Ultrasonographic and clinical appearance of a 22-week-old fetus with Brachmann-de Lange syndrome
Abstract
The diagnosis Brachmann-de Lange or Cornelia-de Lange syndrome is based on the characteristic facial appearance and other malformations. Prenatal ultrasonographic diagnosis has been made occasionally usually confirmed by clinical photographs of third trimester fetuses with distinctly recognizable hair anomalies (synophrys, low anterior and posterior hairlines, and hypertrichosis). However, at 22 weeks of gestation, these highly characteristic signs fail to support the clinical diagnosis. We report on pre- and post-natal findings in a 22-week-old female fetus with Brachmann-de Lange syndrome. The facial Gestalt was already characteristic and the associated upper limb malformations (bilateral monodactyly and ulnar agenesis) supported the diagnosis. The prenatal ultrasound images demonstrated a grossly abnormal facial profile (a protruding and overhanging upper lip and severe retrognathia) highly suggestive of Brachmann-de Lange syndrome. The recurrence risk is estimated &#1%. The recognition of Brachmann-de Lange syndrome in second trimester fetuses is essential for genetic counselling and reassurance of parents contemplating future reproduction. © 2001 Wiley-Liss, Inc.
INTRODUCTION
Brachmann-de Lange syndrome (BDLS, MIM 122470) occurs approximately once in every 10,000 live births [Opitz, 1985]. The diagnosis is based on the characteristic facial appearance: microbrachycephaly, a low frontal hairline, synophrys, anteverted nostrils, long philtrum, thin lips, downturned corners of the mouth, retrognathia and apparently low-set ears, prenatal and postnatal growth retardation, a low-pitched voice, hypertrichosis, upper limb malformations, and delay of psychomotor development. The upper limb defects in BDLS are variable, ranging from almost normal limbs to peromelia, Malformations of inner organs such as heart defects and a diaphragmatic hernia may also occur. Lower limb involvement is rare [for review, see Jackson et al., 1993]. BDLS usually occurs sporadically. Therefore, the diagnosis usually depends on the recognition of the clinical characteristics of the affected fetus or child itself. Affected sibs are rare, suggesting autosomal dominant inheritance and occasional germline mosaicism.
Several accounts dealing with prenatal diagnosis of BDLS are available. Manouvrier et al. [1996] published clinical photographs of affected fetuses at 33, 33, and 34 weeks of gestation and reviewed several further reports on BDLS patients older than 32 weeks. At that developmental period, the characteristic hair anomalies such as a low frontal hairline, synophrys, and hypertrichosis were distinctly recognizable However, in second trimester fetuses, these findings fail to support the diagnosis. The clinical diagnosis must therefore be based on the remaining characteristics of the facial gestalt and on associated malformations.
CLINICAL REPORT
We recently diagnosed Brachmann-de Lange syndrome in a 22-week-old female fetus, the second child of a young, healthy non-consanguineous German couple. The family history was non-contributory. The mother, a 26-year-old gravida 2, para 1 woman was referred for targeted ultrasound examination at 22/+4 weeks of gestation. High-resolution ultrasound (Logiq 700, Fm. GE, Soling) demonstrated severe bilateral upper limb deficiency agenesis of one forearm bone and monodactyly). The facial profile was markedly abnormal with a protruding and overhanging upper lip in combination with severe retrognathia (Fig. 1). There was also cerebellar vermis hypoplasia. Except for the femoral length (31 mm, below the 5th centile), the fetal measurements were normal for gestational age. The parents were informed about the poor prognosis and chose to terminate (carried out at 22 weeks of gestation).
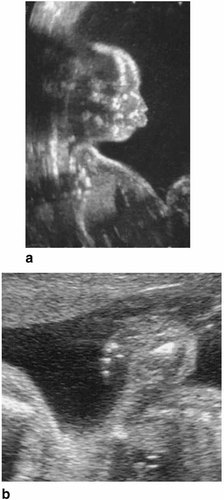
Prenatal ultrasound images obtained at 22 weeks of gestation: Note the protruding upper lip with a long nasolabial distance and severe microretrognathia (a). The hands were monodactylous (b).
On examination, the female fetus had a peculiar shape of the supraorbital ridges, hypertelorism, a short nose with a depressed nasal bridge and anteverted nostrils, a protruding upper lip with poorly defined long philtrum, downturned corners of mouth, marked microretrognathia, apparently low-set malformed ears (Fig. 2), and cleft palate. Postmortem radiography demonstrated bilateral monodactylous upper limbs containing a humerus, a hypoplastic radius, and the thumb. Antecubital webs fixed the forearms in a flexed position. No malformations of the esophagus, heart, diaphragm, or urinary tract were discernible. The karyotype of fetal blood lymphocytes was normal (46,XX) at a 550 bands level. No structural anomalies of chromosome 3 were found despite meticulous examination.
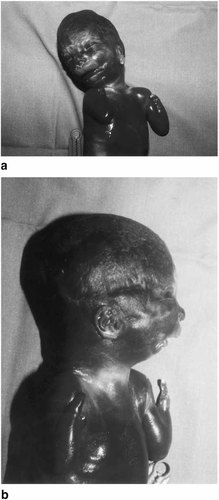
Clinical photographs taken at 22 week of gestation. The fetal face is abnormal showing hypertelorism, a depressed nasal bridge, a small bulging nose with anteverted nostrils, protrusion of the whole upper lip, a long poorly defined philtrum, and severe retrognathia (a). The ear helices are low-set and dysplastic (b). Sparse eyebrows are present, but a synophrys is not (yet) discernible. Note the asymmetric upper limb deficiencies (bilateral ulnar agenesis antecubital webs and monodactyly).
DISCUSSION
Several third trimester BDLS fetuses have been described [see Bruner and Hisa, 1990; Goolsby et al., 1995; Manouvrier et al., 1996; Ackerman and Gilbert-Barness, 1997; Ranzini et al., 1997; Boog et al., 1999]. In those reports, the diagnosis is usually backed up by clinical photographs of the face showing the typical hair anomalies (synophrys, a low frontal hairline, hypertrichosis). In spite of the absence of these armolies, the facial gestalt of this 22-week-old fetus was already characteristic and the ultrasonographic face was suggestive of BDLS. However, it is uncertain, whether this is generally so. Aitken et al. [1999] reviewed second trimester facial profiles of children with postnatally diagnosed BDLS and found only one characteristic profile in 11 cases. This profile, obtained at 19 weeks of gestation was described as “a very small mandible with overhanging upper lip” [Aitken et al., 1999]. In the fetus reported here, the ultrasonographic facial profile fits this description. However, it is of note, that this fetus had a cleft palate, a rare aromaly in BDLS. It seems likely that this cleft is secondary to the likewise unusually severe mandibular hypoplasia (Pierre-Robin sequence) in this particular case, which markedly contributed to the grossly abnormal facial profile. In fetuses suspected of BDLS, measurement of second-trimester maternal serum pregnancy-associated plasma protein-A (PAPP-A) may be of value. For some as yet unexplained reason, PAPP-A levels tend to be lower in fetal BDLS [Aitken et al., 1999]. Furthermore, karyotyping for the exclusion of dup(3q) syndrome is essential in such fetuses, because patients with this cytogenetic anomaly display a facial Gestalt similar to that of BDLS fetuses [see Beck and Mikkelsen, 1981].
The most impressive BDLS anomalies are the upper limb defects, but only 27% of BDLS patients have grossly malformed upper limbs [Jackson et al., 1993]. If present, they tend to affect mainly the ulnar rays [Wiedemann and Kunze, 1995]. Concerning the diagnostic value of severe limb malformations in BDLS in general, Jackson et al. [1993] commented, “although striking when present, these are only seen in cases where other manifestations are similarly severe, so they do not contribute significantly to the diagnostic process.” Thus, fetuses with severe upper limb deficiencies can also be expected to display the most obvious facial changes, whereas the prental ultrasonographic diagnosis of BDLS in fetuses with a milder phenotype is presumably very difficult or even impossible. In fact, most of the available reports on prenatal findings refer to fetuses with severe upper limb malformations and/or a diaphragmatic hernia [Goolsby et al., 1995; Manouvrier et al., 1996; Ackerman and Gilbert-Barness, 1997; Ranzini et al., 1997; Boog et al., 1999]. Although the lower limbs are usually unaffected in BDLS, the mild femoral shortness observed in this fetus is a non-specific sign of this syndrome; Kliewer et al. [1993] found relatively short femora (less than 90% of the expected length) in 4 of 11 subsequently diagnosed fetuses with BDLS.
We conclude that some second trimester fetuses with BDLS can be recognized ultrasonographically or by postmortem clinical examination. In their review of 310 patients and their family histories, Jackson et al. [1993] calculated the risk of recurrence in sib to be less than 1%. Therefore the clinical recognition of BDLS is essential for genetic counselling and reassurance of affected families contemplating future reproduction.
Acknowledgements
We thank Ms. Alexa Nieschlag for her editorial comments on the manuscript.




