age of disease onset: 0–7 years (early), 8–14 years (typical), 15–24 years (intermediate), and >24 years (late onset FRDA, LOFA). While to some extent historical and difficult to justify statistically, this classification has been proven useful in understanding the continuum of FRDA severities. The earliest threshold (7/8 years) has so far not been widely used. The scoliosis data described above were reviewed and manually consolidated. Patient scoliosis status at each visit was categorized as none (<10°), mild (10–19°), intermediate (20–40°), and advanced (>40°) scoliosis. Few angles were measured following surgical intervention, and data amount and quality did not allow assessing improvement of angles. Therefore, postsurgery was rated as a separate category. For descriptive analyses (Fig. 1), missing curvature angles were imputed using last observation carried forward (in case of present scoliosis) or set to <10° when scoliosis was absent.
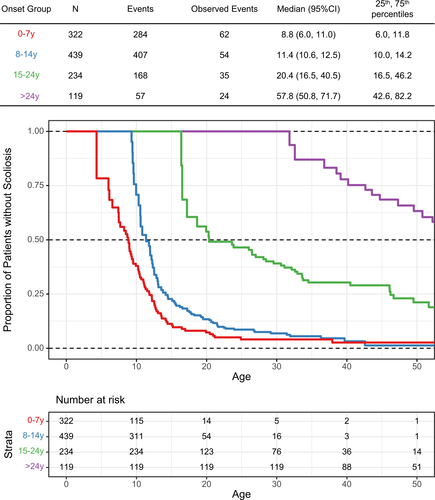
The age at related events (scoliosis, corrective surgery, and LoA) was analyzed using Kaplan Meier methods stratified by age of onset group. However, as a high proportion of subjects presented with significant scoliosis, the use of Kaplan Meier estimates can lead to heavy truncation bias.20, 21 For age at scoliosis onset, we therefore used an alternative algorithm, the Turnbull estimator,22, 23 a method that can deliver reliable estimates in these type of situations.24 For selected analyses, we used Cox proportional hazards models to assess statistical differences between subgroups.
Results
Demographics
Demographic and genetic features of the cohort have been presented previously; maximum follow-up time was 17 years, with the median times being very similar over all onset groups, for example, 4 years in the early onset group (Table 1). In early (age 0–7 years) and typical onset (8–14 years) FRDA, 69% and 80% of patients presented with scoliosis, and 88% and 93% had developed it by their most recent evaluation. In intermediate onset FRDA (15–24 years), 57% presented with scoliosis, and 72% developed it during follow-up. In LOFA (onset > 24 years), these numbers were 28% at first visit and 48% during follow-up. This sharp decrease by onset group was also reflected in patients presenting with or requiring corrective surgery over the study (Table 1). Scoliosis was overall the second-most frequent first symptom at diagnosis of FRDA. This proportion was higher in typical (11%) or intermediate onset FRDA (6%), compared to early onset FRDA (3%). The actual onset of scoliosis is difficult to determine and was not recorded in FACOMS; however, 11 patients reported corrective scoliosis surgery prior to the onset of the first symptoms of FRDA.
| Age of onset group | 0–7 years (early) | 8–14 years (typical) | 15–24 years (intermediate) | >24 years (late) |
|---|---|---|---|---|
| N | 322 | 439 | 234 | 119 |
| Sex (male) | 170 (53) | 217 (49) | 113 (48) | 48 (40) |
| Age of onset | 5 [4, 6] | 11 [9, 13] | 18 [16, 20] | 32 [28, 40] |
| Repeat length (shorter)a | 790 [700, 895] | 705 [600, 820] | 500 [373, 630] | 250 [136, 360] |
| Point mutation | 28 (9) | 16 (4) | 10 (4) | 3 (3) |
| Status at enrollment | ||||
| Age | 12 [9, 18] | 19 [15, 27] | 30 [24, 39] | 49 [43, 57] |
| Scoliosis | 222 (69) | 353 (80) | 133 (57) | 33 (28) |
| Corrective surgery | 57 (18) | 72 (16) | 17 (7) | 2 (2) |
| Status at last follow-up | ||||
| Age | 18 [14, 25] | 24 [19, 33] | 36 [29, 44] | 53 [47, 63] |
| Scoliosis | 284 (88) | 407 (93) | 168 (72) | 57 (48) |
| Corrective surgery | 115 (36) | 102 (23) | 20 (9) | 3 (3) |
| Follow-up (years) | 4 [1, 8] | 3 [1, 8] | 4 [1, 9] | 4 [0, 8] |
| Follow-up (visits) | 4 [2, 7] | 4 [2, 6] | 3 [2, 6] | 3 [1, 6] |
| First symptom of FAb | ||||
| Scoliosis | 11 (3) | 47 (11) | 13 (6) | 0 (0) |
| Balance/ataxia | 272 (85) | 363 (83) | 205 (88) | 113 (97) |
| Cardiomyopathy | 17 (5) | 9 (2) | 1 (0) | 0 (0) |
| Diabetes | 1 (0) | 0 (0) | 0 (0) | 0 (0) |
| Other | 18 (6) | 18 (4) | 13 (6) | 4 (3) |
- N (%) or median [IQR].
- a GAA1, missing for n = 58 (excluding point mutations).
- b Missing for n = 11.
Prevalence of scoliosis and degree of curvature
The proportion of patients with severe scoliosis (Cobb angle > 40°) and who had scoliosis surgery increased with age, particularly in those with early and typical onset (Fig. 1). While in the early onset group, worsening continued into the third decade, progression generally slowed after patients finished growth and reached adulthood. In later age ranges (e.g., >32 years for onset 0–7 years), the proportion of patients with milder scoliosis increased, most likely attributable to overrepresentation of milder phenotypes in this part of the sample (selection bias).
Time-to-event analyses for time to scoliosis (Fig. 2) are complicated by a large number of left-censored observations, corresponding to patients diagnosed with scoliosis at enrollment into FACOMS or FRDA diagnosis, respectively. This results in steep drop in the early part of the Turnbull curves that is otherwise difficult to interpret. In general, however, the estimates paralleled the descriptive results. In the early and typical onset groups, 50% of patients developed scoliosis by the age of 8.8 (95% CI 6.0, 11.8 years) and 11.4 years (95% CI 10.6, 12.5 years), respectively. In contrast, in the intermediate and late onset groups, the median age at onset of scoliosis was 20.4 (95% CI 16.5, 40.5 years) and 57.8 years (95% CI 50.8, 71.7 years), respectively. From the same analysis, it can be estimated that at age 30 years and by onset group, 96%, 93%, 61%, and 0% of patients with FA will be diagnosed with scoliosis.
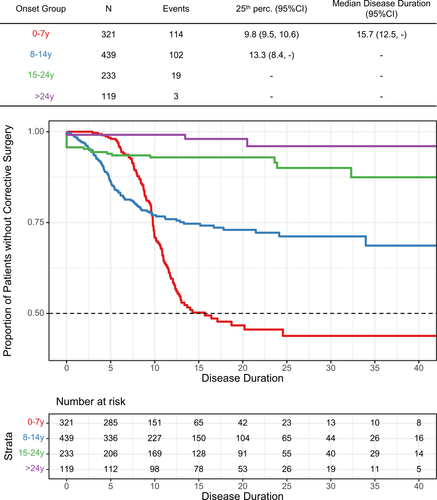
Age and disease duration at scoliosis surgery
The youngest age for scoliosis surgery was at 7 years, although surgery before 10 years was the exception (n = 4). The steepness of the Kaplan Meier curve indicates that scoliosis surgery was most commonly performed between ages 12 and 16 years in the early onset group, with the 25th percentile reached at 14.7 years (95% CI 14.3, 15.5) (Fig. 3). Median age was 19.4 years, and in total, just over 50% of patients eventually had surgery. The group with typical onset reached the 25th percentile at 25.3 years (95% CI 17.8, -), and less than 30% overall had surgery by age 40 years. Scoliosis surgery was performed after 20 years of age in only 28 of 240 cases (12%) and was uncommon in intermediate and late onset patients (23 of 353 patients, 7%).
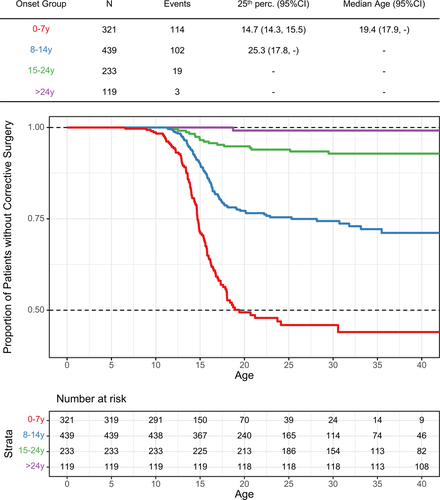
By using the Kaplan Meier estimator, it can be predicted that at age 40 years, 55%, 29%, 7%, and 1% of patients in each onset group had undergone scoliosis surgery. With the early onset group as reference, hazard ratios for undergoing scoliosis surgery were 0.37 (95% CI 0.29, 0.49), 0.10 (95% CI 0.06, 0.16), and 0.02 (95% CI 0.01, 0.08) for typical-, intermediate-, and late-onset patients, respectively (Cox proportional hazard model). Combining the two early onset groups (14 years of age or earlier) versus later onset, the hazard ratio for scoliosis surgery was 0.13 (95% CI 0.08, 0.20).
An interesting result evolved from the analysis using disease duration as the temporal variable (Fig. 4). In those with typical onset (blue curve), the first surgeries were performed just after disease onset, and the proportion steadily increased with disease duration. In comparison to that, surgeries in the early onset group start with a delay of 3–4 years, and the group proportion increased markedly only after 6 years. The cumulative group proportions of patients with surgery cross at the 78th percentile, corresponding to a disease duration of 9.6 years. Of note, in the intermediate and late onset groups, 10 patients (9 + 1) had scoliosis surgery prior to the first symptoms of FRDA. For the purpose of plotting these cases, their times were set to 0 in Figure 4 (green line).
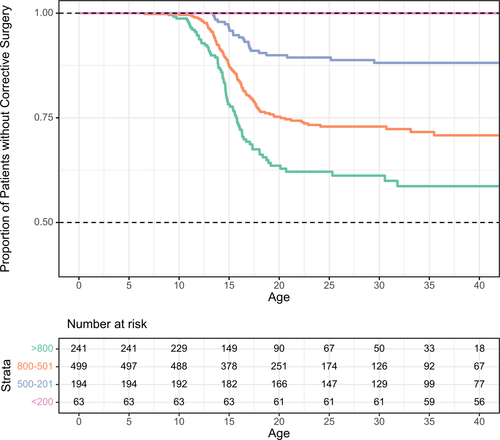
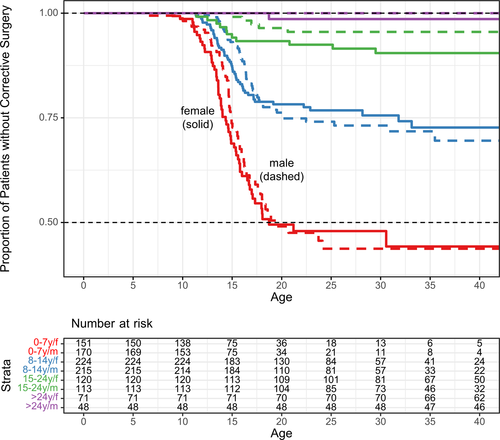
Additional analyses for age at corrective surgery were conducted for subgroups of the shorter GAA repeat length (Fig. 5) and sex (Fig. 6). As expected, longer GAA repeat lengths correlated with earlier age of scoliosis surgery (patients compound heterozygous for a FXN GAA repeat and carrying a point mutation or deletion were excluded from this analysis). For the analysis by sex, Kaplan Meier estimates indicated slightly earlier surgeries in females, especially during the growth period (Fig. 6). The hazard ratio for males versus females, adjusted for grouped age of onset, was 0.91 (95% CI 0.70, 1.17) and did not indicate a significant difference.
Scoliosis surgery and LoA
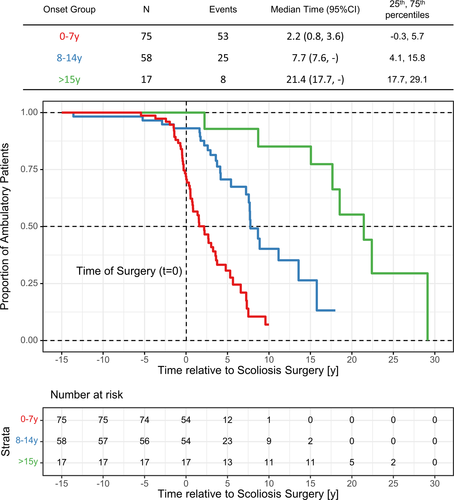
The relationship of LoA and scoliosis surgery was investigated in the subgroup where surgery was performed during follow-up time or when prior age of surgery was documented (n = 237). Patients who were nonambulant at enrollment were excluded (n = 87). In the remaining 150 patients, the two later onset groups (15–25 and >24 years) were combined (Table 2, only one patient had an onset of 24 years).
| Age of onset | 0–7 years (early) | 8–14 years (typical) | >14 years (intermediate and late) | Total |
|---|---|---|---|---|
| N | 75 | 58 | 17 | 150 |
| First event | ||||
| Corrective surgery | 42 (56.0) | 54 (93.1) | 17 (100.0) | 113 (75.3) |
| LoA and surgery coincidental | 25 (33.3) | 0 (0.0) | 0 (0.0) | 25 (16.7) |
| Loss of ambulation | 8 (10.7) | 4 (6.9) | 0 (0.0) | 12 (8.0) |
| Ambulatory at last visit | 22 (29.3) | 33 (56.9) | 9 (52.9) | 64 (42.7) |
| Time from surgery to LoA | 2.2 (0.8, 3.6) | 7.7 (7.6, -) | 21.4 (17.7, -) | 6.6 (3.7, 7.7) |
| Efficacy at surgery (% available) | 59 (78.7) | 37 (63.8) | 4 (23.5) | 100 (66.7) |
| mFARS | 53.8 (11.2) | 41.8 (13.8) | 38.3 (8.3) | 48.7 (13.5) |
| FARS E7 (gait) | 3.6 (1.4) | 2.2 (1.4) | 2.5 (1.3) | 3.0 (1.5) |
- N (%) or mean (SD).
- a Kaplan Meier estimates (95% CI); see also Figure 7.
Our definition of attaining an FDS stage 5 for the first time permits to statistically cope with LoA in the context of natural history data. However, the process of becoming nonambulant is indeed spanning several years from the first use of walking aids to finally becoming fully wheelchair dependent. In addition, only the year of surgery is recorded in FACOMS, and surgeries do not necessarily take place in temporal proximity to a FACOMS visit. Accordingly, borderline cases were manually investigated, and if the order of events could not be determined from the data, LoA and scoliosis surgery were treated as coincident and potentially related.
This was the case for 25 patients (16.7%, Table 2). In most cases however, scoliosis surgery was performed on subjects that were ambulant and had at least one ambulatory visit postsurgery (N = 113, 75.3%). Few patients were operated on post-LoA (N = 12, 8.0%), and all of those individuals were in the two earlier onset groups.
Median times to LoA postscoliosis surgery determined by Kaplan Meier analysis were 2.2, 7.7, and 21.4 years per onset group, respectively (Fig. 7). mFARS and FARS E7 (gait) scores at time of surgery (i.e., assessed within one year) were available for 66.7% of patients. These scores coinciding with scoliosis surgery were higher in the earlier onset groups, demonstrating that these patients had progressed further in their disease at the time of surgery.
Discussion
We have summarized the incidence and temporal progression of scoliosis in a large natural history study of FRDA, as well as the requirement for corrective spinal surgery and its relation to LoA. Consistent with earlier reports,13, 25 indicators of genetic disease severity (age of onset and GAA1) correlated with the severity of scoliosis and further progression of the disease. Prevalence of scoliosis varied in earlier studies, for example, 61%,9 63%,11 or 71%10 in cohorts most reminiscent of typical onset FRDA, while numbers were lower for LOFA patients groups, for example, 22%.9 However, such reports frequently use inconsistent classifications of clinical parameters of FRDA such as age of onset and/or combine largely heterogeneous groups.
Our data allow for a more comprehensive overview and clarity about scoliosis in subsets of patients. Well over 90% of patients with age of onset prior to 15 years of age develop scoliosis, most of them at early ages. At a cutoff age of 30 years, 61% in the intermediate onset group (15–24 years) and 0% in the LOFA group have scoliosis. A more precise prevalence especially at early ages and severe disease is difficult to estimate retrospectively, as most patients are presenting with scoliosis.
Diagnosis of scoliosis often coincides with the diagnosis of FRDA, though less so in early onset FRDA (0–7 years of age). In this group, frequently diagnosed prior to the pubertal growth spurt that leads to scoliosis complications, early motor symptoms are overwhelming. Typical onset patients (8–14 years), however, are diagnosed during or after the intensive growth period making scoliosis a more relevant factor during diagnosis of FRDA. Notably, in this group were several cases in which the FRDA diagnosis was overlooked in spite of existing scoliosis requiring corrective surgery. Alternatively, identification of scoliosis might be less systematic in earlier onset subjects, based on less perceived need for urgent intervention and the reluctance for prolonged evaluation in the youngest children.
The proportion of patients undergoing scoliosis surgery declined substantially with later age at onset, from 55% in early and 25% in typical onset patients to 7% and 1% of patients with intermediate and late onset. Median age at surgery in the most severe subgroup (onset 0–7 years) was 19.4 years, which seems high when compared to 15.4 years reported by Simon.10 This contrast can be attributed to methodology (mean age vs. Kaplan Meier will underestimate the true mean in this subgroup) and stratification (severity of scoliosis vs. age of onset), even if our cohort included more severe patients, few of which will likely require surgery in the future. Apart from a few early cases, surgery was performed during or shortly after finishing the growth period. In all groups, relatively few surgical interventions occur in the third decade of life, by which time progression of spinal deformity is expected to have stabilized. As expected, the shorter repeat length (GAA1) differentiated patients regarding the need for corrective surgery, if not as sharply as age of onset.
The analysis of disease duration at surgery revealed a delay in undergoing surgery in the early onset group (0–7 years). This means that although these patients experience the fastest neurological progression and, by trend, the most severe scoliosis, surgeries are conducted with a marked delay compared to those with typical age of onset. Potentially waiting for the end of the growth period, these patients progress further neurologically and are more advanced when they are finally operated on. As a result, they are more likely to lose ambulation at the same time or shortly thereafter. This result, together with the overwhelming proportion of patients walking for many years after spinal surgery (in later onset groups), renders a causal relationship of surgery and LoA highly unlikely.
Adolescent idiopathic scoliosis presents earlier in females, who also dominate the group of patients with severe deformities,26 an aspect that has not been systematically investigated in neuromuscular disease.12 Some disease specific reports show that females by trend are more affected, for example, in cerebral palsy27 but also in FRDA.8 But comparing subgroups in rare disease often fails to bear out statistically significant effects, due to low patient numbers. Relevant differences can still be found, as, for example, in proximal spinal muscular atrophy type II versus IIIa.28 Much alike, our descriptive result showed a trend for females undergoing surgery at a slightly younger age than males especially during the growth period, but statistically, there was no difference.
Overall, an age of onset before or after 15 years sharply divided groups by probability of developing scoliosis and likelihood of progression leading to surgery. Since typical FRDA is usually diagnosed 3–4 years after onset,4, 24 this concurs with presentation and diagnosis during the growth period versus after finishing it. On the other hand, even in the genetically most severe, early-onset patients only about 50% eventually require surgery. In addition, generally milder phenotypes develop scoliosis to some degree with some requiring surgery. Few patients with LOFA have scoliosis and related complications. Thus, there are considerations beyond simply diagnostic age of onset that influence presence and progression of scoliosis.
One limitation of our study is the likely imprecise estimates of early prevalence of scoliosis in FRDA. This is tied to interaction of FRDA diagnosis and the type of first symptoms recorded. A more comprehensive documentation of patients’ status at diagnosis and their early symptoms could help improve this situation.4 In addition, the early anthropomorphics (particularly height) are not sufficiently detailed to allow an analysis on how height influences management decisions in the FRDA population.
Conclusions
In summary, we have provided a comprehensive overview of scoliosis in FRDA, based on clinical severity and associated clinical parameters. With continued review of the present cohort, other features beyond genotype and age of onset may be identifiable as modifiers for the importance of scoliosis in FRDA.
Acknowledgment
This work was funded by the Friedreich’s Ataxia Research alliance (FARA).
Author Contributions
Christian Rummey conceived and designed the work, analyzed and interpreted the data, and drafted the article. John M Flynn conceived and designed the work and analyzed and interpreted the data. Louise A. Corben, Martin B. Delatycki, George Wilmot, Sub H. Subramony, Khalaf Bushara, Antoine Duquette, Christopher M. Gomez, J. Chad Hoyle, Richard Roxburgh, Lauren Seeberger, Grace Yoon, Katherine D. Mathews, Theresa Zesiewicz, and Susan Perlman revised the article critically and collected the data. David R. Lynch conceived and designed the work, analyzed and interpreted the data, drafted the article, and collected the data.
Conflict of Interest
The authors report no relevant disclosures.